Association of Helicobacter pylori infection with colorectal polyps and malignancy in China
Man Wang,Wen-Jie Kong,Jing-Zhan Zhang,Jia-Jie Lu,Wen-Jia Hui,Wei-Dong Liu,Xiao-Jing Kang,Feng Gao
Man Wang,Wen-Jie Kong,Jia-Jie Lu,Wen-Jia Hui,Wei-Dong Liu,Feng Gao,Department of Gastroenterology,People's Hospital of Xinjiang Uygur Autonomous Region,Urumqi 830001,Xinjiang Uygur Autonomous Region,China
Jing-Zhan Zhang,Xiao-Jing Kang,Department of Dermatology,People's Hospital of Xinjiang Uygur Autonomous Region,Urumqi 830001,Xinjiang Uygur Autonomous Region,China
Abstract
Key words: Helicobacter pylori;Atrophic gastritis;Intestinal metaplasia;Polyps;Colorectal cancer;Gastrointestinal neoplasms
INTRODUCTION
Colorectal cancer (CRC) accounted for 881000 deaths in 2018,representing 9.8% of deaths worldwide.The incidence rate of CRC has increased to the extent that 1.8 million new CRC cases were diagnosed in 2018,according to recent data by the World Health Organization[1].However,it is difficult to detect CRC early due to the lack of typical clinical symptoms,and 20% of patients who are asymptomatic at diagnosis may manifest with aggressive metastases[2].The appearance of colorectal polyps and malignancy is a complex process that involves a combination of dietary habits,smoking,drinking and other environmental factors,and genetic susceptibility[3,4].Colorectal polyps are abnormal protrusions on the surface of the large intestine[5]that are either non-adenomatous or adenomatous polyps.Colorectal adenomatous polyps are considered to be the most important precancerous lesions,developing into CRC through the adenomatous cancer sequence[6].Therefore,early screening and detection of precancerous lesions can prevent the occurrence and development of CRC[7].
GastricHelicobacter pylori(H.pylori) infection is a global public health concern,which has infected approximately[8]50% of the world population,according to recent epidemiological studies[9].The chronic inflammatory state caused byH.pyloriinfection is closely related to the occurrence of gastric cancer.H.pyloriis listed as a class I carcinogen by the World Health Organization International Agency for Cancer Research[10]and is also involved in the tumorigenesis of extragastric target organs,such as lung cancer,and hepatocellular carcinoma[11].Previous studies have indicated that gastricH.pyloriinfection increased the risk of colorectal tumors[12-16].In contrast,however,several other reports have concluded that gastricH.pyloriinfection was not correlated with colorectal polyps or CRC[17-21].Thus,the results of different research studies in different regions vary significantly.Therefore,the present study investigated the relationship between gastricH.pyloriinfection,colorectal polyps,and CRC in northwestern China.In addition,the study provides answers to questions regarding the necessity for colonoscopy screening in patients with gastricH.pyloriinfection.
MATERIALS AND METHODS
Study population
We reviewed the consecutive electronic medical records of patients who underwent gastroscopy and colonoscopy at a regional institution from January 2014 to January 2019.The inclusion criteria included:(1) Complete general information (including gender,age,ethnicity,past history,family history,etc.);(2) Age ≥ 18 years;(3) Patients who underwent bidirectional endoscopy (colonoscopy performed immediately after gastroscopy);(4) A clear pathological diagnosis of colorectal polyps or CRC;and (5)Detection ofH.pyloriinfection.Exclusion criteria were as follows:(1) History of gastric cancer,peptic ulcer,and other malignant tumors;(2) Received antibiotics,NSAIDs,proton pump inhibitors or glucocorticoids in the past month;(3) Patients who underwentH.pylorieradication therapy previously,or radiation therapy,chemotherapy,and other specific treatment for tumors;(4) No total colonoscopy or biopsy;(5) Previous history of gastrointestinal surgery;(6) Presence of inflammatory bowel disease,familial adenoma,Gardner's syndrome (a disease that affects the incidence of CRC);(7) A history of severe systemic disease;(8) A family history of polyposis,and (9) Patients who underwent repeated hospitalizations and a history of endoscopic polyp therapy.All patients provided consent for the study.
