Perineural invasion as a prognostic factor in patients with stage l-lll rectal cancer-5-year follow up
Milica Stojkovic Lalosevic,Tamara Milovanovic,Marjan Micev,Mirjana Stojkovic,Sanja Dragasevic,Milos Stulic,Ivan Rankovic,Vladimir Dugalic,Zoran Krivokapic,Aleksandra Pavlovic Markovic
Milica Stojkovic Lalosevic,Tamara Milovanovic,Mirjana Stojkovic,Sanja Dragasevic,Milos Stulic,lvan Rankovic,Aleksandra Pavlovic Markovic,Clinic for Gastroenterology and Hepatology,Clinical Center of Serbia,Belgrade 11000,Serbia
Milica Stojkovic Lalosevic,Tamara Milovanovic,Marjan Micev,Mirjana Stojkovic,Sanja Dragasevic,Milos Stulic,lvan Rankovic,Vladimir Dugalic,Zoran Krivokapic,Aleksandra Pavlovic Markovic,School of Medicine,University of Belgrade,Belgrade 11000,Serbia
Marjan Micev,Vladimir Dugalic,Zoran Krivokapic,Clinic for Digestive Surgery-First Surgical Clinic,Clinical Center of Serbia,Belgrade 11000,Serbia
Abstract
Key words:Lymphovascular invasion;Perineural invasion;Rectal cancer
INTRODUCTION
Colorectal cancer (CRC) is still the most common gastrointestinal malignancy Worldwide,and one of the most common cancers in general population[1].Concerning geographical distribution,among different regions in Europe,South-eastern Europe has one of the highest incidences and mortality rates of CRC[2].Recent data of the Institute of Public Health of Serbia,have marked CRC as the second most common malignancy in men,with an incidence of approximately 70 per 100000 individuals[3].Rectal cancer (RC) accounts about one third of all diagnosed CRCs,with rising incidence especially in in Western countries[4].Earlier studies have speculated that left-sided CRC and right-sided CRC are potentially two biologically distinct entities,with different molecular pathways as well as different clinical and histopathological characteristics.It has been noted that patients with RC are older,with larger tumor diameter as well as higher metastasis rate,poorer differentiation and high reoccurrence rate[5].Features affecting the outcome of these patients are multiple,and different histology markers have been proposed as important prognostic factors.Despite the fact that previous studies have examined numerous markers regarding the adequate staging of the disease,TNM staging is still used in everyday clinical practice,although it relays only on the anatomic progression of the disease.Though TNM staging has proven as applicable in very early and very late disease stages,still its accuracy in the intermediary stages of the disease remains controversial[6].Precise pathological examination is needed in order to determine which patients would benefit from adjuvant therapy.Earlier investigations have observed that the presence of perineural invasion (PNI) or/as well as lymphovascular invasion (LVI)considerably correlates with the cancer-related outcome[7].PNI is defined as invasion of nervous structures by malignant cells,whereas LVI is considered as presence of malignant cells in blood/lymphatic vessels.Considering adjuvant therapy is reserved for RC patients with locally advanced stage III,it remains challenging whether patients with earlier stages should receive adjuvant therapy.In the present study we aimed to analyze the clinical significance of PNI as well as LVI in patients with stage I-III RC and to investigate whether these two histopathological features alone or combined affect overall survival of RC patients.
MATERIALS AND METHODS
Study population and data collection
A prospective study included newly diagnosed stage I-III RC patients treated and followed at the Clinic for Digestive Surgery,Clinical Center of Serbia,between the years of 2014-2016.All recruited patients had their diagnosis histologically confirmed in accordance with both TNM and Dukes classification[8].Patients obtained diagnosis of RC adenocarcinoma initially on histopathology reports after colonoscopy and later confirmed after surgical treatment.All patients underwent abdominal ultrasonography,abdominal and pelvic CT/or MRI,or endorectal ultrasonography when necessary and chest radiography.In addition,the patient's demographics,surgical details,histopathological details and postoperative outcome were also noted.Histopathology details included:Size of the tumor as well as infiltration,number of involved lymph nodes,differentiation,LVI,PNI and all other characteristics of standard protocol were recorded.Lymphovascular invasion has been defined as presence of cancer cells in vascular or lymphatic structures,whereas perineural invasion has been defined as presence of cancer cells in any of the layers of nerve sheath or perineural space[7].PNI and LVI were detected using routine H&E staining.Patients with locally advanced stage RC received adjuvant chemoradiotherapy,consisted of 44-50 Gy radiotherapy delivered into the whole pelvis,and capecitabine or 5-FU as chemotherapy.Surgical treatment was according to principles of total or partial mesorectal excision[9].Patients meeting the following criteria were excluded from our study:(1) Recurrent RC or metastatic RC disease;(2) Prior 5-years history of other malignancy;(3) Presence of inflammatory bowel disease;(4) Histopathologically confirmed squamocellular carcinoma or neuroendocrine tumor;and (5) Unresectable RC.The study was approved by the Institutional Ethical board (approval number 56-6,Clinical center of Serbia) and was performed in accordance with principles of Helsinki declaration.Informed written consent was obtained from all recruited subjects.
