Inflammatory myofibroblastic tumor of the liver:A case report and review of literature
Alexandra Filips,Martin H Maurer,Matteo Montani,Guido Beldi,Anja Lachenmayer
Alexandra Filips,Guido Beldi,Anja Lachenmayer,Department of Visceral Surgery and Medicine,Inselspital,Bern University Hospital,University of Bern,Bern 3010,Switzerland
Martin H Maurer,Department of Radiology,Inselspital,Bern University Hospital,University of Bern,Bern 3010,Switzerland
Matteo Montani,Institute of Pathology,Inselspital,University Hospital,University Bern,Bern 3010,Switzerland
Abstract
Key words:Inflammatory myofibroblastic tumor;Hepatic;Inflammatory;Anaplastic lymphoma kinase-expression;Case report;Review
INTRODUCTION
Inflammatory myofibroblastic tumors (IMT) are rare diagnostic findings and little is known about their etiology,pathogenesis and clinical behavior.First described in the lungs,this rare neoplasm can occur in various tissues and organs of the human body[1-4].Whereas IMTs were originally considered as inflammatory pseudo tumors,they are now recognized as true neoplasms in the histological typing of the soft tissue tumors classification of the World Health Organization with intermediate biological potential due to their ability to recur and to metastasize[1,4].IMTs of the liver (IMTL)are even more seldom and most published literature are case reports (Table 1) or small case series (Table 2).Most patients present with either abdominal pain or fever,in others the tumor is detected incidentally[5].A systemic inflammatory process with leukocytosis,elevated C-reactive protein (CRP) and other systemic inflammatory markers often accompanies the clinical presentation[3,5-11].Although this type of neoplasm can occur in individuals of all ages,it seems more common in children and young adults[4,12].The etiology of IMTL is unclear[4],but cytogenetic alterations suggest a clonal origin of theses lesions[3,4].Proof of diagnosis is difficult since no tumor markers are available and radiological findings are often not specific[6,8,13].Surgical resection is usually considered as the treatment of choice for these rare findings.IMTLs mostly present as solitary lesions with typical firm surfaces.Histopathologically,they can have three basic patterns,which are often combined in one tumor:(1) A myxoid/vascular;(2) Spindel cell;and (3) Hypocellular fibrous pattern[4].The tumor is frequently infiltrated by eosinophils,lymphocytes and plasma cells[4].Rearrangements of the anaplastic lymphoma kinase (ALK) gene locus are common in IMTs supporting its neoplastic origin.ALK overexpression and its positive immunohistochemical staining is reported in 50%-60% of the cases[14].Differential diagnoses of IMTL include metastatic sarcomatoid carcinoma,spindel cell sarcoma or melanoma,gastrointestinal stromal tumor,sarcoma,solitary fibrous tumor and calcifying tumors besides the large group of inflammatory pseudotumors[6].Although these lesions generally show a benign behavior,there is the possibility of malignant transformation and development of metastases[15,16].Some small case series of IMTs described the anatomic location,size and age as potential risk factors correlated with recurrence[2,13,17].In addition,ALK reactivity in the primary tumor was associated with a non-metastatic course of the disease[6].In the liver,a malignant transformation is extremely rare and only very few cases with local recurrence or metastases have been described[1,18].Due to the scarcity of this disease,the role of a preoperative biopsy is unclear,but because of the difficulty to obtain a proper histopathological diagnosis and the risk of malignant transformation,surgical resection is usually recommended whenever technically feasible[5,8,9,19,20].
We herein report the case of a 32-year-old woman who received an immediate hepatic resection for a large IMTL causing intermittent fever 4 mo postpartum.
CASE PRESENTATION
Chief complaints
A 32-year old woman presented herself to her family doctor with intermittent fever,unclear blood loss,malaise and pain in the right flank 4 mo postpartum.
