老年股骨粗隆间骨折手术治疗效果及预后影响因素分析
傅升培 黄祥文 李泽添
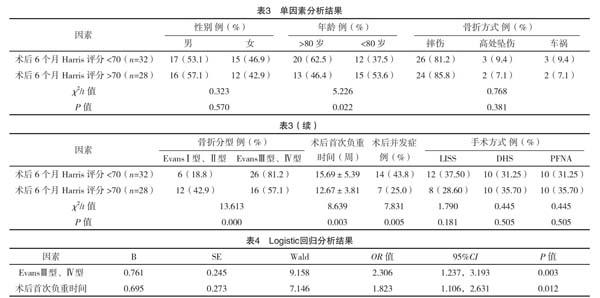
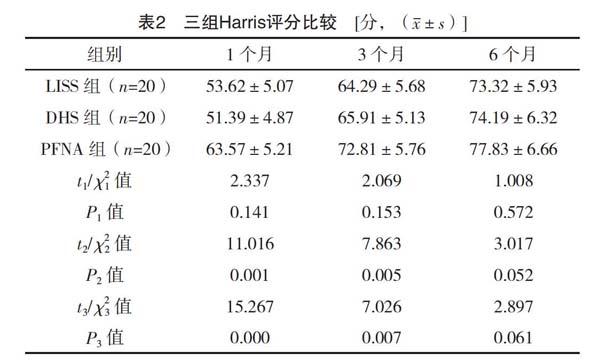
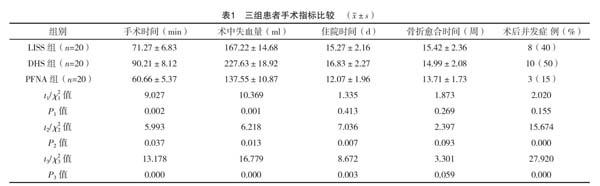
【摘要】 目的:探討老年股骨粗隆间骨折不同手术治疗的效果,分析患者预后相关影响因素。方法:收集2018年5月-2019年5月笔者所在医院治疗的老年股骨粗隆间骨折患者,按手术方式微创内固定系统(LISS)、滑动加压动力髋螺钉(DHS)及股骨近端防旋髓内钉(PFNA)分为三组,每组20例。比较三组手术相关指标(手术时间、术中失血量、骨折愈合时间、住院时间及术后并发症等),并采用Harris评分法评价患者1、3、6个月的髋关节功能。并对比分析Harris评分>70患者与Harris评分<70患者的基本资料,采用多元Logistic回归分析患者预后的影响因素。结果:(1)手术时间、术中失血量由高至低分别为DHS组、LISS组、PFNA组,且差异均有统计学意义(P<0.05)。PFNA组的住院时间、术后并发症率均显著少于LISS组与DHS组(P<0.05),LIIS组与DHS组差异无统计学意义(P>0.05);LISS组患者骨折愈合时间稍长于DHS及PFNA组,但三组差异无统计学意义(P>0.05)。(2)PFNA组术后1个月、3个月Harris评分显著优于LISS组及DHS组(P<0.05)。三组患者术后6个月Harris评分差异无统计学意义(P>0.05)。(3)Harris评分>70患者的年龄、骨折分型、术后首次负重时间、术后并发症率等与Harris评分<70患者比较,差异有统计学意义(P<0.05);Logistic分析发现骨折分型、术后首次负重时间是影响患者预后的影响因素。结论:PFNA术治疗老年股骨粗隆间骨折的效果要优于LISS术与DHS术,具有更小手术创伤、更少并发症率,对患者预后恢复效果更佳。骨折分型与术后首次负重时间是影响患者预后的影响因素。
【关键词】 老年 股骨粗隆间骨折 手术 因素
doi:10.14033/j.cnki.cfmr.2020.21.051 文献标识码 B 文章编号 1674-6805(2020)21-0-04
Analysis of the Operative Effect and Prognostic Factors of Intertrochanteric Fracture in the Elderly/FU Shengpei, HUANG Xiangwen, LI Zetian. //Chinese and Foreign Medical Research, 2020, 18(21): -126
[Abstract] Objective: To explore the operative effect and prognostic factors of intertrochanteric fracture in the elderly. Method: The elderly patients with intertrochanteric fracture of femur treated in our hospital from May 2018 to May 2019 were divided into three groups according to LISS operation, DHS operation and PFNA operation, 20 in each group. The operation related indexes (operation time, intraoperative blood loss, fracture healing time, hospitalization time and postoperative complications) were compared among the three groups. The hip joint function of patients at 1, 3 and 6 months were evaluated with Harris scoring method. The basic data of patients with Harris score>70 and patients with Harris score<70 were compared, and the influencing factors of prognosis were analyzed