Interleukin-6-174G/C polymorphism is associated with a decreased risk of type 2 diabetes in patients with chronic hepatitis C virus
Cliviany Borges da Silva,Diego Alves Vieira,Luisa Freitas de Melo,Anna Luiza Soares Chagas,Adriana Dias Gomes,César Lúcio Lopes de Faria Jr,Rosângela Teixeira,Dulciene Maria de Magalhães Queiroz,Gifone Aguiar Rocha,Maria Marta Sarquis Soares,Juliana Maria Trindade Bezerra,Luciana Diniz Silva
Cliviany Borges da Silva,Sciences Applied to Adult Health Care Post-Graduate Programme,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Cliviany Borges da Silva,Diego Alves Vieira,Luisa Freitas de Melo,Anna Luiza Soares Chagas,Rosângela Teixeira,Luciana Diniz Silva,Outpatient Clinic of Viral Hepatitis,Instituto Alfa de Gastroenterologia,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Diego Alves Vieira,Luisa Freitas de Melo,Anna Luiza Soares Chagas,Medical undergraduate student,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Adriana Dias Gomes,César Lúcio Lopes de Faria Jr,Dulciene Maria de Magalhães Queiroz,Gifone Aguiar Rocha,Laboratory of Research in Bacteriology,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Rosângela Teixeira,Luciana Diniz Silva,Department of Internal Medicine,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Maria Marta Sarquis Soares,Division of Endocrinology,Department of Internal Medicine,Faculdade de Medicina,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Juliana Maria Trindade Bezerra,Epidemiology of Infectious and Parasitic Diseases Laboratory,Department of Parasitology,Institute of Biological Sciences,Universidade Federal de Minas Gerais,Belo Horizonte 30130100,Minas Gerais,Brazil
Abstract
Key words:Chronic Hepatitis C;Type 2 diabetes mellitus;Interleukin 6-174G/C gene promoter single nucleotide polymorphism;Blood hypertension;Healthy control subjects
INTRODUCTION
Globally,an estimated 422 million adults have diabetes mellitus[1]and around 71 million people are living with hepatitis C virus (HCV) infection[2,3].Over the past two decades,an accumulating body of scientific evidence has been linked type 2 diabetes mellitus to HCV infection[4-11].Given the high prevalence and the worldwide distribution of these two comorbidities,their association have an utmost impact on public health[1-3].
In pioneering study,in 1898,Naunyn firstly described an association between liver cirrhosis and diabetes mellitus that it is known as hepatogenous diabetes[12].Hence,cirrhosisper semight lead to glucose intolerance or diabetes mellitus.The prevalence of diabetes in cirrhotic patients with non-alcoholic fatty liver disease,cryptogenic,hepatitis C,and alcoholic hepatopathy ranges from 27.3% to 56.1%[13].Regarding the HCV and the non-alcoholic fatty hepatic disease we have to bear in mind that type 2 diabetes mellitus can be detected prior to the onset of hepatic cirrhosis[13-15]promoting a vicious cycle of hyperglycaemia causing a worsening metabolic state.Thus,altogether,glucose disturbed metabolism and HCV enhance the chronic inflammation and might interact as a reciprocal feed-forward loop[16-19].
The pathogenesis of type 2 diabetes mellitus encompasses both different degrees of insulin resistance and relative insulin deficiency[20,21].Although,some mechanisms underlying the modified glucose metabolism in HCV infection have been elucidated[22-24],several aspects remain unknown.Additionally,Chronic hepatitis C(CHC) patients with type 2 diabetes mellitus are likely to have an accelerated liver disease progression,i.e.,hepatic fibrosis,cirrhosis and hepatocellular carcinoma[25-28].Various factors can be involved in this interaction including direct viral effects and host factors,such as overweight and pro-inflammatory markers[16,17,29,30].Among the inflammatory markers,increased serum concentrations of interleukin-6 (IL-6) have been associated with insulin resistance,type 2 diabetes mellitus as well as advanced forms of liver disease in chronic hepatitis C infection[31-39].