Statistical analysis
Statistical analysis was carried out using the SPSS ver.20.0 (SPSS Inc.,Chicago,IL,United States).Patient's demographics,clinical and pathological characteristics were summarized.Continuous variables were expressed as mean ± SD.Normality of distribution was investigated by Kolmogorov-Smirnov test.The clinicopathological variables between the groups were analyzed usingχ2test.Overall survival (OS) was calculated from the date the diagnosis has been made till the date of lethal outcome or the date of last follow-up.Disease free survival (DFS) was calculated from the date the diagnosis has been made till the date of last follow-up.Kaplan-Meier survival analysis has been used for plot of survival data and differences were analyzed by log-rank test.Cox proportional hazard models were used to analyze survival by each variable.A value ofP <0.05 was considered statistically significant.
RESULTS
Patients characteristics
Demographic,clinical and pathological characteristics of patients are summarized in Table 1.The mean follow-up time in our cohort of patients was 45 mo.
Tumor characteristics according to perineural invasion status
We found no significant differences regarding age,sex and body mass index in different PNI as well as LVI status (P> 0.05).However,there was statistically significant difference in T stage,N stage and differentiation grade in patients with different PNI status (P <0.05) (Table 2).Moreover,we found statistically significant difference in same tumor characteristics regarding LVI status (P <0.05).Additionally,patients with LVI and PNI had more advanced disease in the setting of T stage as well as N stage,and a tendency towards poorer differentiation (P <0.05).
Prognostic factors of RC patients
Overall 5-years survival rate was 97% for TNM stage I,89% for TNM stage II,and 49% for TNM stage III respectively.There was high statistically significant difference regarding OS between different TNM stages (P <0.05) (Figure 1).Local recurrence was observed in 32 patients (10%),and distant recurrence was found in 45 (15%).Disease free survival was 87% for TNM stage I,79% for TNM stage II,and 34% for TNM stage III respectively.When we analyzed survival rates with regards to PNI status,we found that patients without PNI had 84% OS and 66% DFS and whereaspatients with PNI had OS of 48% and DFS of 34% (Figure 2).Moreover patients without LVI had 87% OS,and 66% DFS while patients with LVI had 61% OS and 34%(Figure 3).There was high statistically significant difference regarding OS and DFS between different LVI and PNI status (P <0.05).Furthermore when patients were both LVI and PNI positive survival rate was 43% in comparison to both LVI and PNI negative status 86% (P <0.05) (Figure 4).Cox proportional hazard model was further used to investigate the independent survival prognostic factors.After controlling the age and gender both LVI presence and PNI presence significantly correlated with poor overall survival and disease free survival (P <0.05).Namely presence of LVI was associated with 3-fold higher risk of lethal outcome (HR = 3.23;95%CI:1.800-5.800;P<0.05) and 2-fold higher risk of disease recurrence (HR = 2.33;95%CI:1.094-4.967;P <0.05).Presence of PNI was associated with almost 4-fold higher risk of lethal outcome(HR = 3.99;95%CI:2.231-7.148;P <0.05),and 6-fold higher risk of disease recurrence(HR = 6.11;95%CI:2.651-14.079;P <0.05).Lethal outcome risk was higher when both PNI and LVI were present (HR = 5.49;95%CI:2.889-10.429;P <0.05).
DISCUSSION
Previous studies have widely investigated pathways of metastases formation in CRC.Namely,vascular and lymphatic pathways have been acknowledged as common route for distant cancer spreading.However,numerous investigations have highlighted the pathway of cancer spreading trough nerve invasion of cancer cells.Bearing in mind that first step in metastases formation is invasion of vascular and neural structures,LVI and PNI individually as well as combined have been a focus of investigations in different cancer types,including CRC[10].However limited number of studies investigated influence of both LVI and PNI in early and intermediate stages of RC.