by multiple Logistic regression. Result: (1) The operation time and blood loss during operation from high to low were DHS group, LISS group and PFNA group respectively, and the difference was statistically significant (P<0.05). The hospitalization time and postoperative complication rate of PFNA group were significantly lower than those of LISS group and DHS group (P<0.05), but there was no significant difference between LISS group and DHS group (P>0.05). The fracture healing time of LISS group was slightly longer than that of DHS group and PFNA group, but there was no significant difference among the three groups (P>0.05). (2) The Harris score of PFNA group was significantly better than that of LISS group and DHS group after 1 month and 3 month (P<0.05). There was no significant difference in Harris score between the three groups after 6 month (P>0.05). (3)There were significant differences in age, fracture classification, time of first postoperative weight-bearing and postoperative complication rate between patients with Harris score>70 and those with Harris score<70 (P<0.05). Logistic analysis showed that fracture classification and the time of first postoperative weight-bearing were the factors influencing the prognosis of patients. Conclusion: PFNA is better than LISS and DHS in the treatment of intertrochanteric fracture of femur in the elderly. It has less surgical trauma, less complication rate and better effect on the prognosis of patients. Fracture classification and the time of first postoperative weight-bearing are the factors influencing the prognosis of patients.
[Key words] The elderly Intertrochanteric fracture Operation Influence
First-authors address: Yunan Peoples Hospital, Yunan 527199, China
老年人骨质疏松,骨强度下降,受到外伤后更易出现骨折。股骨粗隆间骨折是我国老年人常见的骨折现象,发生率高。但是由于老年人机体恢复能力差,对于手术的耐受性普遍不高,因此部分患者多采用保守治疗[1-2]。保守治疗虽然可以保证患者免受手术痛苦,但长期的卧床会影响患者髋关节功能恢复,而且会引起其他相关症状如吸入性肺炎、褥疮等。随着近年来骨科医学技术的发展,衍生出多种股骨粗隆间骨折手术方式,而且不乏发展出更适合于老年人的手术治疗方式。目前常用固定方式有微创内固定系统(less invasive stabilization system,LISS)、滑动加压动力髋螺钉(dynamic hip screw,DHS)及股骨近端防旋髓内钉(proximal femoral nail anti-rotation,PFNA)等,不过手术方式不同,手术相关指标及预后可能有所不同[3-5]。而老年人多合并各种慢性疾病,机体恢复能力相对较弱,所以选择何种手术方式需要综合考虑。本研究采用上述三种手术方式对60例老年股骨粗隆间骨折患者进行手术治疗,探讨相关手术指标,并分析影响患者预后恢复的相关因素。