The diagnosis of normal intestinal mucosa,colorectal polyps,CRC,atrophic gastritis,and intestinal metaplasia was mainly based on endoscopic manifestations and histopathological examinations.Pathological diagnoses required confirmation by two pathologists.Referring to the fourth national consensus report onH.pyloriinfection treatment in 2012[22],H.pyloriinfection was defined as follows:Positive14Curea breath test and/or positive hematoxylin and eosin staining on gastric biopsies.
Study design
All subjects underwent complete colonoscopy and data regarding the location,size,shape,and number of polypoid lesions and the location of tumors were recorded.According to the size of the largest polyp,the patients with colorectal polyps were divided into those with a maximum diameter ≥ 1 cm and those with a maximum diameter ≤ 1 cm.According to the number of polyps,patients with a single polyp were included in the solitary polyp group,and those with ≥ 2 polyps were included in the multiple polyps group.Colorectal polyps and CRC were classified according to the location.The distal colorectum was defined as the anus to the splenic flexure,while the proximal colon was defined as the cecum to the splenic flexure,and patients with multiple lesions on both sides were defined as the whole colon.We dividedH.pylori-related gastric disease into atrophy and intestinal metaplasia according to a method described previously[23].Colorectal polyps including non-adenomatous and adenomatous polyps were considered.The prevalence of gastricH.pyloriinfection in CRC patients,patients with colorectal polyps,and the control group were compared.In addition,the prevalence of atrophic gastritis or intestinal metaplasia with gastricH.pyloriinfection among CRC patients,colorectal polyp patients,and the control group was also compared.
Statistical analysis
SPSS 17.0 was used for statistical analysis.Data for continuous variables were expressed as mean ± SD,and categorical data as a ratio or percentage.Thet-test was used for data with a normal distribution.For comparisons among multiple groups of means (e.g.,sex,BMI),one-way ANOVA was used.If the hypothesis of homogeneity of variance was not satisfied,Welch's ANOVA was used.In addition,we used theχ2test to compare categorical variables.A logistic regression model was applied to estimate the correlation betweenH.pyloriinfection,colorectal polyps,and CRC.After adjusting for gender and age,we calculated the odds ratio (OR) value and 95%confidence interval (95%CI).All variables withP< 0.05 were considered statistically significant and remained in the final models.
RESULTS
Patient characteristics
In total,6538 patients were enrolled in our study (Figure 1).The characteristics of the participants are outlined in Table 1.Of these patients,3872 were confirmed to have colorectal polyps and 304 had CRC by colorectal biopsy,and the remaining 2362 patients who had no abnormalities on colonoscopy,no history of polypectomy,and no clinical symptoms were classified as controls.The patient group with colorectal polyps included 2189 men and 1683 women.Their mean age was 53.01 ± 12.60 years.The patient group with CRC comprised 167 men and 137 women with an average age of 61.26 ± 12.94 years.The control group comprised 1355 men and 1007 women with a mean age of 45.81 ± 13.44 years.There were significant differences in age among the three groups (Welch F = 320.48,P< 0.001).However,there were no significant differences in gender,BMI,smoking,drinking,or family history of CRC among the three groups (P= 0.66;P= 0.06;P= 0.39;P= 0.28;P= 0.16,respectively).All patients underwent gastroscopy on the day of colonoscopy.The main indications for performing gastroscopy and colonoscopy are shown in Table 2.
