Optimal proximal resection margin distance for gastrectomy in advanced gastric cancer
Amy Kim, Beom Su Kim, Jeong Hwan Yook, Byung Sik Kim
Abstract
Key words: Stomach neoplasms; Gastrectomy; Margins of excision; Prognosis;Recurrence
INTRODUCTION
Although the worldwide gastric cancer incidence has been declining over the past few decades, gastric cancer remains the third leading cause of cancer mortality[1-3]and surgery is still the mainstay curative treatment for gastric cancer patients[4]. While radical surgery with adequate resection of the stomach and lymph nodes is the prime focus of treatment, quality of life after surgery has been receiving increased attention due to improvements in the postoperative survival of gastric cancer patients. Several studies have revealed that subtotal gastrectomy leads to better nutrition and quality of life after surgery than total gastrectomy (TG)[5,6], and a recent report showed the relationship between the remnant volume of the stomach and nutritional status after surgery[7]. Thus, surgeons should consider these factors when determining the optimal extent of resection.
Bozzettiet al[8]reported that a proximal resection margin (PRM) of at least 6 cm should be obtained for tumors invading the serosa to ensure an infiltration-free margin. However, this was published back in 1982 and may not accurately reflect the current state of gastric cancer treatment where values such as function preservation,nutrition, and quality of life are emphasized. The 2014 Japanese gastric cancer treatment guidelines (Version 4) suggest that a gross margin of at least 3 cm should be obtained for T2 or deeper tumors with Bormann type 1 or 2, and 5 cm should be obtained for Bormann type 3 or 4 tumors[9]. The National Comprehensive Cancer Network recommends a PRM of > 4 cm for a safe microscopic margin[10]. These guidelines do not specify the clinical studies, making it difficult to assess the reliability of the suggested PRMs.
In 2014, it was reported that as long as negative margins were obtained by intraoperative frozen-section examination, PRM is not related to patient survival or local recurrence[11]. However, a 2017 study revealed that PRM is an independent prognostic factor for the overall survival (OS) of gastric cancer patients and a PRM of at least 2.1 cm should be obtained[12]. Several other studies have examined the relationship between the PRM and the prognosis of patients with gastric cancer, but the results were inconsistent[13-18], particularly for patients with advanced gastric cancer (AGC).
This study is based on extensive retrospectively collected data and aims to investigate the relationship between PRM and the recurrence-free survival (RFS) or OS after surgery and thus determine the optimal PRM for patients with AGC.
MATERIALS AND METHODS
Patients
Between June 2004 and December 2007, 1518 patients in total underwent total or distal gastrectomy (DG) with curative intent for AGC at the Division of Stomach Surgery in Asan Medical Center. Patients with stage IV AGC or evident gross residual tumor were observed intraoperatively and those who underwent palliative gastrectomy were not included in the study. We excluded gastroesophageal junction cancer(Siewert I or II) patients, patients with a history of previous stomach surgery, patients who underwent neoadjuvant chemotherapy and patients whose pathologic report confirmed fewer than 15 lymph nodes retrieved. Cases in which grossly positive resection margins were observed, and those where the final biopsy reports confirmed a positive resection margin were excluded. We also excluded cases without data for PRM.
To evaluate patient characteristics, we collected data on the sex, age, preoperative body mass index (BMI), history of previous operations on the stomach, medical history of hypertension (HTN), diabetes mellitus (DM), American Society of Anesthesiologists (ASA) score, history of smoking, preoperative value of CEA, CA 19-9 and CA 72-4, tumor location, type of surgery (TG or DG), and type of reconstruction. Clinicopathologic outcomes included the Borrmann classification of the tumor, the number of synchronous tumors in the stomach, tumor size, depth of invasion, number of lymph nodes collected (CLN), number of positive lymph nodes(PLN), histology according to differentiation, status of lymphovascular invasion (LVi)and Perineural invasion (PNi), distance of the tumor from the PRM and distal resection margin (DRM), TNM stage based on the American Joint Committee on Cancer (AJCC) staging Manual 7thedition, recurrence status, and survival.
The extent of resection was determined according to the surgeon's preference,primarily based on the Japanese gastric cancer treatment guidelines. The tumor location was defined according to equally divided sections for the upper-third,middle-third, and lower-third of the stomach. For multiple cancers, the location was defined based on the most proximal tumor. The distances of the PRM and DRM were defined as the shortest distance from the most proximal or distal end to each resection line, measured on formalin-fixed surgical specimens by pathologists. Recurrence was classified as locoregional (anastomosis site, remnant stomach, gastric bed, regional lymph nodes, adjacent organ, or paraaortic lymph node), hematogenous (distant organs), peritoneal (peritoneal seeding or Krukenberg's tumor), distant lymph nodes(extra-abdominal lymph nodes), and mixed. The main patterns of recurrence were determined based on the site at the time of diagnosis.
This study was approved by the Institutional Review Board of Asan Medical Center and the University of Ulsan College of Medicine (No. 2019-1036).
Statistical analysis
Statistical analysis was performed using SPSS version 21.0 (SPSS, Inc., Chicago, IL,United States). To analyze the demographics and clinicopathologic features depending on different PRM categories, one-way ANOVA and Fisher's exact test were used for continuous and categorical variables, respectively. Kaplan-Meier survival analysis and Cox proportional hazard analysis were performed to assess the impact of PRM on RFS and OS. AnyPvalue < 0.05 was considered statistically significant. The study was reviewed by a biomedical statistician from Department of medical statistics, University of Ulsan College of Medicine.