History of present illness
The patient reported that the symptoms began 4 mo after she gave birth to her healthy child.She complaint about fatigue and right upper quadrant abdominal pain.She had recurrent episodes of fever up to 38.5 °C,but no jaundice or pruritus.
History of past illness
There was no significant history of past illnesses.
Personal and family history
Personal and family history was unremarkable.She gave birth to a healthy child 4 mo before she was treated at our institution.
Physical examination upon admission
Vital signs were within the normal range,body temperature was 38.5 °C.On examination,the patient had a right upper quadrant tenderness,without jaundice or hepatosplenomegaly.
Laboratory examinations
Urine and most blood analyses were without any pathological findings including a normal liver function and normal ferritin levels.While the white blood cell count was normal,CRP was elevated to 181 mg/L.The liver enzymes (aspartateaminotransferase 31 U/L,alkalic-aminotransferase 49 U/L) and cholestasis parameters (alkalic-phosphatase 466 U/L,y-glutamyl transferase 424 U/L) showed an increase while the serum bilirubin (6 μmol/L) stayed normal.
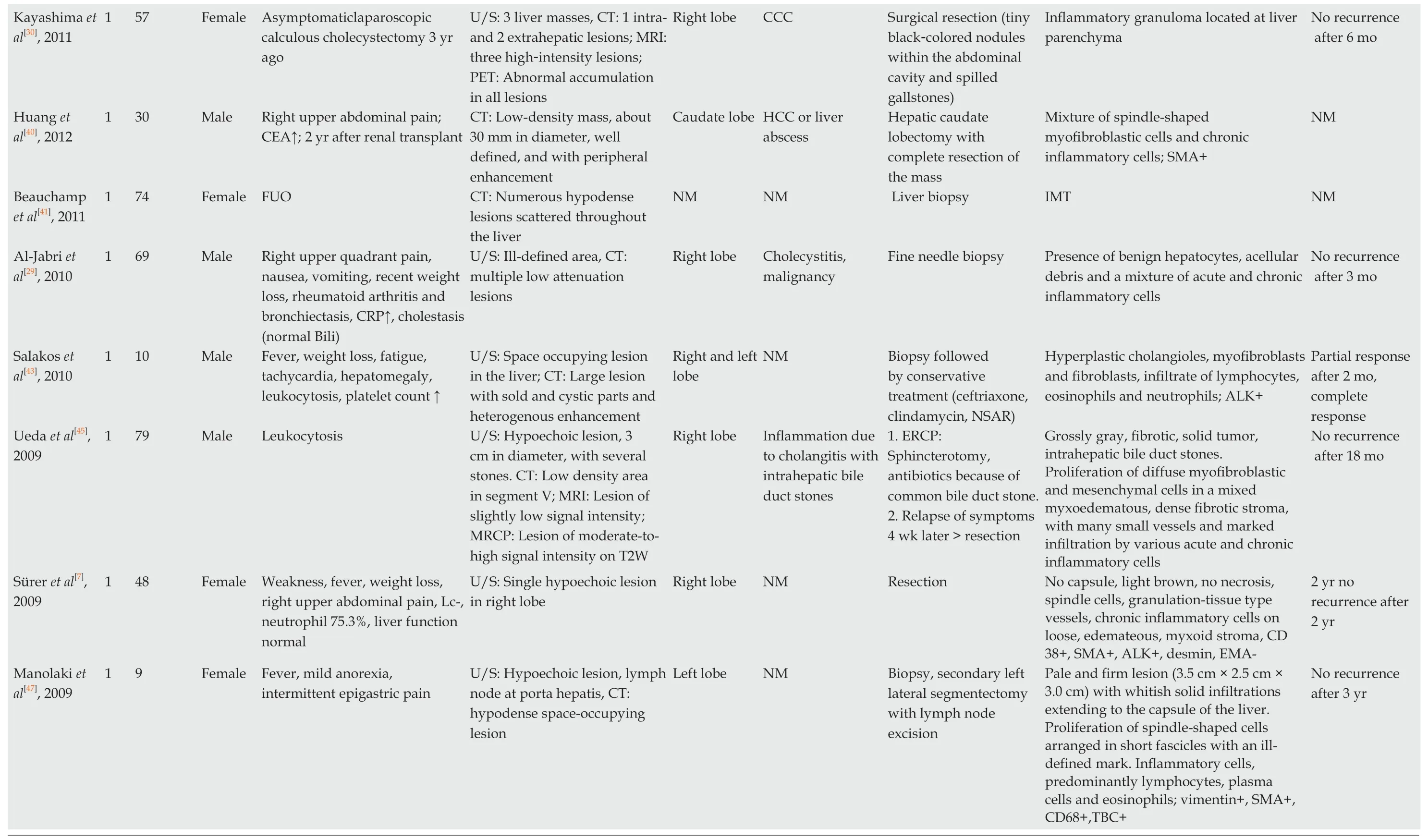
Imaging examinations
An ultrasound of the abdomen (Figure 1A) revealed a round,encapsulated liver lesion in segment IVa/b of unclear dignity,a non-contrast computed tomography of the abdomen ruled out urolithiasis,but confirmed the suspicious lesion of 8 cm in the liver as an incidental finding.The computer tomography (CT) and,same day magnetic resonance imaging (MRI) of the upper abdomen (Figure 1B-F) showed an 8 cm × 8 cm tumor in segment IVa/b of the liver suspected to be a liver adenoma.Additional serological tests