Correlation between H.pylori infection and colorectal polyps
The colonoscopy findings and pathological characteristics of colorectal polyps are shown in Table 3.The prevalence ofH.pyloriinfection in the colorectal polyp group(2134/3872,55.11%) was higher than that in the control group (890/2362,37.68%;P<0.001).Multivariate logistic regression demonstrated that the patients with positiveH.pyloriinfection in the colorectal polyp group had a higher OR after age and gender adjustment (adjusted OR = 2.19,95%CI:1.96-2.44,P< 0.001).The prevalence ofH.pyloriinfection was higher in the multiple polyps group than that in the solitary polyp group and the control group (adjusted OR = 1.15,95%CI:1.02-1.31,P= 0.03;adjusted OR = 2.41,95%CI:2.12-2.74,P< 0.001).The positive rate ofH.pyloriinfection in the adenomatous polyp group (952/1588,59.95%) was higher than that in the nonadenomatous polyp group (1182/2284,51.75%,adjusted OR = 1.41,95%CI = 1.24-1.60,P< 0.001).The same association was found between the adenomatous polyps and control groups (adjusted OR = 2.53,95%CI:2.20-2.89,P< 0.001).However,the polyp size and locations were not associated withH.pylori(P= 0.26;P= 0.08).According to the polyp location,thePvalue of the proximal colon was 0.18,the distal colorectal was 0.23,and the whole colon was 0.51.Furthermore,based on the status ofH.pyloriinfection and histopathological findings of the gastroscopy specimens,we found that the incidence ofH.pylori-related atrophic gastritis in the colorectal polyp group was 34.99% (1355/3872),which was higher than that in the control group (541/2362,22.90%,P< 0.001) (Table 4).H.pylori-associated atrophic gastritis was significantly associated with colorectal polyps compared to that in the control group (adjusted OR= 5.42,95%CI:4.67-6.30,P< 0.001).The prevalence ofH.pylori-related intestinal metaplasia in the patient group with colorectal polyps was 8.96% (347/3872),which was higher than that in the control group (105/2362,4.45%) (P< 0.001).Overall,H.pylori-associated intestinal metaplasia status was positively associated with colorectal polyps (adjusted OR = 5.88,95%CI:4.60-7.52,P< 0.001).
Correlation between H.pylori infection and CRC
The prevalence ofH.pyloriinfection in the CRC group (189/304,62.17%) was higher than that in the control group (890/2362,37.68%) (P< 0.001).After adjustment for age and gender,multivariate logistic regression demonstrated that the patients with positiveH.pyloriinfection in the CRC group had a higher OR (adjusted OR = 3.05,95%CI:2.33-3.99,P< 0.001) and among 304 patients with CRC,270 cases had adenocarcinoma,including 167 cases withH.pyloriinfection (61.85%);11 cases had neuroendocrine tumors,including 7 cases withH.pyloriinfection (63.64%);14 cases had intramucosal cancer,including 9 cases withH.pyloriinfection (64.29%);9 cases had signet ring cell cancer,including 6 cases withH.pyloriinfection (66.67%).The histopathological findings of CRC were not related toH.pylori(P> 0.05).Moreover,theχ2test showed that CRC location was not correlated withH.pyloriinfection (P=0.62).Compared to the control group,bothH.pylori-related atrophic gastritis and intestinal metaplasia significantly increased the risk of CRC (adjusted OR = 3.46,95%CI:2.63-4.55,P< 0.001;adjusted OR = 4.86,95%CI:3.22-7.34,P< 0.001) (Table 2).
DISCUSSION
H.pyloriinfection plays an important role in the pathogenesis of gastrointestinal diseases[24].However,whether gastricH.pyloriinfection increases the risk of colorectalpolyps and CRC has been debated in various studies.This could be related to differences in the dietary habits of the study population,the patient population susceptibleH.pylori,study sample size,and other factors.TheH.pyloriinfection rate in China is more than 50%[25].The relationship between gastricH.pyloriinfection and colorectal polyps and CRC in Northwest China is unclear;thus,we conducted this study.Some studies have shown that gender and age are related toH.pyloriinfection,colorectal polyps,and CRC[12,26].Therefore,we conducted a multifactorial logistic regression analysis after adjusting for those factors.No significant differences in BMI,smoking,drinking,or family history of CRC among the subjects were found.

Table1 Baseline characteristics of the participants,n (%)
The results showed that the increase inH.pyloriinfection rate was positively correlated with the increase in colonic polyp incidence,polyp number,and malignancy,suggesting thatH.pyloriinfection might be a risk factor for colorectal polyps and tumors.Patients withH.pyloriinfection are 2.19 times more likely to develop colorectal polyps and 3.05 times more likely to develop CRC than those who do not haveH.pyloriinfection.Additionally,we found that the incidence ofH.pyloriinfection coexisting with atrophic gastritis or intestinal metaplasia was higher in patients with colorectal polyps and CRC than in the control group.There was a significant correlation betweenH.pylori-associated gastropathy and colorectal adenomatous polyps or CRC.These results are consistent with those of previous studies[26,27].A large-scale population-based study by Sonnenberget al[28]also supports this argument.However,another study found no significant relationship betweenH.pyloriinfection and CRC.This may have been due to the broader age range and the limited number of patients[29].