RESULTS
Table 1 summarizes the patients' baseline demographics and clinicopathologic characteristics. There were 859 patients who underwent DG and 659 patients who underwent TG. The median age at the time of operation was 60 and 57 in the two groups, respectively. In the DG group, there were 626 patients (72.9%) with tumors located in the lower third of the stomach. In the TG group, 586 (88.9%) had cancer in the upper or middle third of the stomach. After DG, anastomosis was performed using the Billroth I reconstruction method for 71.0% of patients, Billroth II for 15.9%and Roux-en-Y gastrojejunostomy (RYGJ) for 13.0%.
The median PRM distance was 4.8 cm and 3.5 cm in the DG and TG groups,respectively. There were 220 (25.6%) and 251 (38.1%) cases of recurrence during the follow-up period of 59 (0-127) and 58 (0-129) months in each group.
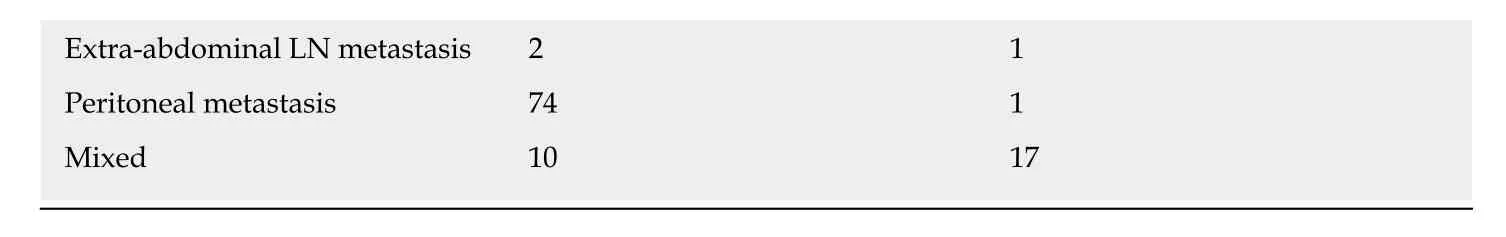
Patient cohorts in the DG and TG groups were subdivided into different groups according to the length of the PRM: ≤ 1.0 cm, 1.1-3.0 cm, 3.1-5.0 cm and > 5.0 cm.Tables 2 and 3 present the clinicopathologic factors in the different PRM subgroups.In both the DG and TG groups, there were no significant differences in age, sex, T stage, or N stage according to the PRM distance. Among patients who underwent DG,the tumor location (P< 0.001), reconstruction type (P= 0.004) and tumor size (P=0.004) differed between the PRM subgroups. Additionally, there were more undifferentiated tumors (P= 0.023) and perineural invasion (P= 0.010) in the PRM ≤ 1 cm subgroup. In the TG group, there were statistical differences in the tumor location(P< 0.001), tumor size (P< 0.001), proportion of linitis plastica (P< 0.001), and perineural invasion (P= 0.002) between the PRM subgroups. There were no significant differences in the recurrence rate or local recurrence rate according to the PRM distance in either the DG or TG group.
Kaplan-Meier analysis was performed to assess the impact of PRM distance on RFS and OS. In the DG group, the mean RFS was 83.8, 90.9, 96.0, and 94.9 mo with a fiveyear RFS of 35.3%, 41.8%, 47.0%, and 41.0% in the PRM ≤ 1 cm, 1.1-3.0 cm, 3.1-5.0 cm,and > 5 cm subgroups, respectively. In the TG group, the mean RFS was 73.8, 78.5,88.3, and 83.7 mo with a five-year RFS of 42.2%, 33.0%, 45.9%, and 39.3%, respectively.Neither the DG nor TG group showed statistical differences in either RFS or OS according to the PRM distances (Figures 1 and 2).
Univariate and multivariate analyses were performed to investigate the impact of the PRM distance and other factors on OS (Tables 4 and 5) and RFS (Tables 6 and 7)using the Cox proportional hazard model. Variable selection for multivariate analysis was done using the backward elimination method with a likelihood ratio test. This revealed that among patients who underwent DG, a higher T stage (T3;P= 0.003, T4;P< 0.001) and N stage (N2, N3;P< 0.001) were associated with worse RFS. Other risk factors included older age (P= 0.012) and reconstruction type; Billroth II (P= 0.016)and RYGJ (P= 0.003) reconstructions resulted in worse RFS than Billroth I reconstruction (Table 6). In the TG group, higher T stage (T4;P= 0.014) and N stage(N2;P= 0.001, N3;P< 0.001) were risk factors associated with RFS. Older age (P=0.032), linitis plastica (P< 0.001) and the presence of lymphovascular invasion (P=0.013) were also associated with worse RFS (Table 7). However, neither group showed a significant difference in either RFS or OS according to the distance of the PRM.
DISCUSSION
It is widely accepted that sufficient resection margins should be achieved for curative resection of gastric cancer. The optimal length for the proximal margin is often suggested to be at least 4-6 cm[8-10]. Over the years, surgical skills and technologies have developed and fields of minimal, less invasive approaches are quickly growing.Guidelines suggest laparoscopic gastrectomy should be performed for early gastric cancer (EGC) in the distal third of the stomach[9]and laparoscopic TG was recently demonstrated to be safe and feasible for EGC. Moreover, there are ongoing trials and studies for laparoscopic approaches in advanced cancer, particularly in eastern countries. However, surgeons still abide by conventional rules and try to achieve the recommended margin length, even in difficult conditions.