In the available literature presence of LVI ranges from 10% up to almost 90%[11,12].In comprehensive retrospective analysis of Hoganet al[13]where LVI was observed in both CRC and RC patients,LVI was present in about 30% of the patients with RC.Results of Hoganet al[13]are similar to our own,where LVI was present in 38% of the patients.However,the results of Zhonget al[14]as well as Kimet al[6]reported presence of LVI in 20% and 16% patients,respectively.Wide discrepancies in the presence of LVI could be due to heterogeneity of study population,taking into account that majority of studies included both CRC and RC patients.Moreover,different histopathology methods used in specimen staining could potentially influence detection of LVI.Discrepancies could also be due to differences in interpretation of LVI,as some authors note LVI as lymphatic invasion,or angiolymphatic invasion or venous invasion[15,16].
Hoganet al[13]state that LVI is associated with adverse OS in RC group of patients,although the presence of LVI was higher in colon cancer patients.This furthermore emphasizes the necessity of LVI assessment in RC patients.
In our cohort of patients with LVI had 61% survival rate,while patients without LVI had 87% survival rate.There was high statistically significant difference regarding OS between different LVI statuses.In study of Choet al[17],LVI was found to be strong prognostic factor for worse OS in RC patients,with 3-fold higher risk of lethal outcome.Results of the Sunet al[7]additionally emphasize the significance of LVI detection in RC patients,where LVI presence was associated with even 4-fold higher risk of poor survival.Results of both studies are in concordance with the results of our investigation,where we have found that patients with LVI have 3-fold higher risk of lethal outcome.
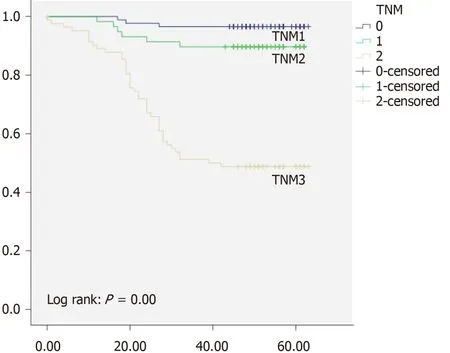
Figure1 Kaplan Meier curve regarding TNM status of rectal cancer patients.
PNI has been a field of investigation in many cancers,firstly head and neck,and later bladder and prostate cancer as well as pancreatic and gastric cancers[18-20].The importance of PNI detection in the terms of treatment decision is necessary,considering that earlier investigations in patients with CRC have marked PNI as a predictor of poor prognosis[12].
In large study of Songet al[21]presence of PNI was found in 17% of the patients,while Huhet al[12]reported presence of PNI was found in 19% of the patients.Results of our study are in concordance with the results of previous investigations.To be specific,PNI was present in 19% of our patients with RC.
Kinugasaet al[22]reported that patients with PNI had 51% 5-year survival rate compared to PNI absent patients with 80% survival rate.Results of our study are similar to previously reported.In our cohort patients with PNI had survival rate of 48%,and patients without PNI had 84% of 5-year survival rate.The data in available literature demonstrate that OS in CRC as well as RC,differ trough stages,and is dependent from many cofounding factors including LVI and PNI[23].Namely it has been shown that presence of LVI and PNI is associated with more advanced tumors,as well as poor overall survival.In the study of Zhenget al[24]patients with PNI showed significantly worse survival than those without PNI.In the previously mentioned study of Sunet al[7]patients with PNI had 4.8-fold higher risk of poor survival.Swetset al[25]have marked PNI as a indicator for adjuvant therapy,with presence of PNI associated with 3-fold higher worse survival.Results of our investigation suggest that patients with PNI had almost 4-fold higher risk of lethal outcome,which is in accordance with previously reported.Risk is even higher when both PNI and LVI are present,which is similar to the results of Sunet al[7].
This was a single center study on early and intermediate rectal cancer patients who were all Caucasian,so these were the limitations of our study.
In conclusion results of our study suggest that PNI and LVI individually and combined have significant impact on survival rates of early and intermediate rectal cancer patients.Additional randomized prospective studies are necessary to investigate potential benefits of adjuvant therapy for these patients.