1 资料与方法
1.1 一般资料
收集2018年5月-2019年5月笔者所在医院治疗的老年股骨粗隆间骨折患者共60例,纳入标准:(1)60岁<年龄<95岁;(2)受伤前患肢功能正常;(3)符合Evans分型标准;(4)配合术后早期康复训练。排除标准:(1)合并严重脏器官疾病;(2)合并恶性肿瘤;(3)合并盆骨、脊柱等骨折;(4)有沟通、认知障碍。按手术适应证和禁忌证分为LISS组、DHS组及PFNA组,每组20例。其中LISS组男女比例为10∶10,年龄62~87岁,平均(73.3±3.7)岁,其中摔伤16例,高处坠伤2例,车祸2例。
骨折分型为EvansⅠ型3例,Ⅱ型4例,Ⅲ型10例,Ⅳ型3例。DHS组男女比例12∶8,年龄63~90岁,平均(75.1±4.6)岁,其中摔伤17例,高处坠伤2例,车祸1例。骨折分型为Evans Ⅰ型2例,Ⅱ型3例,Ⅲ型11例,Ⅳ型4例。PFNA组男女比例11∶9,年龄61~89岁,平均(73.8±3.9)岁,其中摔伤17例,高处坠伤1例,车祸2例。骨折分型为EvansⅠ型3例,Ⅱ型3例,Ⅲ型11例,Ⅳ型3例。三组患者入组基本信息比较差异无统计学意义(P>0.05),具有可比性。本研究经笔者所在医院医学理论委员会批准后开展。
1.2 方法
所有患者术前均进行术前常规检查与外伤护理,待生命体征稳定后行腰硬联合麻醉或全麻,患者取仰卧位,垫高术侧,麻醉满意后采取不同手术治疗。(1)LISS组患者手术方式:术侧髋关节股骨粗隆转角外侧为手术切口,切口宽度4~6 cm。皮肤组织切开后对术区肌肉组织进行分离,暴露术区,在C型臂透视下进行骨折复位操作。选择尺寸合适的LISS钢板倒置插入股骨,检查LISS钢板与股骨的贴合度,满意后在C型臂透视下在支架近端钉入第1枚钉子用于定位、在支架最远端钉入第2枚钉子用于初步锁定。推紧钢板并调整至满意位置后,分别将剩余钉子打入,完成钢板固定。C型臂透视下检查钉子固定情况,满意后进行术区清理及切口缝合。(2)DHS组患者手术方式:选择髋关节外侧为手术切口入路,切口长度10~15 cm,依次切口皮肤与肌肉组织后进行骨折复位操作。C型臂透视下在股骨粗隆上端头颈中钉入DHS导针进行预固定。调整正侧位角度,满意后在DHS导针上分钉入防旋钉,测量DHS导针长度后进行攻丝处理,并选择长度合适的DHS螺丝钉拧入。完成固定后置入鋼板,调整钢板位置满意后分别钉入固定螺钉,完成钢板固定。透视下检查钢板及钉子情况,满意后清理术区、置入引流管并缝合切口。(3)PFNA组患者手术方式:手术切口入路与LISS相同,切口长度3~5 cm,依次切开皮肤与肌肉组织,处理后暴露术区。在粗隆顶点进针,保证导针居中进行股骨远端扩髓,选择大小合适的PFNA主钉置入,在C型臂透视下调整主钉深度与角度。然后测量骨质导针长度,并选择长度合适的螺旋刀片锁定远端螺钉。最后C型臂透视下检查处置情况,满意后清理术区、置入引流管并缝合切口。
1.3 观察指标
(1)统计患者手术相关指标(手术时间、术中失血量、骨折愈合时间、住院时间及术后并发症等);(2)Harris髋关节功能评分,总分100分,<70分表示差,70~79分为尚可,80~89分为较好,90分以上为优;(3)统计所有患者基本资料,包括性别、年龄、骨折原因、骨折分型、术后首次负重时间、术后并发症率、手术方式等。
1.4 统计学处理
本研究所有数据以SPSS 19.0进行统计学分析。手术时间、术中失血量、骨折愈合时间、住院时间及Harris评分等计量资料以(x±s)表示,符合正态分布采用t检验,计数资料以率(%)表示,采用字2检验,多元回归分析采用Logistic分析,P<0.05为差异有统计学意义。
2 结果
2.1 三组患者手术指标比较
手术时间、术中失血量由高至低分别为DHS组、LISS组、PFNA组,且差异均有统计学意义(P<0.05)。PFNA组的住院时间、术后并发症率均显著少于LISS组与DHS组(P<0.05),LIIS组与DHS组则无显著差异(P>0.05);LISS组患者骨折愈合时间稍多于DHS及PFNA组,但三组差异无统计学意义(P>0.05),见表1。