Several studies are rooted in this discrepancy in the appropriate PRM distance. In 2006, Haet al[19]reported that PRM had no significant influence on the prognosis of EGC patients; however, a PRM length of > 3 cm improved the survival rates in AGC patients. Squireset al[15]reported their findings from a 2015 study based on 465 patients who underwent curative-intent gastrectomy for distal gastric cancer. Their results indicated that a proximal margin distance > 3 cm is associated with better OS and RFS in stage I disease, whereas the proximal margin distance did not significantly improve prognosis in either stage II or III disease. The authors concluded that a proximal margin of > 3 cm is optimal for distal gastric cancer. Wanget al[12]reported that a proximal margin of 2.1-4.0 cm and 4.1-6.0 cm should be obtained for patients with solitary- and infiltrative-type tumors, respectively, for better prognoses. In 2017,based on 974 patients with gastric and esophago-gastric junction cancer, Bissolatiet al[17]reported that a resection margin, either proximal or distal, that is < 2 cm for T1 cancer and < 3 cm for T2-4 cancer is associated with resection margin involvement,which was demonstrated in previous literature to have a negative prognosticimpact[20-24]. However, Kimet al[13]reported in 2014 that the length of the proximal margin did not affect the OS or local recurrence and several subsequent studies have arrived at similar conclusions[11,14,18].
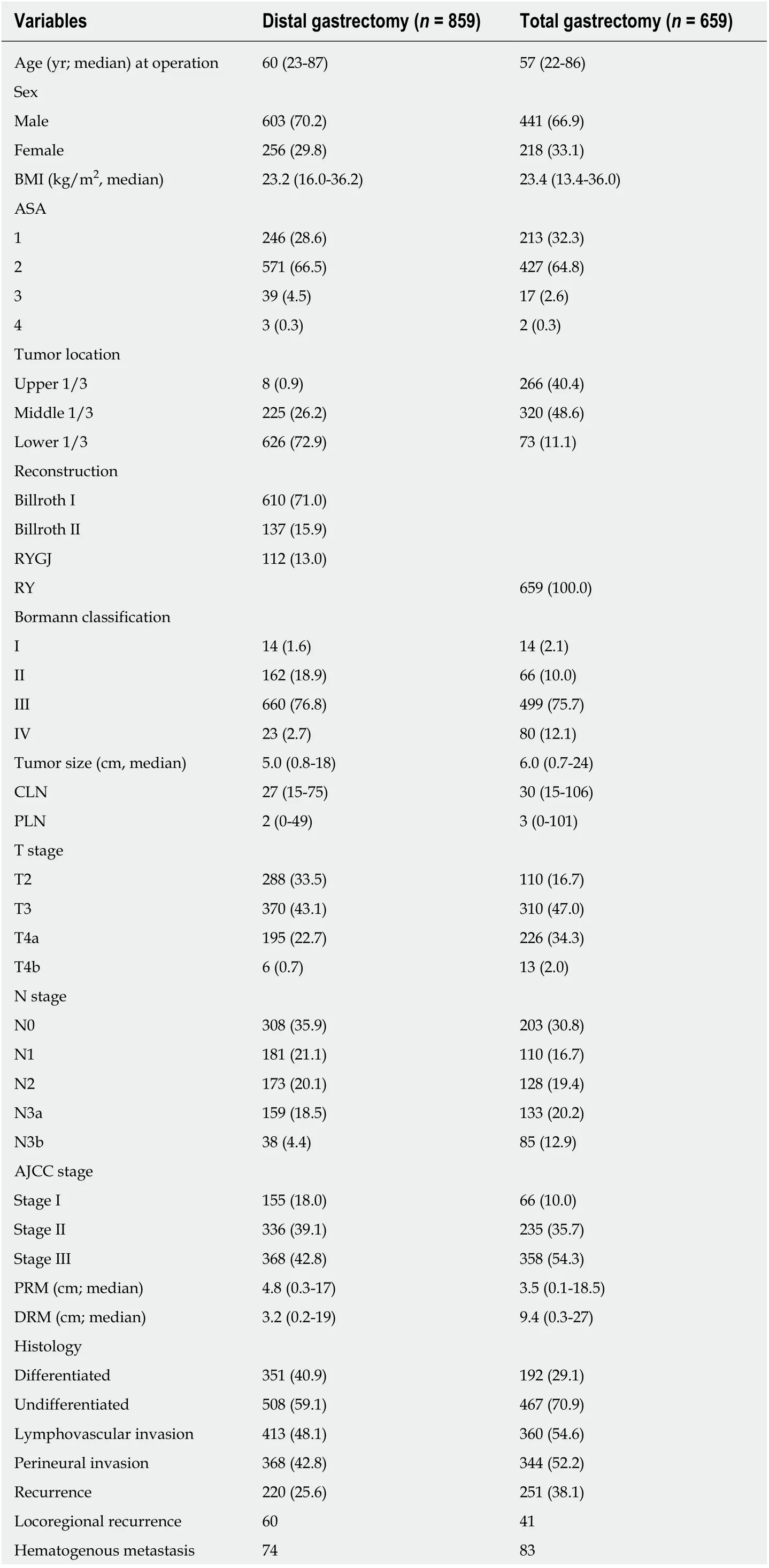
Table 1 The basic demographics and clinicopathologic characteristics of patients whounderwent distal and total gastrectomy with curative intent for gastric adenocarcinoma, n (%)
RYGJ: Roux-en-Y gastrojejunostomy; RY: Roux-en-Y esophagojejunostomy; CLN: Total number of collected lymph nodes; PLN: Total number of positive lymph nodes; PRM: Proximal resection margin; DRM: Distal resection margin; AJCC: American Joint Committee on Cancer.