Polymorphisms in the IL-6 gene,which may alter the expression of IL-6,have been investigated in the context of metabolic disease and CHC[31,32,34-42].The association between the single nucleotide polymorphism (SNP) of IL-6 located in the promoter region at the position-174G/C (rs1800795) and type 2 diabetes mellitus was first reported in United States Pima Indians and Spanish Caucasians[43].The C-allele was significantly associated with a decreased risk of type 2 diabetes.However,in further investigations these results have not been confirmed[34,39].In the setting of hepatitis C,IL-6 SNP polymorphisms have been associated with hepatic-and extra hepatic-related outcomes,such as cirrhosis,hepatocellular carcinoma and poor quality of life[31,32,40-42].Altogether,bothin vitroexperiments and clinical studies including healthy individuals have demonstrated that the presence of C allele is associated with lower levels of IL-6[44-46].The interrelationship between decreased concentration of this cytokine and IL-6-174 SNP is more pronounced in individuals carrying the CC genotype[44-46].
Because the host's immune response play an important role in extrahepatic manifestations in subjects chronically infected with HCV,even before the onset of hepatic cirrhosis,we hypothesized that IL-6-174G/G genotype,the IL-6 highproducer phenotype,may be associated to a high inflammatory profile that negatively affects the course of type 2 diabetes mellitus in these patients.Additionally,these factors may accelerate the liver fibrosis that also affects the insulin resistance.Thus,we evaluated the frequency of IL-6-174G/C SNP in patients chronically infected with HCV and in healthy subjects of the same ethnicity.Associations between type 2 diabetes mellitus (dependent variable) and demographic,clinical,nutritional,virological and,IL-6 genotyping data were also investigated in CHC patients.
MATERIALS AND METHODS
Participants
From March 2017 to July 2019,we prospectively included 260 adult patients with confirmed CHC diagnosis attending the Viral Hepatitis Outpatient Clinic,University Hospital,Belo Horizonte,Brazil.The control group consisted of 179 consecutive volunteer blood donors from the hemocenter of Felício Rocho Hospital (Hemoter -Clínica Romeu Ibrahim de Carvalho),Belo Horizonte,Brazil.The Viral Hepatitis Outpatient Clinic is an outpatient care ambulatory of a metropolitan tertiary teaching hospital that admits patients for the treatment of viral chronic hepatitis.All participants signed the informed consent form.The study was designed and conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Federal University of Minas Gerais/UFMG (ETIC 0404.0.203.000-10).
The exclusion criteria were:Pregnancy,breastfeeding,hepatic encephalopathy,HBV/HCV or HCV/HIV co-infection,current antiviral,use of non-steroidal antiinflammatory drugs or corticosteroids,and the presence of advanced disease such as chronic kidney disease,heart failure,chronic pulmonary disease,chronic pancreatitis and neoplasia,including hepatocellular carcinoma.
Clinical,biochemical,histological and radiological methods were performed for the diagnosis of the liver disease[47,48].The severity of liver dysfunction was assessed by the Child-Pugh-Turcotte score[49].Compensated cirrhosis was defined as the absence of variceal bleeding,ascites and oedema,jaundice or symptomatic encephalopathy on physical examination,and decompensated cirrhosis as the presence of any of these complications[50].The aspartate amino transferase to platelet ratio index[51]was calculated for each participant based on medical data.
The diagnosis of type 2 diabetes mellitus was based on documented use of oral hypoglycaemic medication or insulin;random plasma glucose levels ≥ 200 mg/dL in the presence of classic symptoms of hyperglycaemia or hyperglycaemic crisis;fasting plasma glucose ≥ 126 mg/dL on two occasions;2 h plasma glucose ≥ 200 mg/dL during oral glucose tolerance test or haemoglobin A1c ≥ 6.5% on two occasions[52].
Blood hypertension was diagnosed according to the 2018 European Society of Hypertension/European Society of Cardiology Guidelines[53].
An expert nutritionist carried out all nutritional evaluations.Weight and height were measured with a mechanical platform scale (FILIZOLA®,São Paulo,Brazil).Body mass index was calculated using the formula,Body mass index =weight/height2and the nutritional status of the patients were determined according to the World Health Organization criteria[54].Elderly individuals were classified according to the Lipschitz classification[55].
