Hydatidiform mole in a scar on the uterus: A case report
Hao-Ru Jiang, Wen-Wei Shi, Xiao Liang, College of Medical Imaging, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
Hui Zhang, Yan Tan, Department of Radiology, First Clinical Medical College, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
Abstract
BACKGROUND
Cesarean scar molar pregnancy is extremely rare, but the incidence has been rising due to the continuous increase in the rate of cesarean section. The presence of a hydatidiform mole in the scar left on the uterus by the procedure may lead to severe complications. We performed a literature review and found only seven reported cases of cesarean scar molar pregnancy. Accurate diagnosis and appropriate treatment are extremely important for the patients’ prognosis.
CASE SUMMARY
A 35-year-old woman, gravida 4, para 1, complained of vaginal bleeding lasting more than 1 mo and amenorrhea lasting more than 2 mo. The patient’s serum human chorionic gonadotropin was 4287800 IU/L. Ultrasound showed a 11.5 cm× 7.5 cm mass at the anterior lower wall of the uterus. The patient underwent suction evacuation, and partial grape-like tissue mixed with blood clots was removed. Uterine arterial embolization was performed to control intraoperative and postoperative bleeding. Histological examination confirmed the presence of a hydatidiform mole in uterine scar. After surgery, there was still a mass with heterogeneous intensity near the isthmus of the uterus on magnetic resonance imaging. The patient then underwent chemotherapy. During the 6-mo follow-up period, the mass disappeared and the serum human chorionic gonadotropin level gradually decreased to normal level.
CONCLUSION
We report a case of cesarean scar molar pregnancy successfully cured by comprehensive treatment. We found that cesarean scar molar pregnancy was subject to intraoperative bleeding, and uterine arterial embolization before surgery may be helpful.
Key words: Hydatidiform mole; Cesarean scar pregnancy; Comprehensive treatment; Case report; Magnetic resonance imaging; Literature review
INTRODUCTION
Cesarean scar pregnancy is a rare type of ectopic pregnancy, which means that the gestational sac is implanted in the myometrium at the site of a previous cesarean section[1]. Hydatidiform mole pregnancy embedded in cesarean scars is also extremely rare[2-5]. It can lead to severe complications, such as uterine rupture, hemorrhage, and maternal death[6]. Here, we report a case of cesarean scar molar pregnancy cured by comprehensive treatment and summarize its clinicopathologic and imaging characteristics based on the previous literature.
CASE PRESENTATION
Chief complaints
A 35-year-old woman complained of vaginal bleeding lasting more than 1 mo and amenorrhea lasting more than 2 mo.
History of present illness
The patient usually had a regular menstrual period lasting 7 d on a 26-d cycle with no dysmenorrhea. There was no obvious cause of continuous vaginal bleeding at any point in the 2 mo leading up to treatment. There were no early pregnancy reactions such as nausea or vomiting and no discomfort such as lower abdominal pain,dizziness, or fatigue. The patient had normal appetite, sleep, and urination despite the bleeding, and she had no weight loss.
History of past illness
The patient had undergone three previous surgical terminations of pregnancy, 10, 6,and 2 years prior, respectively, and one cesarean delivery 10 years prior (gravida 4,para 1).
Physical examination
Physical examination showed a markedly enlarged uterus.
Laboratory examinations
Upon admission, the serum human chorionic gonadotropin (HCG) and β-HCG levels were 4287800 IU/L and 1512540 IU/L, respectively. After suction evacuation under ultrasound guidance and uterine arterial embolization, the HCG and β-HCG levels were 187780 and 66312 IU/L, respectively. Two weeks later, the patient underwent seven cycles of chemotherapy with fluorouracil (5-Fu) and kengshemycin (KSM) once every 3 wk. After the third cycle, the HCG and β-HCG levels were 29540 and 8869 IU/L, respectively. After the sixth cycle, the HCG and β-HCG levels were 381.8 and 115 IU/L, respectively. After the seventh cycle, the β-HCG level was 38.7 IU/L. The HCG/β-HCG level had dropped to normal after 6 wk.
Imaging examinations
At admission, ultrasound indicated a 11.5 cm × 7.5 cm mass at the anterior lower wall of the uterus, in which an anechoic 5.1 cm × 2.8 cm area was noted inside; the echo of the myometrium was heterogeneous. Ten days after embolization, magnetic resonance imaging (MRI) (Figure 1) demonstrated that there was still a mass measuring 6.7 cm × 6.5 cm × 6.0 cm in the proximal isthmus. The lesion showed heterogeneous intensity on both T1-weighted image (WI) and T2WI, heterogeneous hyperintensity on diffusion-weighted image, and hypointensity on apparent diffusion coefficient maps. The mass showed mild rim enhancement in the arterial phase and continued enhancement in the venous and delayed phases; multiple distorted vascular masses were seen in the anterior wall of the uterus. After the sixth cycle of chemotherapy, MRI (Figure 2) showed that the lesion was visibly diminished in size.