The conclusions regarding the safe length of PRM, particularly for AGC patients,are not consistent even among recent papers. Thus, we designed a large-scale study to determine the optimal length of the PRM for patients with AGC. Cross-tabulation analysis with our data showed that the incidence of recurrence or local recurrence according to the distance of the PRM did not differ (P> 0.05) in patients who underwent DG or TG for AGC. We performed Kaplan-Meier survival analysis to assess the effect of the PRM distance on RFS and our results showed no statistical difference in RFS between the PRM subgroups. Multivariate analysis using the Cox proportional hazard model revealed consistent results. Although previous reports do not agree on the safety of short resection margins, particularly in AGC, our results demonstrate that the distance of the PRM did not affect the prognosis of AGC patients who underwent curative gastrectomy.
Our multivariate analysis of influential factors in RFS and OS for patients who underwent DG showed significant differences between different reconstruction methods; this is inconsistent with previous literature. Billroth I was the most preferred reconstruction method after gastrectomy for gastric cancer patients at our institution.When a tumor involved pylorus or the stomach stump was too short for gastroduodenostomy, Billroth II or RYGJ was applied. Therefore, there is a chance that cases with B-II and RYGJ anastomosis were associated with larger and more progressed tumors. Another possible reason is that because Billroth I is the most preferred method in our institution, surgeons were more comfortable with the procedure, resulting in better outcomes. Although there is no consensus, a