for hepatitis,the tumor markers carbohydrate-antigen 19-9 and alpha-fetoprotein,and markers for echinococcosis were all negative.After discussion of the case in our interdisciplinary liver tumor board on the next day,we performed a positron emission tomography-computed tomography (PET-CT) which showed the known lesion as a metabolically active tumor resembling an inflammatory pseudotumor of the liver or a malignant tumor of unclear origin.No other lesions was detected in any of the performed scans.
Further diagnostic work-up
The pathologist macroscopically (Figure 2) described the size of the resected specimen as wedge-shaped and nodular,9.5 cm × 7.0 cm × 7.5 cm.The capsule of the liver was about unremarkable on one-half of the supplement.An area of 7.5 cm × 7.5 cm × 6.2 cm was sharply circumscribed,whitish/creamy and fibrous.No clearly definable capsule.The remaining liver tissue was inconspicuous and showed no further hereditary findings.The total weight of the tumor was 198 g.Immunohistochemistry showed a clear expression of cytoplasmic ALK and a weak expression of smooth muscle actin.Cytokeratin-PAN (CK Pan),Cytokeratin 18 (CK18),signal transducer and activator of transcription protein 6 (STAT6),Desmin,tyrosin-protein (C-kit),discovered on gastrointestinal stromal tumors 1 (DOG1),ETS related gene (ERG),family of calcium binding protein (S100) and SRY-related HMG-box 10 Protein(SOX10) showed no expression.The intra-tumoral immunoglobulin G4 (IgG4)-positive plasma cells were slightly increased,but displayed only a very small percentage of all plasma cells (Figure 3).The pathological diagnosis revealed an IMTL with no fibrosis and no malignancy.
FINAL DIAGNOSIS
The final diagnosis of the presented case is an IMTL.