Furthermore,an in-person interview was conducted using instruments to assess the sociodemographic and clinical characteristics of the patients.Fifteen patients were not included:Twelve patients who had initially agreed to take part in this study failed to complete the questionnaires;three patients were excluded because blood sample was inadequate for genotyping.Two hundred and forty-five patients and 179 healthy subjects remained in the study.
All participants were from a similar socioeconomic level,as assessed by a previously validated questionnaire[56],which was based on income and educational level,as well as similar cultural habits.All subjects were natives of Minas Gerais,state in the south-eastern region of Brazil with the following ethnic background:56.0% of European ancestry,32.0% of African ancestry and 12.0% of Amerindian ancestry homogeneously present in each patient,irrespective of their phenotype[57].
Laboratory parameters
Blood samples were obtained from each subject after an overnight fasting for cytokine genotyping and biochemical assessments.Alanine aminotransferase,aspartate aminotransferase,gamma-glutamyl transpeptidase alkaline phosphatase,albumin,total bilirubin,prothrombin time and hemogram were evaluated by using Vitros®5600 (Ortho Clinical Diagnosis,Raritan,NJ,United States).
HCV genotype was determined by a line probe assay (VERSANT HCV genotyping assays;Bayer's Diagnostic Corporation,Tarrytown,NY,United States ) and viral load assessed by a commercial test (CobasTaqMan HCV test V.2.0;Roche Molecular Systems,Pleasanton,CA,United States).The assays were carried out according to the manufacturers' recommendations.
Aliquots of leukocytes and plasma were stored at -80 °C until analysis.
DNA extraction and genotyping of IL-6
DNA was extracted from the leukocytes with the QIAmp DNA mini kit (QIAGEN GmbH,Hilden,Germany) according to the manufacturer's recommendations.DNA concentration and purity were evaluated by spectrophotometry (NanoDrop Lite Spectrophotometer,Thermo Scientific,Waltham,MA,United States).DNA concentration was determined by absorbance at 260 nm and purity was assessed by the absorbance ratio at 260/280 nm.The DNA of the samples was stored at -20 °C before use.
IL-6-174G/C (rs1800795) genotyping was Taqman assayed by Real Time PCR System 7.500 (Applied Biosystems,Thermo Scientific,Foster City,CA,United States )by using oligonucleotide primers previously described by Fishmanet al[44].The sequence of synthetic probes and reaction conditions are described in Table 1.
Statistical analysis
The Hardy-Weinberg equilibrium of alleles at individual loci was assessed by twotailedχ2test or Fisher's exact test.
Data were analysed with SPSS statistical software package version 17.0 (SPSS Inc.,Chicago,IL,United States).Descriptive statistics were used to provide information regarding demographic,clinical,nutritional,virological,and genetic data.The Shapiro-Wilk test was used to evaluate whether the data were normally distributed.The asymptotic Pearson'sχ2test was used to compare the percentages.The Student'st-test or ANOVA was used to compare the means and the two-tailed Mann-WhitneyUtest was used for medians.
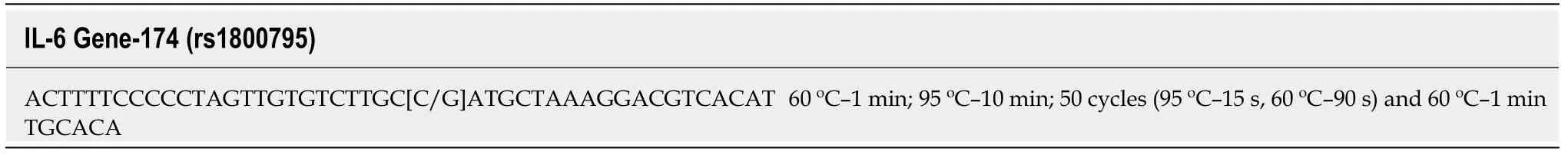
Table1 Probes and conditions used in the polymerase chain reaction to genotype interleukin 6 single nucleotide polymorphism at position-174 (rs1800795)
The associations of each variable including IL-6-174G/C,sex,increasing age,blood hypertension,nutritional status,liver fibrosis stage (chronic hepatitis and cirrhosis)with type 2 diabetes mellitus were tested in univariate analysis.All variables withPvalues < 0.20 were included in the full model of logistic regression.Odds ratio and 95%CI were used as an estimate of the risk.The Hosmer-Lemeshow test was used to assess the adequacy of the models.Variables that had missing data > 10% were not selected for the models of multivariate analysis.Pvalues ≤ 0.05 were considered significant.