number of studies reveal more gastric stump cancer in patients who underwent Billroth II reconstruction rather than Billroth I after gastrectomy either due to carcinoma or benign lesions[25-27]. There is also an RCT from Japan that shows more hematogenous recurrence in B-II compared to B-I[28]. This is an important result that warrants further investigation with a careful design, taking many factors such as recurrence patterns,recurred time after surgery, histology of the initial tumor, and many other factors into consideration.
There is a limitation in the retrospective design of this study. Another limitation is that the length of the resection margin used in the study may not accurately portray the gross distance we observe intraoperatively. We used the PRM as described on the pathologic report, which was measured under formalin fixation. We chose to use the pathologic report because measurements from the operation room are expected to be less consistent depending on the measured time after resection or in cases with indistinctive tumor margins such as linitis plastica. Additionally, for TG, we used circular staplers that produce doughnut specimens that are not added to the length of PRM, so the actual PRM may be few millimeters longer than measured.
In conclusion, the distance of PRM is not a prognostic factor for AGC patients; it does not affect the incidence of recurrence or local recurrence. A greater PRM distance was not associated with better survival outcomes and a distance of < 1 cm did not correlate with worse OS or RFS.
敏捷型的BIM团队,同时响应内部的需求,包括技能交换、工时轮换、任务转包。团队负责人须时刻响应内部沟通企图,冲刺阶段全程陪同完成。最大程度响应团队对于技能提升、办公环境、加班待遇的需求。
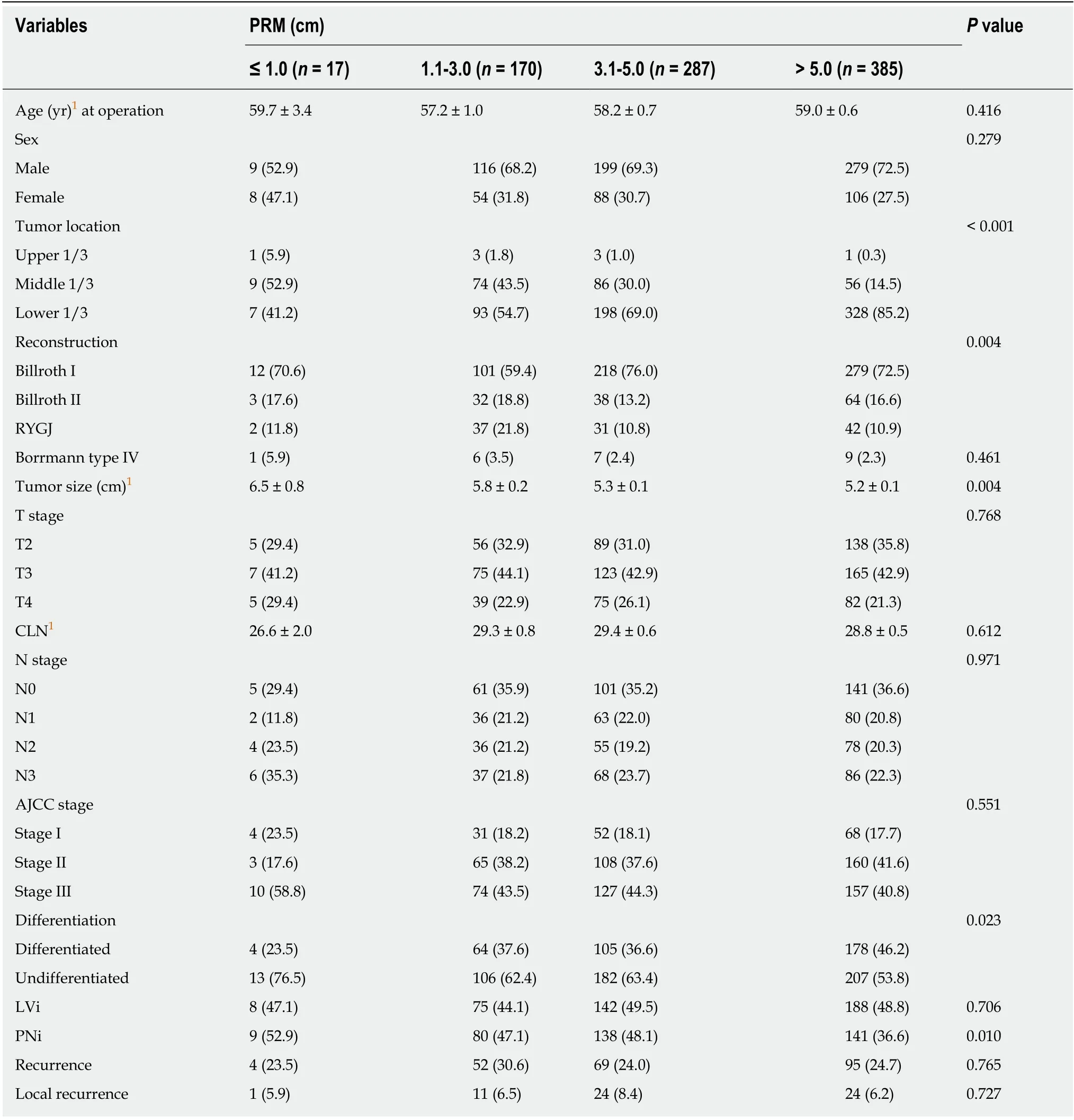