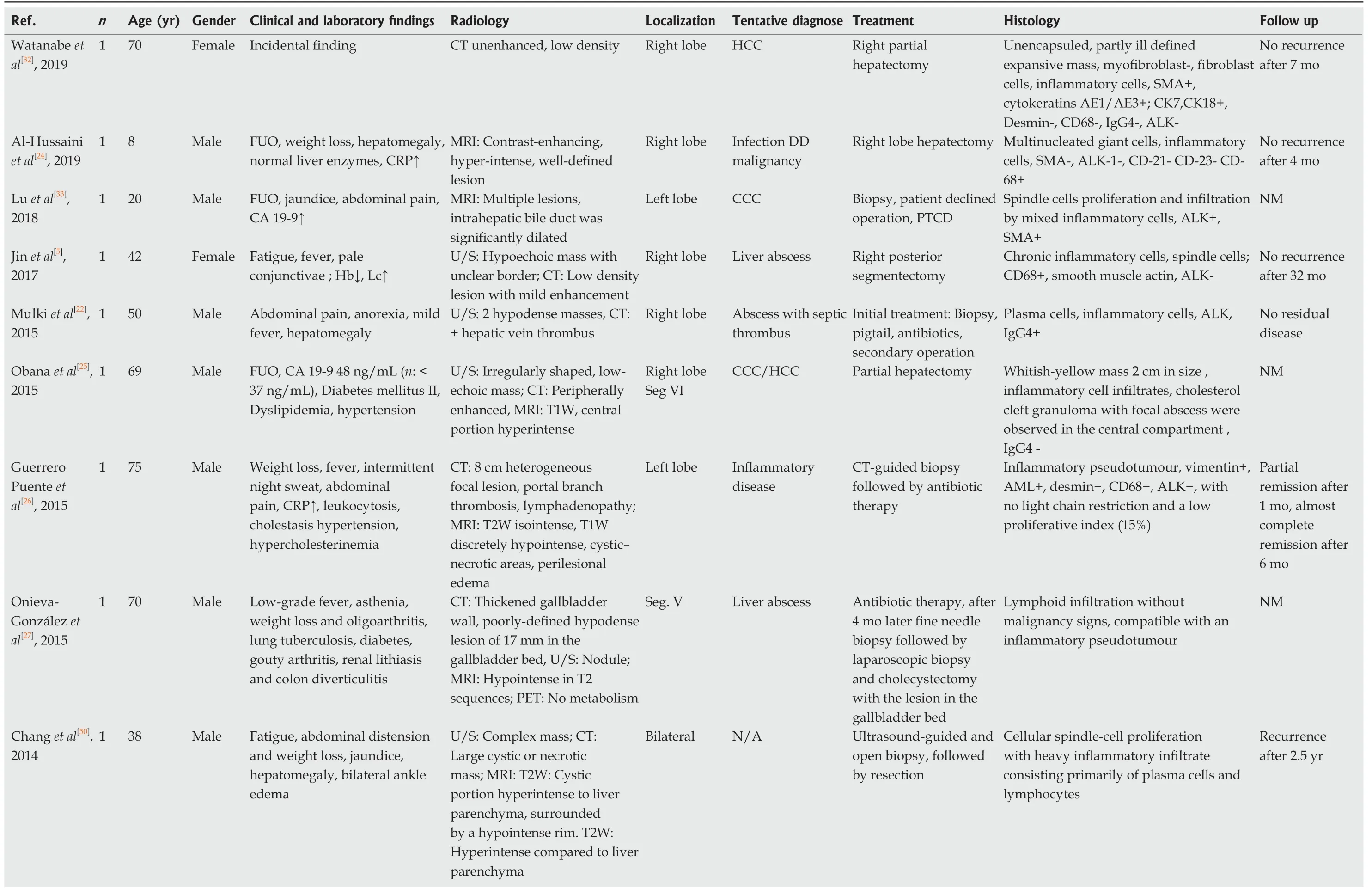
Table1 Case reports

NM NM NM No recurrence after 1 yr NM Bland spindle cell proliferation amidst small mature lymphocytes,numerous plasma cells,histiocytes,and few neutrophils. Spindle cells showed a storiform pattern with large areas of necrosis;cytokeratin (CAM 5.2)-,cytokeratin 5/6 -,actin-, CD34-,CD117-, DOG-1-, desmin-, CD68-,S100-,Pan-melanoma-.Spindle cells were negative for CD21, CD23,CD35, ALK-1.Epstein-Barr virusencoded small RNA in situ hybridization (EBER) showed large numbers of Epstein-Barr virus positive cells,including some spindle cells Tumor with fibrosis and partially necrotic tissue infiltrated by inflammatory cells, predominantly plasma cells,and also pigmented macrophages and granulocytes Dense hyalinised stroma and scattered,histiocytic and lymphocytic inflammation NM Grossly a non-encapsulated but well demarcated hepatic tumor with central necrosis of 11 cm in greatest dimension microscopically: Spindle myofibroblastic cells arranged in fascicles.Leukocytes, lymphocytes, plasma cells,SMA+ Percutaneous needle core biopsy > NM Left hemihepatectomy with partial excision of the adherent abdominal wall and diaphragm Surgical resection Surgical resection Antibiotics, later right hepatic lobectomy Fibrolamellar hepatocellular carcinoma or CCC Primary hepatic tumor Adenoma, focal nodular hyperplasia or HCC Pyogenic hepatic abscess Right lobe Segment IV Malignancy Left lobe Seg. VI Right lobe U/S: 18 cm mass with slightly echogenic center; MRI:Large mass with central dark area and some peripheral spokes; CT: Mass,20 cm × 17 cm × 18 cm, with extensions into the medial segment of the left hepatic lobe, hypervascular nodular area with enhanced density at the periphery and hypoattenuating showed density centrally U/S: Heterogeneous hypoechogenic tumor;CT: Contrast enhancing mass with irregular confluent non-enhancing areas in the center with a hypodense late enhancing rim and no washout in