RESULTS
Distribution of the IL-6 genotypes in CHC patients and controls (blood donors)
The frequencies of the IL-6 SNP did not differ between CHC patients and blood donors (Table 2).All alleles were in Hardy-Weinberg equilibrium in the control group(P> 0.95) and in the CHC patients (P> 0.38) as shown in Table 2.
Demographic and clinical characteristics of CHC patients
Among the 245 patients with CHC,94 (38.4%) had cirrhosis [Child-Turcotte-Pugh score A5,60 (63.8%);A6,21 (22.3%);B7,6 (6.4%);B8,4 (4.3%);B9,2 (2.1%);C10,1,(1.1%)].The mean age of the patients was 51.8 ± 11.4 years and 129 (52.7%) were males.
Cirrhosis was significantly more frequent (P= 0.03) in males (61.7%) than in females (38.3%).The patients with cirrhosis (53.5 ± 8.8 year) were older (P= 0.05) than those without (50.8 ± 12.7 year).Overweight tended to be more frequent (P= 0.08) in the CHC patients without (64.9%) than in those with cirrhosis (53.2%).
There was no significant difference (P= 0.11) in blood hypertension rate between CHC patients with cirrhosis (46.8%) and those without (35.8%).The frequency of type 2 diabetes did not differ (P= 0.33) between the two groups (24.5% in cirrhotic and 18.5% in non-cirrhotic patients).
HCV viral load and genotype in patients with CHC
There was no significant difference (P= 0.58) in the viral load between patients without [HCV-RNA log10 (IU)/mL,5.93 (interquartile range:5.46-6.39)] and those with cirrhosis [5.86:(interquartile range:5.34-6.20)].Also,the frequency of HCV Genotype 1 in patients without cirrhosis [109/126 (86.5%)] did not differ (P= 0.25)from that of patients with [61/78 (78.2%)].The quantification of viral load and HCV genotyping were available in 213/245 (86.9%) patients.
“哦,祝贺你。”李静说完用哈哈打圆场。但殷桃曾经磨刀霍霍,特幸福地说,“对,我感觉这是独特美妙的时辰。”
Characteristics of CHC patients with and without type 2 diabetes mellitus
Fifty-one (20.8%) patients had type 2 diabetes mellitus that was significantly more frequent in older patients (Table 3).The prevalence of blood hypertension was higher in type 2 diabetes mellitus than in those without the disease (Table 3).Lower frequency of IL-6-174G/C and C/C genotypes was observed in patients when compared to those without type 2 diabetes mellitus (Table 3).
Factors associated with type 2 diabetes mellitus in patients with chronic hepatitis C
In the univariate analysis,type 2 diabetes mellitus was associated with old age,blood hypertension,body mass index,and the GC and CC genotypes of IL-6-174 (Table 3).In the multivariate analysis,type 2 diabetes mellitus remained inversely associated with the GC and CC genotypes of IL-6-174 and positively associated with bloodhypertension (Table 4).