Table 2 Clinicopathologic factors depending on the distance from the proximal resection margin in patients who underwent curative distal gastrectomy, n (%)
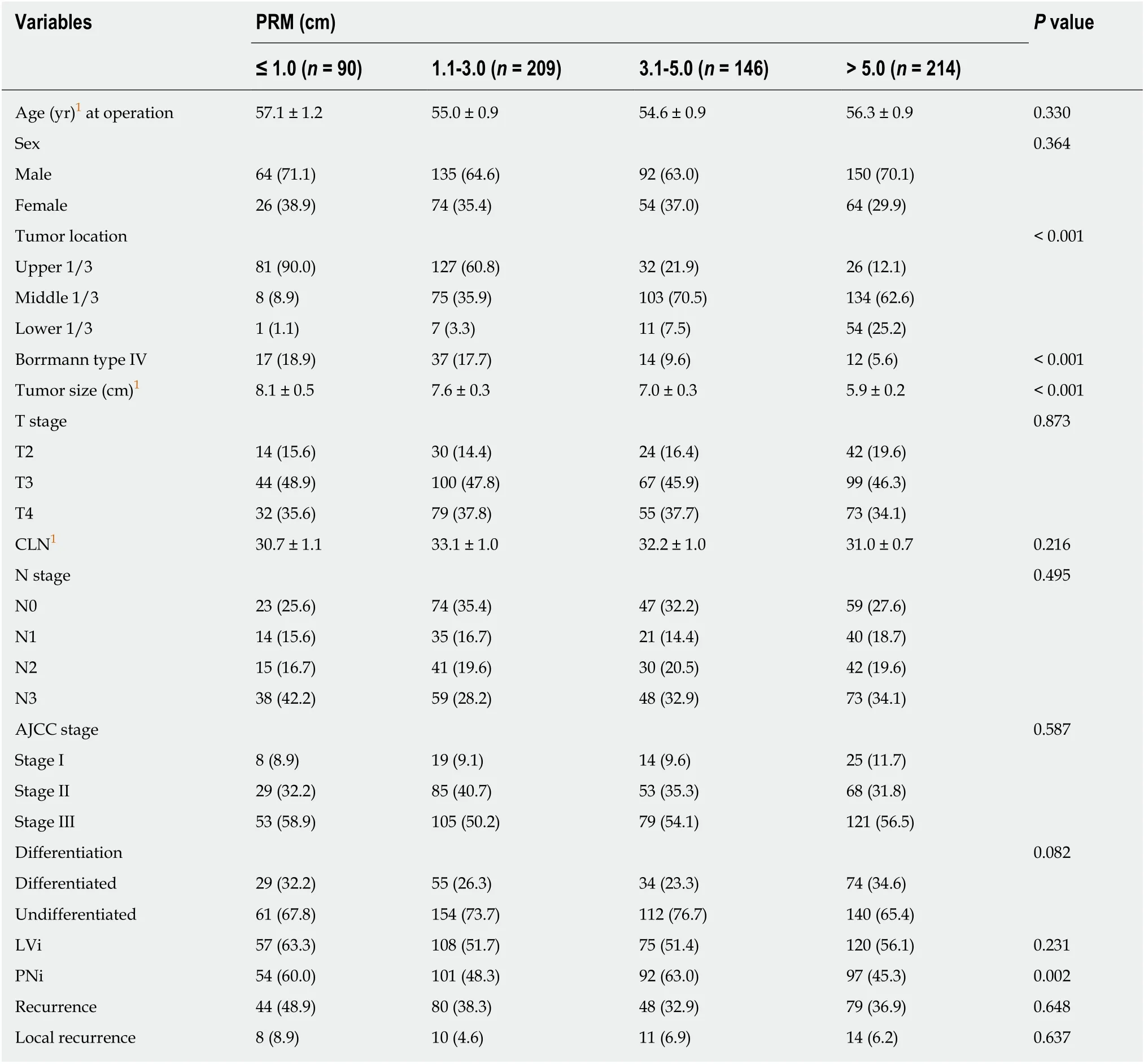
Table 3 Clinicopathologic factors depending on the distance from the proximal resection margin in patients who underwent curative total gastrectomy, n (%)
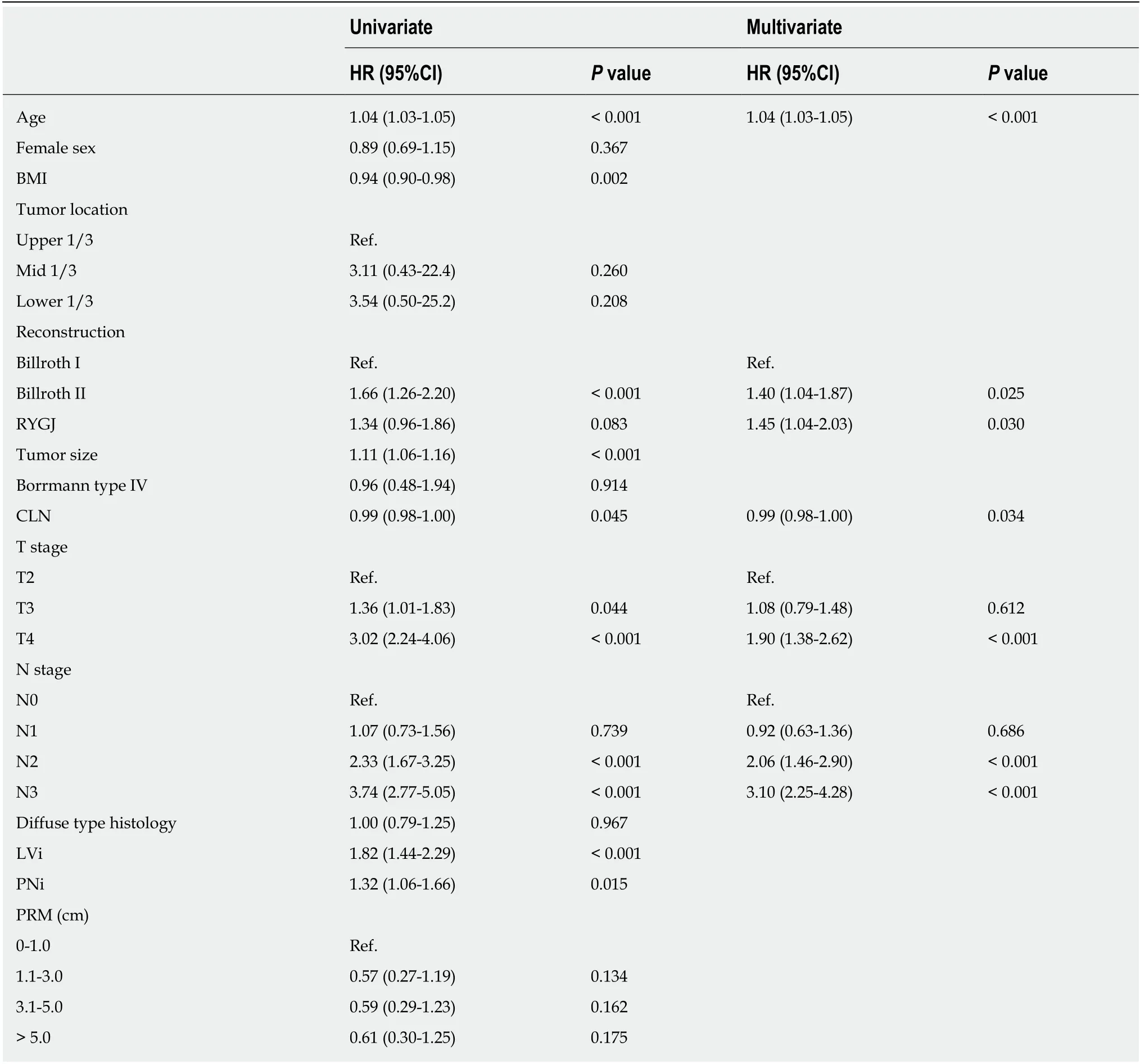
Table 4 Analysis of the risk factors associated with overall survival in patients who underwent distal gastrectomy using the Cox proportional hazard model
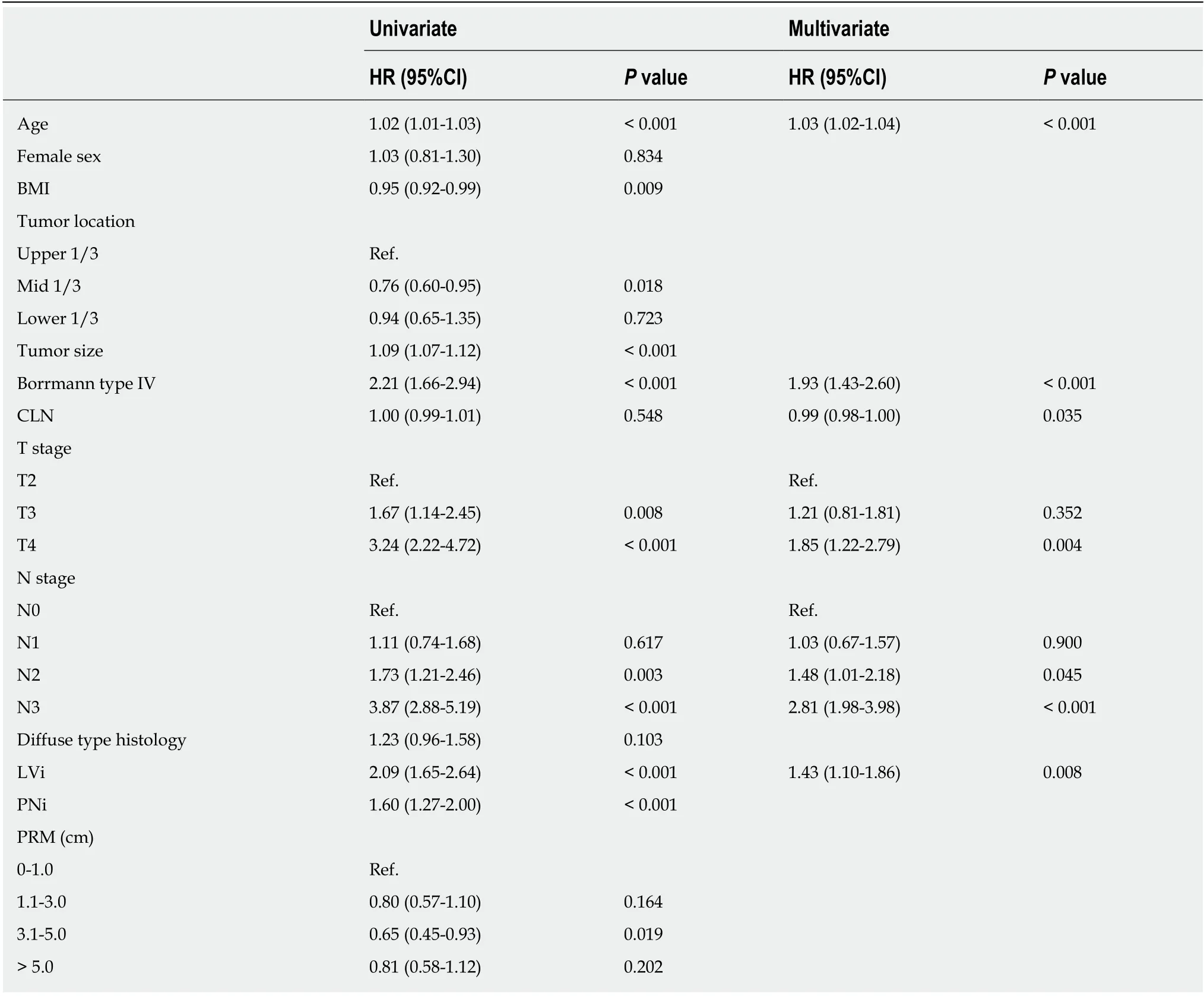
Table 5 Analysis of the risk factors associated with overall survival in patients who underwent total gastrectomy using the Cox proportional hazard model
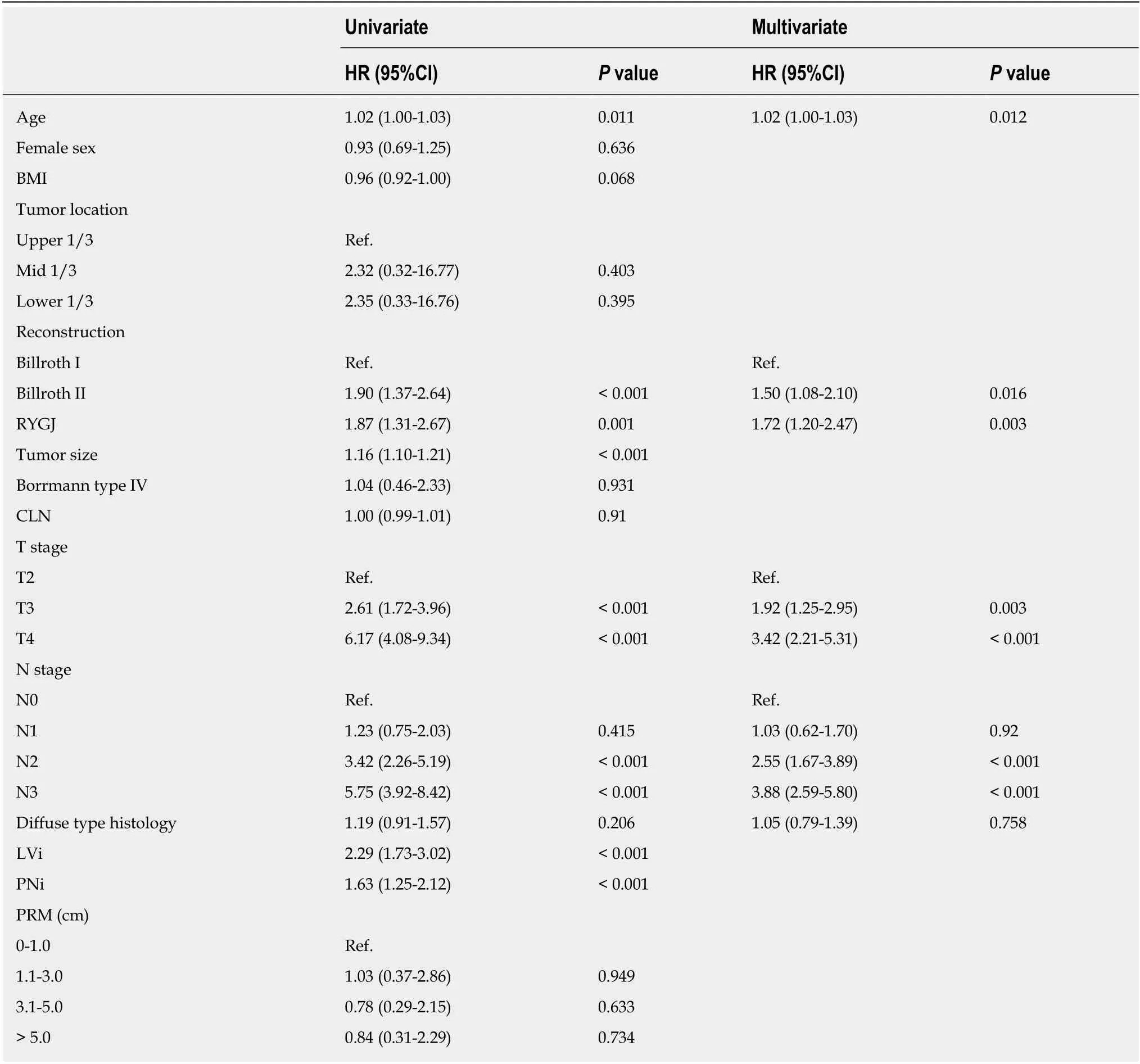
Table 6 Analysis of the risk factors associated with recurrence-free survival in patients who underwent distal gastrectomy using the Cox proportional hazard model

Table 7 Analysis of the risk factors associated with recurrence-free survival in patients who underwent total gastrectomy using the Cox proportional hazard model
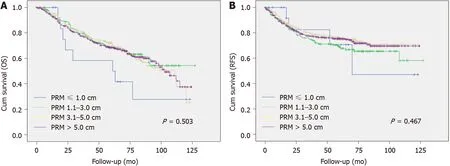
Figure 1 Correlation of overall survival (A) and recurrence-free survival (B) with the distance of proximal resection margin in patients who underwent distal gastrectomy. Kaplan-Meier method was used to analyze OS and RFS according to the distance of PRM. There were no significant differences between the PRM subgroups. OS: Overall survival; RFS: Recurrence-free survival; PRM: Proximal resection margin.
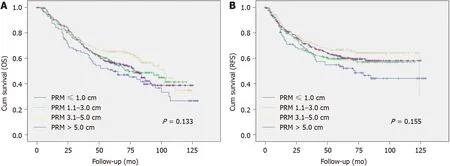