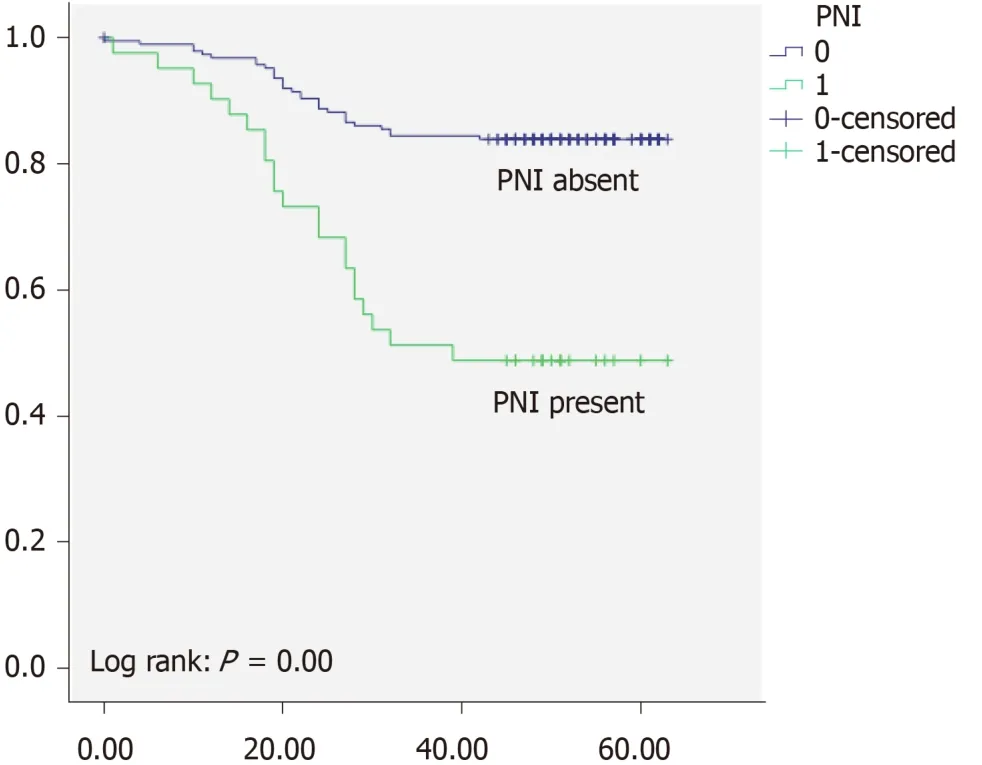
Figure2 Kaplan Meier curve regarding perineural invasion status of rectal cancer patients.
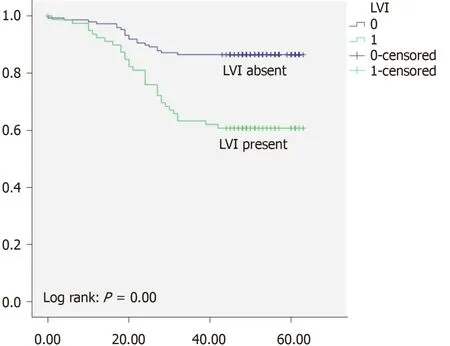
Figure3 Kaplan Meier curve regarding lymphovascular invasion status of rectal cancer patients.