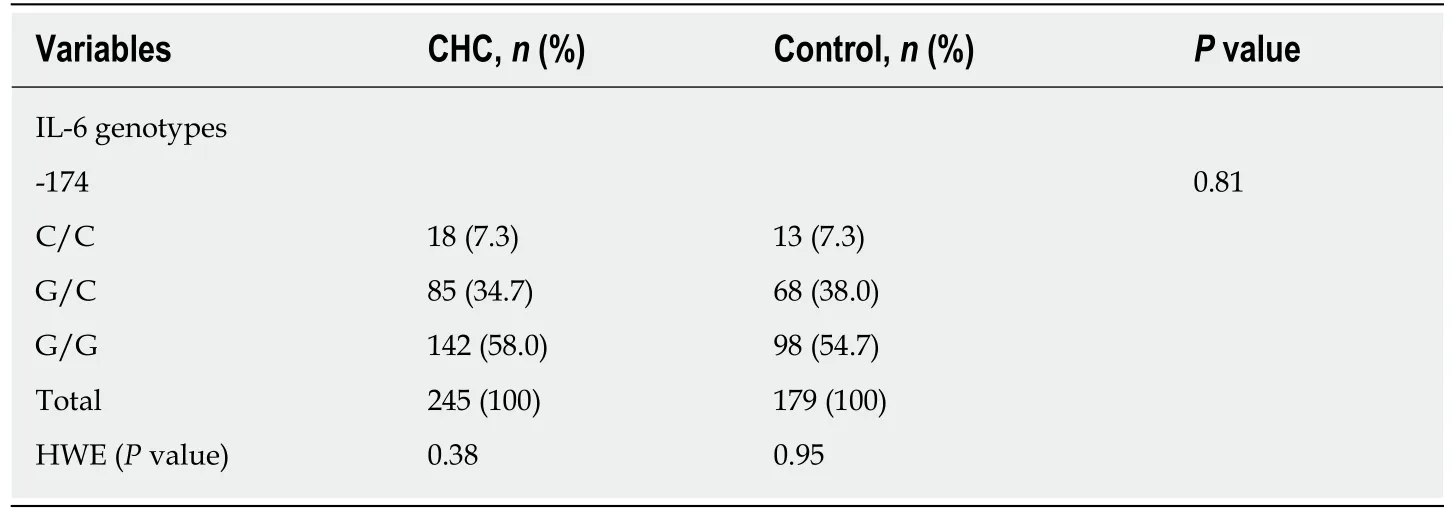
Table2 The interleukin genotype distribution in patients with chronic hepatitis C (n = 245) and healthy controls (n = 179)
DISCUSSION
Impaired glucose tolerance and type 2 diabetes mellitus have been reported to frequently occur in patients with chronic HCV infection independently of the hepatic disease severity[26,58,59].In consonance with the literature,we found a high prevalence of the type 2 diabetes mellitus in our patients[5,7,60,61].Although there is a sizeable body of scientific evidence linking glucose disturbed metabolism and hepatitis C,the biological mechanisms behind the concurrence of these conditions have not been completely clarified yet.
To the best of our knowledge,this is the first study to demonstrate that the GC and GG genotypes of IL-6-174 are inversely associated with type 2 diabetes mellitus in patients chronically infected with HCV.In the current study,CHC patients with type 2 diabetes mellitus had lower frequency GC and CC IL-6-174 genotypes compared to those without diabetes.Although,several investigations have shown that subjects carrying the GC and CC genotypes of IL-6 SNP had a decreased risk of type 2 diabetes mellitus[34-38],the association has not found by others[34,39],which may be due to the differences in the study designs and/or genetic ancestry of the populations.Concerning the chronic liver diseases,the IL-6-174G/C polymorphism has been associated with both fibrosis progression and hepatocellular carcinoma development[41,62,63]in patients with CHC.The majority of the studies has verified an association between the presence of the high producer genotype (GG) and poor outcome in patients with the hepatopathy[31,32,40,41,62,63].
Patients with CHC,with insulin resistance or type 2 diabetes mellitus are likely to have a more complicated course of the infection[24-27].Based on previous reports,it is important to keep in mind,if on the one hand insulin resistance is recognized as a risk factor for the progression of HCV-related liver disease[26-29,31,32],on the other hand,preceding HCV infection significantly increases the risk of developing type 2 diabetes mellitus[7].Additionally,diabetic patients are at an increased risk of acquiring HCV infection[64-66].Thus,this two-way interface,i.e.,the relationship linking HCV and type 2 diabetes mellitus,is possibly determined by complex and multifaceted interactions among the hepatitis virus,the environment and the host.Our current data show that neither different HCV genotypes nor viral load was significantly associated with type 2 diabetes mellitus.In this scenario,the host-related factors should be highlighted.