There are a few plausible theories to explain the distribution of colorectal polyps and CRC and its association withH.pyloriinfection.Honget al[30]found that gastricH.pyloriinfection was positively associated with an increased risk of proximal colorectal adenomatous polyps.Zhanget al[31]found thatH.pyloriinfection mainly increased the risk of distal CRC.However,our study illustrates that gastricH.pyloriinfection could increase the risk in both proximal and distal colorectal neoplasms,which was consistent with the study by Inoueet al[32,33].H.pyloriinfection causes microbiological changes in the digestive tract,increases the production of bile acids,causes DNA damage and activation,plays an important role in the proximal colonic mucosa,and increases the risk of proximal colonic polyps and malignancy[34].Preclinical models have demonstrated that increased gastrin secretion caused byH.pyloriinfection has a mitogenic effect and selectively acts on the distal colon,thereby increasing the risk of distal colon polyps and malignancy[35].These mechanisms may work synergistically.In addition,in our study,no significant differences were found among CRC patients with different pathological types and the prevalence ofH.pyloriinfection.This may be because the most prevalent type of CRC is adenocarcinoma;however,studies with a larger sample size are needed to confirm this hypothesis.
The mechanism by which gastricH.pyloriinfection increases the incidence of colorectal polyps and CRC is not clear.Some studies have shown that gastrin gene expression is up-regulated in both colorectal polyps and CRC[36,37],andH.pyloriinfection can cause hypergastrinemia.Gastrin acts on gastrointestinal epithelial cells and can promote the formation of COX-2,which affects the occurrence,development,invasion,and metastasis of colorectal neoplasia[38].Gastrin can also induce colonic mucosal cell proliferation to promote the development of CRC[39].Moreover,from the perspective of gastrointestinal microecology,chronic gastritis caused by long-termH.pyloriinfection can lead to massive glandular atrophy and decreased gastric acid secretion.Low gastric acid may adversely affect the intestinal flora,cause bacterial overgrowth,colonic disorders,and colorectal carcinogenesis[40,41].In addition,H.pyloriinfection may cause damage to colorectal epithelium through the chronic inflammatory response mediated by inflammatory factors such as interleukin-8[42].