the late phase,MRI:In T1W hypointense borders,well defined without fatty components.T2W a heterogeneous slightly hyperintense lesion with an illdefined hyperintense rim U/S: 2 cm × 2.4 cm mass in the left hepatic lobe with associated biliary duct dilatation, MRI:atrophic left liver lobe with multiple strictures and distal duct dilatation. 2-cm lesion at the origin of the left hepatic duct Gastroscopy, CT lung and abdomen, MRI:3.3 cm lesion U/S and CT: Heterogenous rounded hepatic lesion of 7 cm in greatest dimension Chronic cough,right-upperquadrant pain, anorexia for 3 mo, leukozytosis, elevated platelet count tenderness,focus over epigastrium abdominal pain, renal transplant FUO CRP↑quadrant abdominal pain Male Female Moderate diffuse abdominal Female Right-upper-quadrant NM Female Fever,diaphoresis,right-upper-43 67 56 NM 23 1 1 1 1 1],],],You et al[35 2014 Durmus et ],2014 al[36 Wong et al[37 2013 Kruth et al[38 2012 Chablé-Montero et ],2012 al[39
CT:Computed tomography;MRI:Magnetic resonance imaging;FUO:Fever unknown origin;CRP:C-reactive protein;CCC:Cholangiocarcinoma;HCC:Hepatocellular carcinoma;PTCD:Percutaneous transhepatic cholangio drainage;NM:Not mentioned;U/S:Ultrasonography;Hb:Haemoglobin;LC:Leukocytes;TC:Thrombocytes;T1W:T1-Weighted;T2W:T2-Weighted;Chron Hep B:Chronic Hepatitis B;Seg:Segment;↑:Increase;↓:Decrease;WBC :Wight blood cells;SMA:Smooth muscle actin;ERCP:Endoscopic retrograde cholangiopancreatography.

Table2 Clinical studies of > 2 patients

CT:Computed tomography;MRI:Magnetic resonance imaging;FUO:Fever unknown origin;CRP:C-reactive protein;CCC:Cholangiocarcinoma;HCC:Hepatocellular carcinoma;PTCD:Percutaneous transhepatic cholangio drainage;NM:Not mentioned;U/S:Ultrasonography;Hb:Haemoglobin;LC:Leukocytes;TC:Thrombocytes;T1W:T1-Weighted;T2W:T2-Weighted;Chron Hep B:Chronic Hepatitis B;Seg:Segment;↑:Increase;↓:Decrease;WBC :Wight blood cells;SMA:Smooth muscle actin;ERCP:Endoscopic retrograde cholangiopancreatography.