HCV infection and type 2 diabetes mellitus are associated with increased production of IL-6,a pro-inflammatory cytokine that plays a crucial role in viral induced liver damage[17,29,31-41,61,62],and may cause insulin resistance in adipose tissue,skeletal muscle and liver by inhibiting insulin signal transduction[67,68].Therefore,the results of the current study pointed to the role of IL-6 pathway in mediating both liver injury and disturbed glucose metabolism in CHC patients.Furthermore,even in the era of direct antiviral agents (DAAs),that has been causing dramatic changes in the treatment of CHC[69],the evidences of the current investigation should not be disregarded.Although most of the studies have demonstrated that HCV clearance by DAA treatment reverses or improves the insulin resistance[11,28,69,70],in a more recent investigation,the authors observed that successful hepatitis C virus treatment among patients with type 2 diabetes significantly reduces glycated haemoglobin shortly aftertreatment,but not for a long time[71].In addition,Hengstet al[72]demonstrated that DAA-induced viral clearance does not fully re-establish the modified cytokine and chemokine milieu in CHC patients[72].These evidences aligned with our results reinforce the role played by the immune-mediated mechanisms in the pathogenesis of insulin resistance and diabetes in HCV chronic hepatitis.
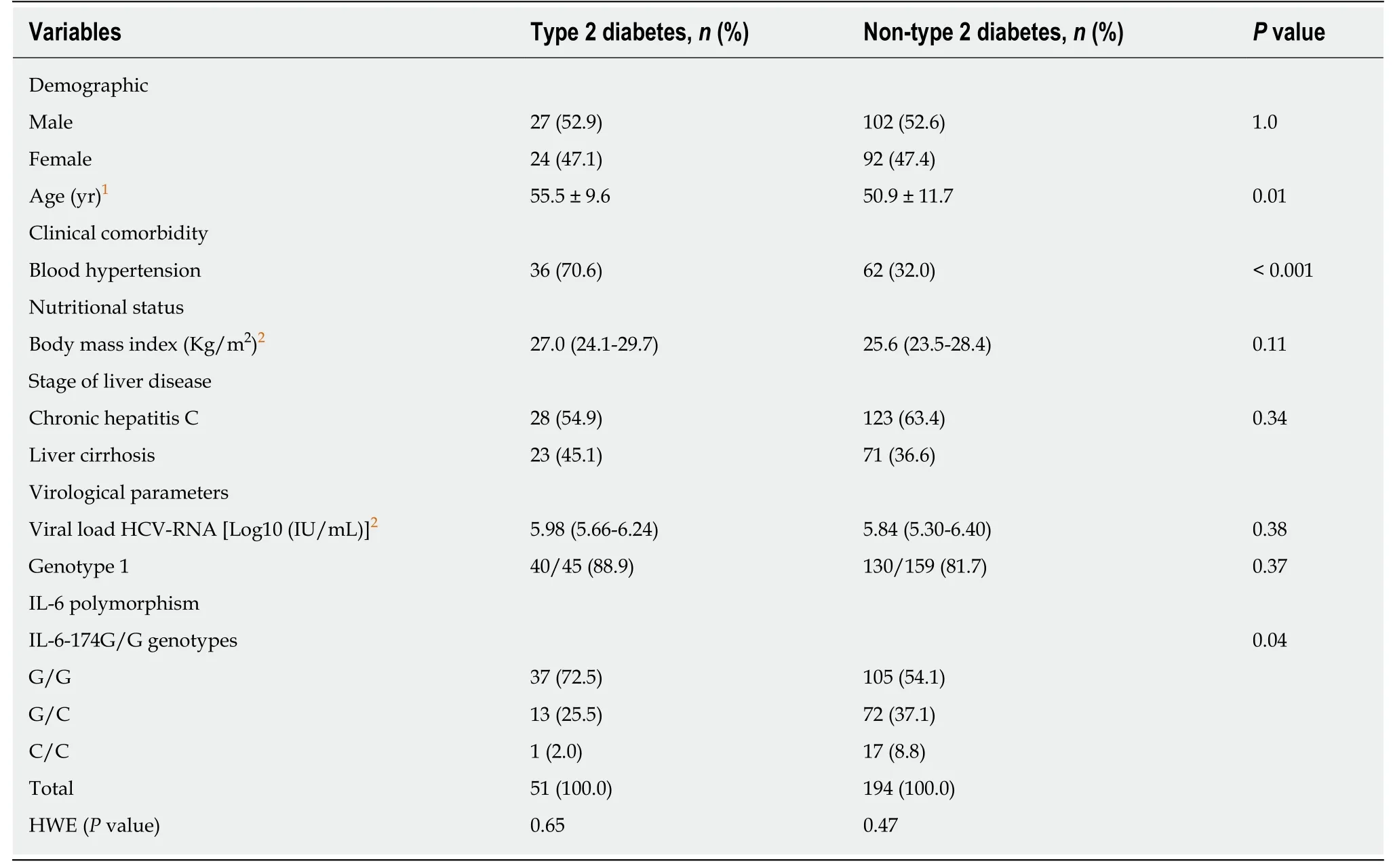
Table3 Demographic,clinical comorbidity,nutritional status,liver fibrosis stage,virological,cytokine genotyping data of the chronically hepatitis C virus-infected patients with (n = 51) and without type 2 diabetes (n = 194)
In the present study,in addition to IL-6 SNP,arterial hypertension was associated with type 2 diabetes mellitus.Studies have demonstrated that cardiovascular diseases,hypertension and diabetes are strongly correlated to each other[73].Their powerful relationship have also been observed in patients chronically infected with HCV[74,75].