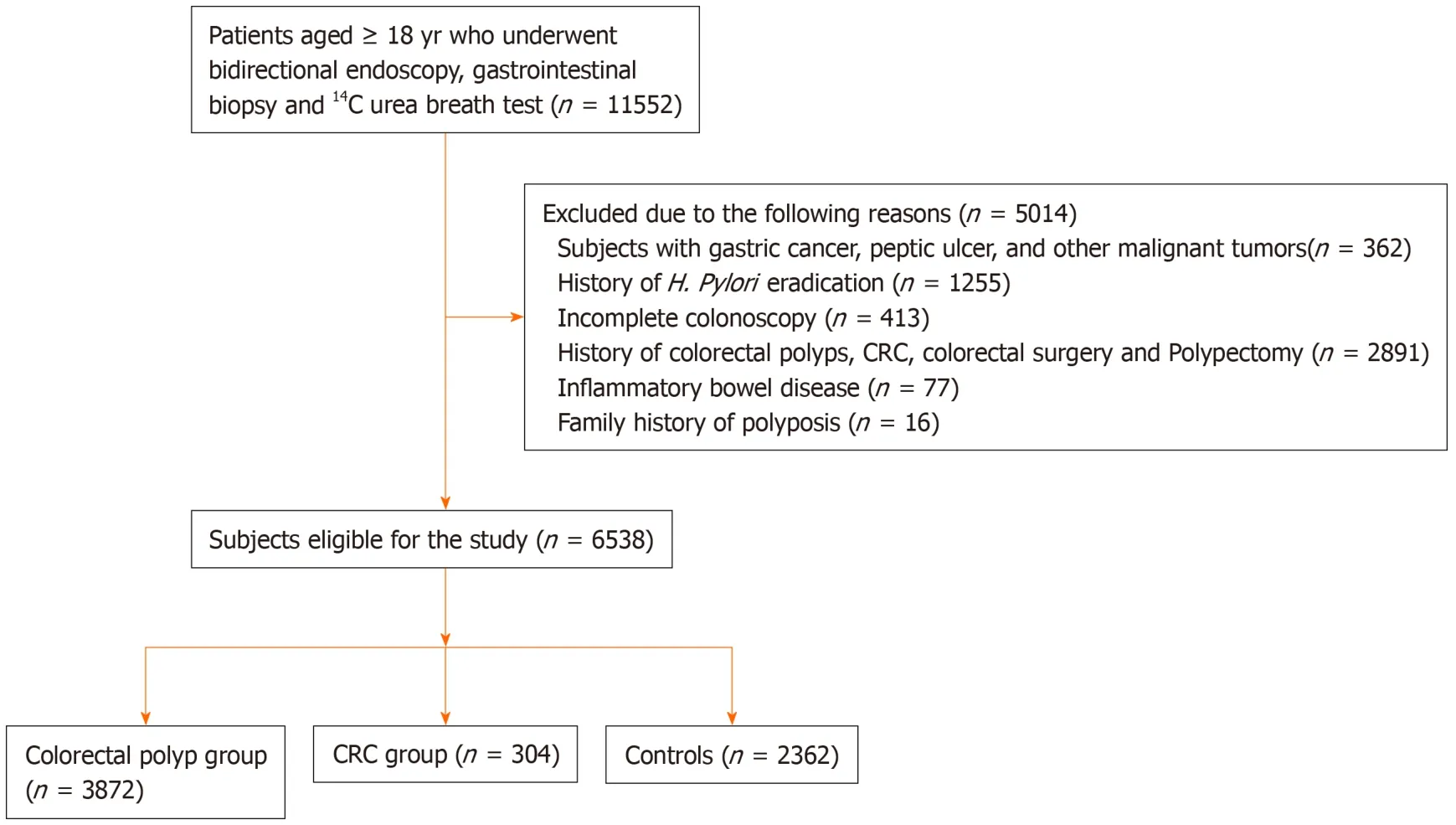
Figure1 Flowchart of the study participants.
The early diagnosis of CRC is relatively difficult.During the development of CRC,the normal mucosa develops into an adenoma and then to adenocarcinoma.This process provides opportunities for early detection and intervention of CRC.Early diagnosis and resection of colonic polyps can reduce the morbidity and mortality of CRC[43].Further studies with regard to pathogenic mechanisms should be continued,which can help to develop relevant prevention and early detection strategies.
Some studies found that only the current situation ofH.pyloriinfection could stimulate the immune response,thus inducing or perpetuating chronic inflammation of the gastrointestinal tract[44,45].The strength of our study was that histopathological results and the14C-urea breath test were used to determineH.pylori.A histopathological examination has high specificity and sensitivity in the diagnosis of gastric pathological changes andH.pyloriinfection.However,histopathological examination and the14C-urea breath test can only diagnose the current infection ofH.pylori,compared with the serological tests,which do not distinguish current or past infections.Therefore,our study explains the current relationship betweenH.pyloriinfection,colorectal polyps,and CRC more accurately.In addition,our sample size was relatively large,which is an advantage of this study.
Our study also has several limitations.First,we did not consider the possible effect of the duration ofH.pyloriinfection on colorectal polyps and CRC.Secondly,we did not consider other confounding factors,such as constipation,eating habits,and metabolic syndrome.Thirdly,this was a single-center study.More investigation through prospective multicenter studies with large sample sizes should be conducted.
In conclusion,this study showed that gastricH.pyloriinfection andH.pylori-related gastric atrophic or intestinal metaplasia increased the risk of colorectal polyps and CRC.Early colonoscopy screening and surveillance is necessary to reduce the risk of colonic polyps and CRC in patients withH.pyloriinfection.Further investigation is required to understand whether the eradication of gastricH.pylorican reduce the occurrence of colorectal polyps and CRC.