Figure1 Imaging features within the liver lesion in segment IV.
TREATMENT
Due to the unclear situation with fever and the suspicion of a large adenoma or malignant tumor of the liver,an immediate surgical resection was performed.Intraoperatively,the solitary central lesion could be confirmed by intraoperative ultrasound,which also excluded additional liver lesions.An open resection of the liver segment IVa/b was performed achieving a negative resection margin.While no intra-operative complications occurred,the patient developed a bilioma,which had to be drained interventionally 7 d after the surgery accompanied by an endoscopic retrograde cholangiopancreatography with stent insertion.
OUTCOME AND FOLLOW-UP
The case was discussed postoperatively in our interdisciplinary liver tumor board to determine the postoperative management.While no adjuvant therapy was indicated,it was recommended to follow the patient clinically by MRI imaging every 3 mo after the surgery for the duration of at least one year.

Figure2 Postoperative macroscopic pathology of the inflammatory myofibroblastic tumors.
The patient returned to work and MRIs of the liver 3,6 and 12 mo after resection showed no local recurrence and no novel liver lesions.
DISCUSSION
We herein present and discuss the case of a 32-year-old woman who presented with a suspicious and symptomatic liver mass consequently diagnosed as IMTL.
IMTs of the liver are extremely rare findings that can sometimes mimic malignant lesions[6].In terms of demographics,the tumor seems to be more common in men than in women (M/F:1.5/1) with a mean age at diagnosis of 37 years[7].IMTL usually occur in the right liver lobe,in close proximity to the gallbladder or central biliary system[7,8].Typical clinical findings reported in the literature are fever,abdominal pain,lack of strength and weight loss[7],which all occurred in our case (intermittent fever,unclear blood loss,malaise and pain in the right flank) and led to the ultimate diagnosis.In addition to the fever,laboratory findings often suggest inflammation due to leukocytosis,neutrophilia and elevated CRP[5,6,8,10].More rarely,anemia and sometimes also elevated liver enzymes are reported[6].According to the clinical signs of infection,some individual cases were reported to be correlated with different active(virus) infections[5,18,19,21,22].In our patient,the antibody to Epstein-Barr virus was positive in the serological findings without any signs of an active Epstein-Barr virus infection.A clear association between IMT and infectious organisms seems to be doubtful since in most reported series,including our own case,no acid-fast organisms,fungi,parasites or bacteria could be identified in the tumor[10,19].
Radiological features of IMTLs are nonspecific and a definite radiological diagnosis seems to be impossible.Due to the small cases (Tables 1 and 2) we could see,that the tumor in ultrasonography mostly was hypoechogenic.An IMT may be suspected if a defined soft tissue mass and a heterogeneous enhancement with invasive or noninvasive growth are present on adjacent structures in CT or MRI[6,8,23].Not all patients underwent a MRI for diagnostic treatment,only in eight cases[17,24-29].Al-Hussainiet al[24]and Kayashimaet al[30]described a contrast-enhancing,hyper-intense well defined lesion without going into details.In four cases the lesion in T1W was mostly hypointense and T2W hyperintense[17,25,26,28].Despite its rarity,lack of diagnostic signs and symptoms,IMTL should not be ruled out as a differential diagnosis in liver lesions like focal nodular hyperplasia,hepatocellular adenoma,carcinoma and ecchinococcosis especially in young patients with normal tumor markers[7].In addition IMTL can sometimes mimic a liver abscess[22].Although many synonyms have been used for this lesion,including plasma cell granuloma,postinflammatory tumor,xanthomatous pseudotumor,inflammatory pseudotumor,and inflammatory fibrosarcoma[31],the new classification clearly suggests the term inflammatory myofibroblastic tumor of its suitable origin or organ,in our case an IMTL[4].