The limitations of our study should also be considered.First,the subjects included were recruited from a referral centre and,consequently,may not be representative of all patients with CHC.Second,the cross-sectional nature of the investigation hindered the likelihood to recognize any cause-effect relationship between type 2 diabetes mellitus and IL-6 SNP in hepatitis C.Furthermore,another limitation is the lack of data on the serum concentrations of IL-6 of patients and controls;however,the functional significance of the studied polymorphism is well understood[44-46].
In the current study,we demonstrated for the first time that the IL-6-174G/C gene promoter polymorphism is inversely associated with type 2 diabetes mellitus in patients with CHC.This finding reinforces the need for additional investigations focusing on the biological mechanisms of diabetes mellitus in patients chronically infected with HCV.The identification of potential inflammatory mediators involved in the crosstalk between HCV and the pancreas-liver axis remains important issues that deserve further investigations.Moreover,better understanding of these processes may positively affect the management strategies for reducing the extra-hepatic manifestations and their negative impact on health status in CHC patients.
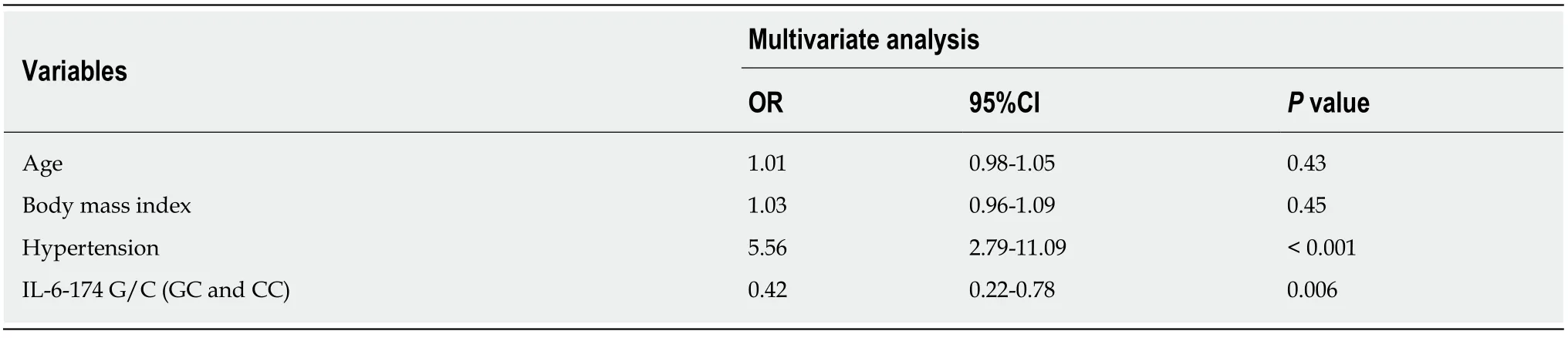
Table4 Variables associated with diabetes mellitus in patients with chronic hepatitis C
ARTICLE HIGHLIGHTS
Research background
Chronic hepatitis C (CHC) is associated with an elevated prevalence of type 2 diabetes mellitus.Although,some mechanisms underlying the modified glucose metabolism in hepatitis C virus(HCV) infection have been elucidated,several aspects remain unknown.Growing scientific evidence has suggested a role of pro-inflammatory immune response.Increased serum concentrations of interleukin-6 (IL-6) have been associated with insulin resistance,type 2 diabetes mellitus as well as advanced forms of liver disease in chronic hepatitis C infection.