Figure 2 Correlation of overall survival (A) and recurrence-free survival (B) with the distance of proximal resection margin in patients who underwent total gastrectomy. The Kaplan-Meier method was used to analyze OS and RFS according to the distance of PRM. There were no significant differences between the PRM subgroups. OS: Overall survival; RFS: Recurrence-free survival; PRM: Proximal resection margin.
ARTICLE HIGHLIGHTS
Research background
The conventional guidelines suggest the surgeons to obtain an extensive resection margin during surgery for gastric cancer. Several recent studies have raised questions regarding the need for such extensive resection and necessity of total gastrectomy for tumors located on middle-third of stomach, while the consensus has not been reached. There are some studies those demonstrate the unnecessity of longer proximal resection margin (PRM) distance in early gastric cancer.However, there are very few regarding the PRM distance for advanced gastric cancer (AGC).
Research motivation
We would like to discover the optimal PRM distance for patients who undergo gastrectomy for AGC.
Research objectives
The objective of this study was to investigate the influence of the PRM distance on the oncologic outcomes of patients who underwent gastrectomy for AGC, thus to prove the safety of the PRM distance shorter than the conventional literatures suggest.
Research methods
We retrospectively collected data from 1518 patients who underwent total gastrectomy (TG) or distal gastrectomy (DG) for AGC between June 2004 and December 2007. The distances of the PRM and DRM were defined as the shortest distance from the most proximal or distal end to each resection line, measured on formalin-fixed surgical specimens by pathologists. The demographics and clinicopathologic outcomes were compared according to the different PRM categories and an analysis on the influence of PRM on recurrence-free survival and overall survival was performed.