Due to the small number of cases worldwide (Tables 1 and 2),no clear diagnostic tests or radiographic features exist that help to make a definite diagnosis without a histopathological examination of the tissue[10].We performed a comprehensive literature search and studied the cases published during the last 10 years[5,7,17,24-30,32-47].There were more men affected than women.The most common localization of the tumor was on the right lobe of the liver.All patients in the described cases had at least an ultrasonography and/or a CT.In some cases,the diagnostic work-up was completed with MRI,MRCP or PET-CT.Due to the different radiological findings the tentative diagnose showed a large variation from liver abscess,inflammatory process and also malignancy.

Figure3 Postoperative microscopic pathology of the inflammatory myofibroblastic tumors.
In the gross examination of the resected specimen,most findings showed the similar finding of a well-demarcated,unencapsulated,yellow-whitish mass.Histologically infiltrations of chronic inflammatory-cells like lymphocytes,neutrophils,eosinophils,and macrophages were often described.Whenever immunohistochemical analyses were performed,ALK expression showed a similar distribution.The performed treatment of the different cases varied according to the initially suspected diagnose.In summary,more patients were treated conservatively,although there is no clear indication for such a treatment.Surgical resections were performed according to the size and location of the suspected tumor and varied from small atypical resections to major hepatectomies.In most of the cases the definite histology report of the resected specimen then showed the diagnosis of an IMTLUnfortunately,follow-up was not described in all published cases.Except for one reported recurrence after 2.5 years,most patients stayed tumor-free during a followup ranging from X-Y months[48].
Surgical resection is usually recommended so that a proper pathological work-up can be performed and malignancy can be ruled out.Nevertheless,several different treatment strategies have been published including conservative approaches with steroids,high-dose steroids,radiation and chemotherapy[6-8,11].Interestingly,one case with a spontaneous regression has also been reported[17].A typical pathological finding is that the IMTL's are unencapsulated.They are usually solid or gelatinous on the intersection and have a white color.Hemorrhage,calcification or necrosis are rarely described[6,12],similar to the pathological findings in our case.As described by Elpeket al[6],chromosomal translocations leading to the activation of ALK can be detected in IMTLs.Although immunohistochemistry for ALK expression in immunohistochemistry can reliably predict the presence of ALK gene rearrangement,its prognostic relevance is still unclear[14,49].IMTLs differ from IgG4-related liver disease in terms of ALK expression,low IgG4 positive cell infiltration,and lack of obstructive phlebitis[6].
The natural course of IMTL without curative surgical therapy is unclear.To date,only a few cases have been described in which patients had local recurrence or metastases after liver resections[15,16,48].Due to the small numbers published worldwide,no recommendations for the follow-up are available and patients is treated according to the decisions made in the local interdisciplinary tumor boards.In our case,the finding of the pseudotumor was 4 mo postpartum.Due to the rather large size of the lesion it was considered an advanced lesion.The pregnancy may have masked general symptoms such as nausea,vomiting,and abdominal pain.So far,only one case of newly diagnosed IMTL has been reported during pregnancy[18].
CONCLUSION
In summary of the literature and with the experience from our own recent case,complete surgical resection of a suspected IMTL should be the preferred treatment of choice in order to rule out malignancy,avoid long-term medical treatment and to be able to recommend an appropriate follow-up for the patient.
 World Journal of Hepatology2020年4期
World Journal of Hepatology2020年4期
- World Journal of Hepatology的其它文章
- Geoepidemiologic variation in outcomes of primary sclerosing cholangitis
- Liver injury induced by paracetamol and challenges associated with intentional and unintentional use
- Interleukin-6-174G/C polymorphism is associated with a decreased risk of type 2 diabetes in patients with chronic hepatitis C virus
- Comparison of four non-alcoholic fatty liver disease detection scores in a Caucasian population
- Combined endovascular-surgical treatment for complex congenital intrahepatic arterioportal fistula:A case report and review of the literature