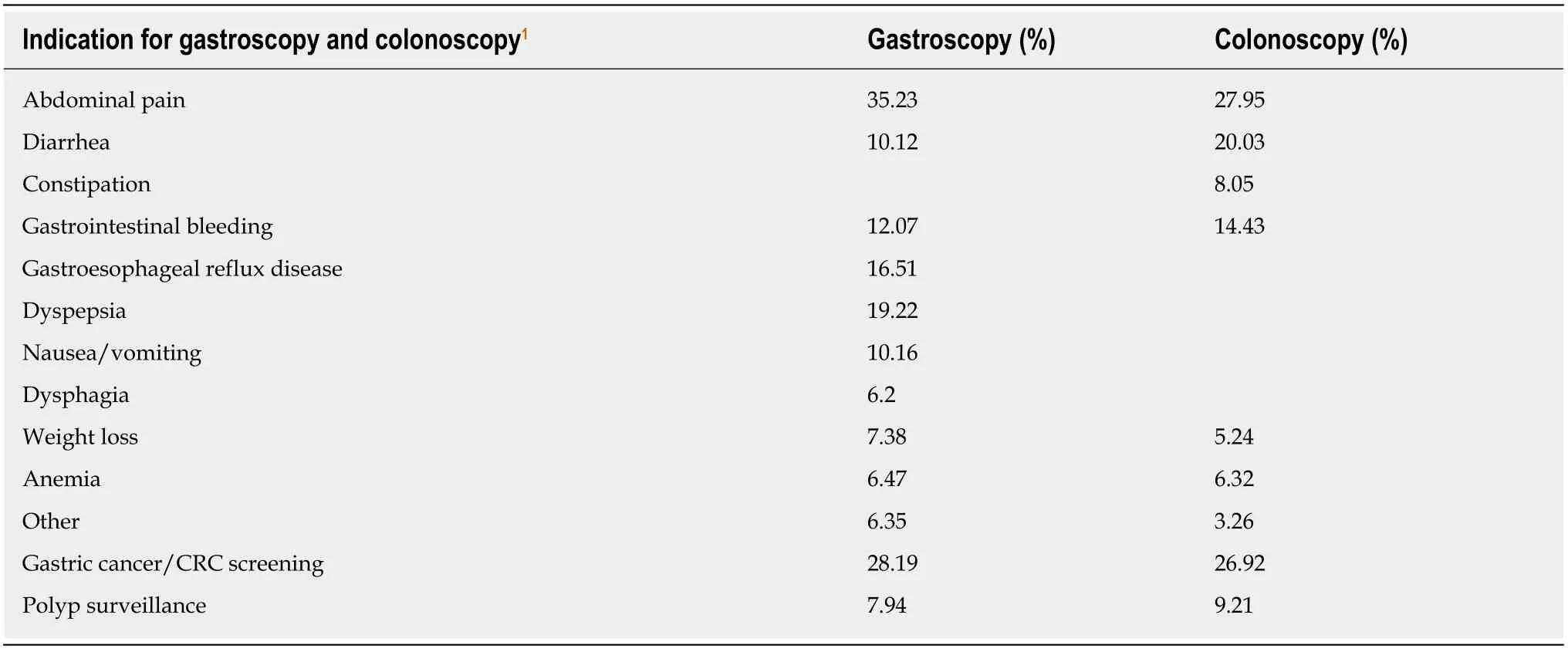
Table2 The main indications for gastroscopy and colonoscopy
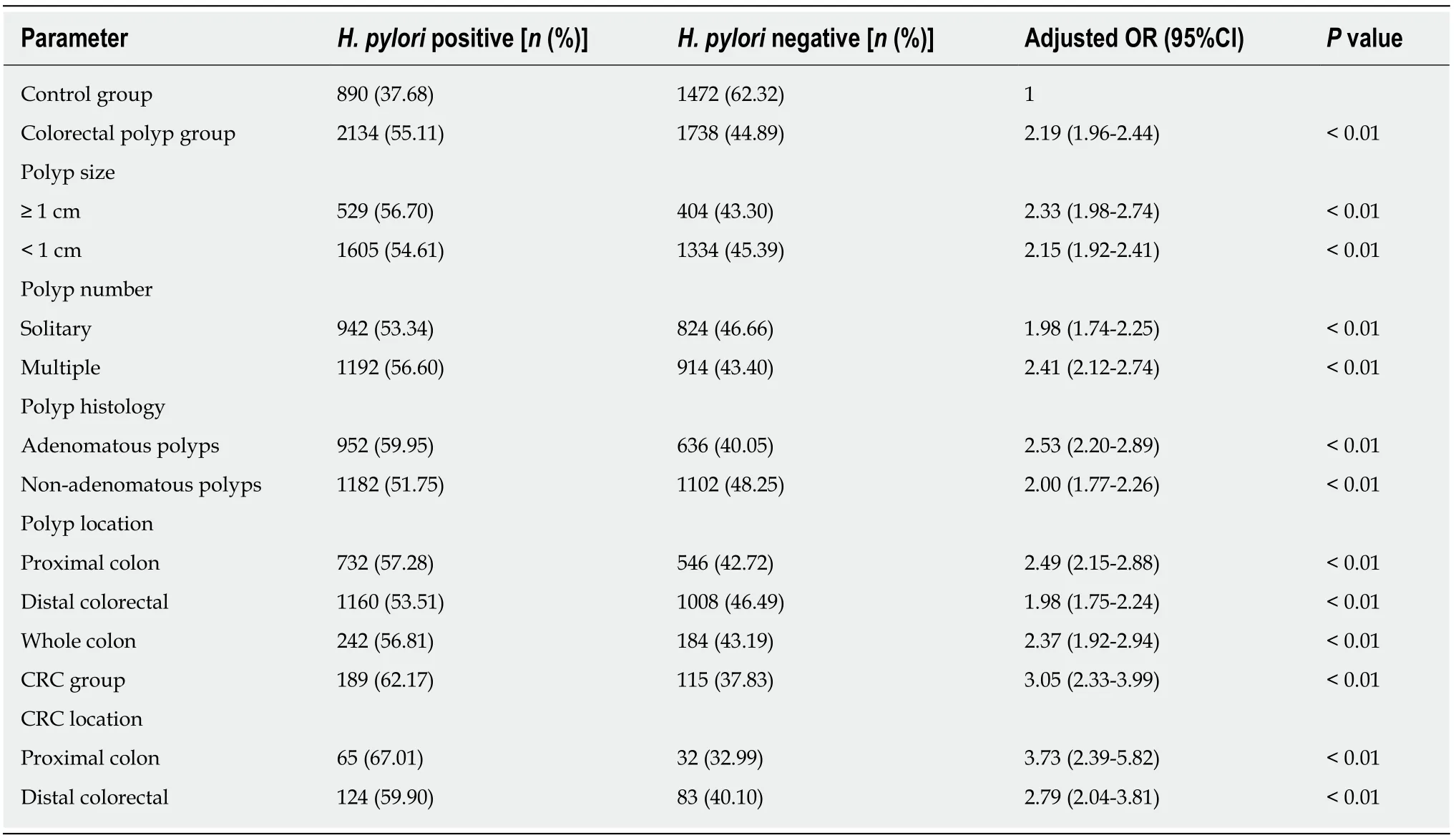
Table3 The association between Helicobacter pylori infection,colorectal polyps,and colorectal cancer,compared with the control group
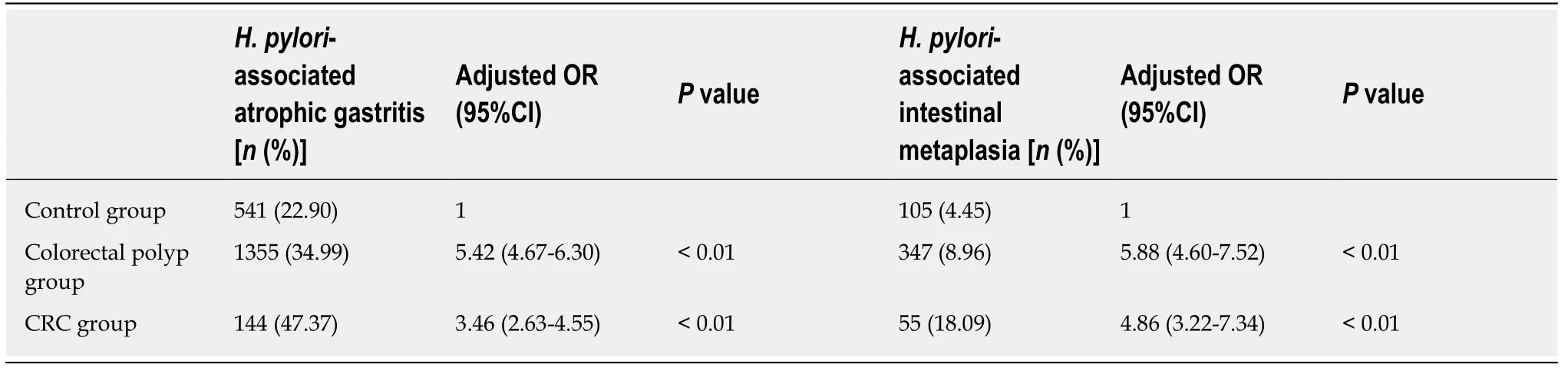
Table4 The association of Helicobacter pylori-associated atrophic gastritis or intestinal metaplasia with colorectal polyps and colorectal cancer,compared with the control group
ARTICLE HIGHLIGHTS
Research background
Gastric Helicobacter pylori (H.pylori) infection is a global public health problem.It is associated with chronic gastritis,gastroduodenal ulcer and gastric malignancies.The relationship between H.pylori infection and the risk of colorectal polyps and colorectal cancer (CRC) has also received extensive attention in recent years.
Research motivation
There is still no clear conclusion regarding the relationship between gastric H.pylori infection and the risk of colorectal polyps and CRC.
Research objectives
Our main purpose was to investig ate the correlation between gastric H.pylori infection and the risk of colorectal polyps and CRC,which is essential for the early screening and detection of colorectal precancerous lesions.
Research methods