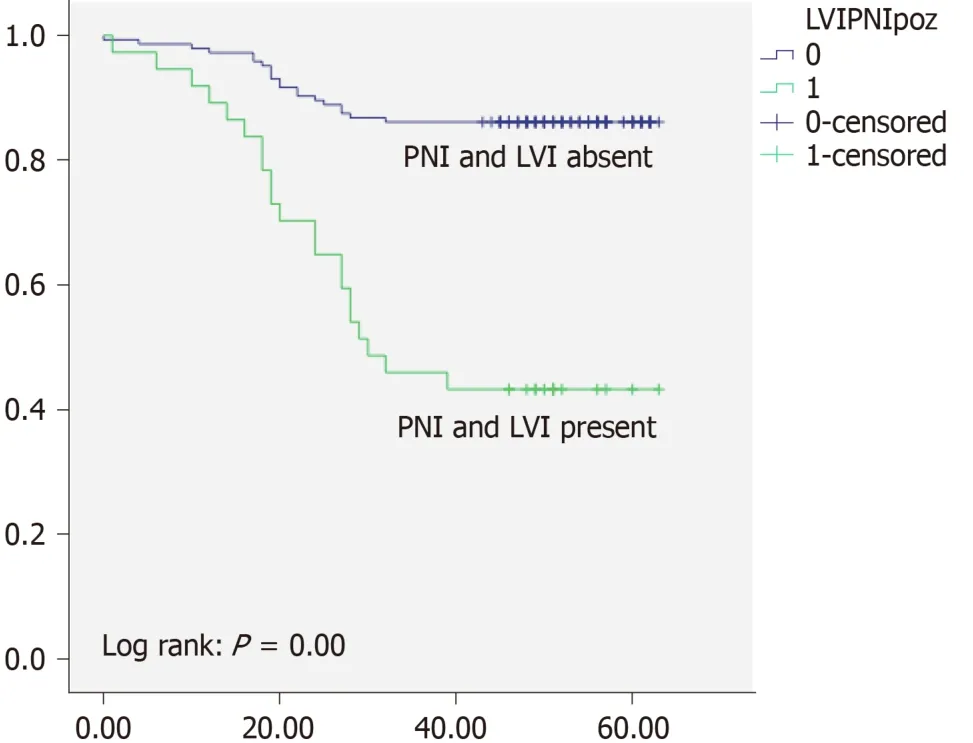
Figure4 Kaplan Meier curve regarding both perineural invasion and lymphovascular invasion status of rectal cancer patients.
ARTICLE HIGHLIGHTS
Research background
Rectal cancer (RC) accounts about one third of all diagnosed colorectal cancers.Although TNM staging has proven as applicable in very early and late disease stages,accuracy in the intermediary stages of the RC remains controversial.Precise pathological examination is needed in order to determine which patients would benefit from adjuvant therapy.Few previous investigations have focused on correlation of presence of perineural invasion (PNI) or/as well as lymphovascular invasion (LVI) with the cancer-related outcome in RC patients,therefore more studies in this field are need ed.
Research motivation
Considering the rising incidence of RC,we have investigated easily applicable and reliable factors that can potentially predict potential outcomes in patients with RC.
Research objectives
We evaluated the clinical significance of PNI as well as LVI in patients with stage I-III RC and further investigated whether these two histopathological features alone and combined affect survival of RC patients.
Research methods
We have prospectively studied patients with early and intermediate RC.Using Kaplan-Meier method we have analyzed the median survival time,whereas Cox proportional hazards models were used to evaluate the influence of PNI and LVI as prognostic factors in RC patients.
Research results
Using Kaplan-Meier analysis for overall survival rate,we have found that both LVI and PNI were associated with lower overall survival rates as well as disease free survival rates (P < 0.01).Moreover when Cox multiple regression model was used,presence of LVI was associated with 3-fold higher risk of lethal outcome and 2-fold higher risk of disease recurrence (P < 0.05).Presence of PNI was associated with almost 4-fold higher risk of lethal outcome and 6-fold higher risk of disease recurrence (P < 0.05).
Research conclusions
This study supports the hypothesis that PNI as well as LVI should be carefully and thoroughly examined in the histopathological analysis of RC patients even in early and intermediate disease stages,bearing in mind that such findings could have a great impact on the prognosis.Also patients with both LVI and PNI involvement even in early stages of the disease should not be overlooked,and must be monitored carefully with more frequent and detailed check-ups.
Research perspectives
PNI and LVI should be included as obligatory analysis in histopathology reports of RC patients.Additional randomized prospective studies are necessary to confirm these results,and also to investigate other potential prognostic factors in RC patients.
 World Journal of Gastrointestinal Oncology2020年5期
World Journal of Gastrointestinal Oncology2020年5期
- World Journal of Gastrointestinal Oncology的其它文章
- Espresso coffee,caffeine and colon cancer
- Association of Helicobacter pylori infection with colorectal polyps and malignancy in China
- Gastric cancer with peritoneal metastases:Efficiency of standard treatment methods
- Perioperative chemotherapy for advanced gastric cancer-results from a tertiary-care hospital in Germany
- Neutropenia in colorectal cancer treated with oxaliplatin-based hyperthermic intraperitoneal chemotherapy:An observational cohort study
- Characterization and strong risk association of TLR2 del-196 to-174 polymorphism and Helicobacter pylori and their influence on mRNA expression in gastric cancer