Research results
The DG and TG groups showed no statistical difference in RFS or OS according to the distance of PRM. Multivariate analysis also revealed that in both groups, there was no significant difference in RFS or OS according to the PRM distance.
Research conclusions
The distance of PRM did not affect the incidence of recurrence or local recurrence. A greater PRM distance was not associated with better survival outcomes and a distance as short as < 1 cm did not correlate with worse OS or RFS. Therefore, the PRM distance shorter than conventional literatures suggest may be accepted.
Research perspectives
Further research would be essential to set a guideline for the optimal PRM distance for AGC. A long-term prospective study with detailed data on PRM including measurements done during operation by the surgeons and after fixation by the pathologists should give better answers.
 World Journal of Gastroenterology2020年18期
World Journal of Gastroenterology2020年18期
- World Journal of Gastroenterology的其它文章
- Medical management of metabolic and cardiovascular complications after liver transplantation
- New role for ceramide in hypoxia and insulin resistance
- Role of gut microbiota on intestinal barrier function in acute pancreatitis
- Prognostic significance of hepatic encephalopathy in patients with cirrhosis treated with current standards of care
- Computed tomography vs liver stiffness measurement and magnetic resonance imaging in evaluating esophageal varices in cirrhotic patients: A systematic review and meta-analysis
- Annexin A2 promotion of hepatocellular carcinoma tumorigenesis via the immune microenvironment