Research motivation
Patients with CHC,with insulin resistance or type 2 diabetes mellitus are likely to have a more complicated course of the infection.Based on previous reports,it is important to keep in mind,if on the one hand insulin resistance is recognized as a risk factor for the progression of HCVrelated liver disease,on the other hand,preceding HCV infection significantly increases the risk of developing type 2 diabetes mellitus.Additionally,diabetic patients are at an increased risk of acquiring HCV infection.Thus,this two-way interface,i.e.,the relationship linking HCV and type 2 diabetes mellitus,is possibly determined by complex and multifaceted interactions among the hepatitis virus,the environment and the host.
Research objectives
The objectives of this study were therefore to investigate the frequency of IL-6-174G/C(rs1800795) single nucleotide polymorphism in CHC patients and in healthy subjects of the same ethnicity.Furthermore,the association between type 2 diabetes mellitus (dependent variable)and demographic,clinical,nutritional,virological and IL-6 genotyping data was also evaluated in patients chronically infected with HCV.
Research methods
Two hundred and forty-five patients with CHC and 179 healthy control subjects (blood donors)were prospectively included.Type 2 diabetes mellitus was diagnosed according to the criteria of the American Diabetes Association.Clinical,biochemical,histological and radiological criteria were applied to make the diagnosis and staging of the liver disease.IL-6-174G/C (rs1800795)genotyping was Taqman assayed by Real Time PCR System 7.500 by using oligonucleotide primers previously described by Fishmanet al[44].The Hardy-Weinberg equilibrium of alleles at individual loci was assessed by two-tailed chi-square test or Fisher's exact test.The associations of each variable including IL-6-174G/C,sex,increasing age,blood hypertension,nutritional status,liver fibrosis stage (chronic hepatitis and cirrhosis) with type 2 diabetes mellitus were tested in univariate analysis.All variables withPvalues < 0.20 were included in the full model of logistic regression.Odds ratio (OR) and 95%CI were used as an estimate of the risk.Pvalues ≤0.05 were considered significant.
Research results
Type 2 diabetes mellitus,blood hypertension and liver cirrhosis were observed in 20.8%(51/245),40.0% (98/245) and 38.4% (94/245) of the patients,respectively.The frequency of the studied IL-6 single nucleotide polymorphism did not differ between the CHC patients and controls (P= 0.81) and the alleles were in Hardy-Weinberg equilibrium (P= 0.38).In the multivariate analysis,type 2 diabetes mellitus was inversely associated with GC and CC genotypes of IL-6-174 (OR = 0.42;95%CI = 0.22-0.78;P= 0.006) and positively associated with blood hypertension (OR = 5.56;95%CI = 2.79-11.09;P< 0.001).
Research conclusions
In the current study,we demonstrated for the first time that the IL-6-174G/C gene promoter polymorphism is inversely associated with type 2 diabetes mellitus in patients with CHC.This finding reinforces the need for additional investigations focusing on the biological mechanisms of diabetes mellitus in patients chronically infected with HCV.
Research perspectives
The identification of potential inflammatory mediators involved in the crosstalk between HCV and the axis pancreas-liver remains important issues that deserve further investigations.Moreover,better understanding of these processes may positively affect the management strategies for reducing the extra-hepatic manifestations and their negative impact on health status in CHC patients.
 World Journal of Hepatology2020年4期
World Journal of Hepatology2020年4期
- World Journal of Hepatology的其它文章
- Geoepidemiologic variation in outcomes of primary sclerosing cholangitis
- Liver injury induced by paracetamol and challenges associated with intentional and unintentional use
- Comparison of four non-alcoholic fatty liver disease detection scores in a Caucasian population
- Combined endovascular-surgical treatment for complex congenital intrahepatic arterioportal fistula:A case report and review of the literature
- Inflammatory myofibroblastic tumor of the liver:A case report and review of literature