A retrospective analysis of 6538 patients who underwent colonoscopy was conducted.The patients were divided into three groups:The CRC group,colorectal polyps group,and the control group.All subjects completed a 14C-urea breath test,bidirectional gastrointestinal endoscopy,and a biopsy on the same day.The characteristics of gastrointestinal endoscopy,pathology of gastritis,polyps and CRC,and the detection of H.pylori in the three groups were analyzed.
Research results
Patients with H.pylori inf ection were 2.19 times more likely to develop colorectal polyps and 3.05 times more likely to develop CRC than those who did not have H.pylori infection.The prevalence of H.pylori infection was higher in the multiple polyps group than in the solitary polyp group,and was also higher in the adenomatous polyps group than in the nonadenomatous polyps group.Additionally,we found that the incidence of H.pylori infection coexisting with atrophic gastritis or intestinal metaplasia was higher in patients with colorectal polyps and CRC than in the control group.The size and location of polyps,the histopathological characteristics and the location of CRC were not related to H.pylori infection.
Research conclusions
The incidence of colonic polyps and CRC in patients with gastric H.pylori infection and H.pyloriassociated atrophic gastritis or intestinal metaplasia was significantly higher than that in the normal population.Early and frequent colonoscopy is necessary to reduce the risk of colonic polyps and CRC in patients with H.pylori infection.The mechanism by which gastric H.pylori infection increases the incidence of colorectal polyps and CRC should be further studied.
Research perspectives
This study demonstrates that early colonoscopy screening and surveillance are necessary to reduce the risk of colonic polyps and CRC in patients with H.pylori infection.The future direction of research is to evaluate whether the eradication of gastric H.pylori can reduce the occurrence of colorectal polyps and CRC.Large-scale and long-term follow-up investigations are needed.
 World Journal of Gastrointestinal Oncology2020年5期
World Journal of Gastrointestinal Oncology2020年5期
- World Journal of Gastrointestinal Oncology的其它文章
- Espresso coffee,caffeine and colon cancer
- Perineural invasion as a prognostic factor in patients with stage l-lll rectal cancer-5-year follow up
- Gastric cancer with peritoneal metastases:Efficiency of standard treatment methods
- Perioperative chemotherapy for advanced gastric cancer-results from a tertiary-care hospital in Germany
- Neutropenia in colorectal cancer treated with oxaliplatin-based hyperthermic intraperitoneal chemotherapy:An observational cohort study
- Characterization and strong risk association of TLR2 del-196 to-174 polymorphism and Helicobacter pylori and their influence on mRNA expression in gastric cancer