FINAL DIAGNOSIS
Histological examination confirmed the diagnosis of hydatidiform mole in a uterine scar (Figure 3).
TREATMENT
The patient underwent a suction evacuation using the No. 8 suction tube (MKL,Suzhou, China) under ultrasound guidance. Abundant grape-like tissue mixed with blood clots was shaved out, but there was a massive hemorrhage during and after the operation. Therefore, the patient was infused with concentrated erythrocyte 4 U and fresh frozen plasma 400 mL, and a Foley catheter balloon was used to restrain blood loss for more than 10 min. Also, emergency uterine arterial embolization was performed to control active bleeding. The Seldinger technique was applied to puncture and catheterize the bilateral internal iliac arteries through the right femoral artery, and the procedure was performed under local anaesthesia. Angiography confirmed that the vessels were uncomplete, tortuous, and disordered. Thus,superselective embolization of both uterine arteries was performed using gelatin sponge granules. Postembolization angiography showed no obvious bleeding. The hemoglobin level was 22 g/L and 48 g/L before and after the embolization,respectively. Then, the patient underwent seven cycles of chemotherapy with 5-Fu and KSM.
OUTCOME AND FOLLOW-UP
During the 6-mo follow-up period, the mass disappeared and the serum HCG gradually decreased to normal level, and the patient had no complaint.
DISCUSSION
Cesarean scar molar pregnancy is extremely rare, but the incidence has been rising due to the continuous increase in the rate of cesarean section[2]. The myometrium of the uterus usually thins and merges with the thin and fibrous scar after caesarean section, so hydatidiform moles in the uterine scar may have severe complications,such as uterine rupture, hemorrhage, hysterectomy, and serious maternal morbidity[6].
To our knowledge, only seven cases have been reported, including one case of cesarean scar invasive molar pregnancy[3], four cases of partial molar pregnancy[2,4,5,7],one case of complete molar pregnancy[8], and one case in which the author did not specify the type[9]. Clinicopathological features of the eight cases including our case are listed in Table 1. Among these cases, the median maternal age was 34 years (range from 28 to 44 years) with a median gravidity of 4 (range from 2 to 8) and at least one parity. All patients had at least two prior uterine curettages. The concentration of HCG/β-HCG also increased abnormally. The clinical manifestations were not fully identical, but the most common symptom was vaginal bleeding for more than 1 mo(6/8 cases, 75%). Other presentations include symptoms of pregnancy[2], abdominal pain[3], and amenorrhea[5], and only one patient was asymptomatic on admission[8].
To date, MRI has not been used very often in the diagnosis of hydatidiform mole embedded in the scar on the uterus. Only two cases have been reported: One was an ectopic molar pregnancy, which showed isointensity on T1WI, hyperintensity on T2WI, and distinct contrast enhancement[10], and the other was a cesarean scar molar pregnancy, which showed a low signal on T1WI and heterogeneous high signal on T2WI, and the myometrium of the anterior wall of the uterine isthmus incision was not continuous[5]. All three cases showed different signals on T1WI and T2WI, which could be caused by hemorrhage or cystic components. Ashet al[6]stated that MRI could be used to show the gestational sac embedded in the anterior lower uterine segment, evaluate pelvic anatomy, improve intra-operative orientation, and assess the possibility of myometrial invasion. Whether MRI is available to the application of hydatidiform mole in the scar of uterus remains to be further studied.
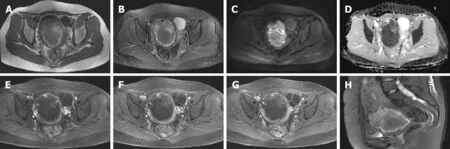
Figure 1 Magnetic resonance imaging demonstrated an irregular mass in the proximal isthmus. A: The lesion was hypointense to hyperintense on T1-weighted image; B: The lesion was hypointense to hyperintense on T2-weighted image; C: Heterogeneous hyperintensity was seen on diffusion-weighted image; D: The lesion was hypointense on apparent diffusion coefficient maps; E: Gadolinium-enhanced magnetic resonance imaging indicated that the edge of the mass was enhanced in the arterial phase; F and G: The edge of the mass was persistently enhanced in the venous and delayed phases; H: Sagittal T2-weighted image showing localized widening of the upper cervical canal.
In histopathology, invasive mole often presents molar villi in the myometrium and vascular permeation, while hydatidiform mole usually presents mildly or markedly hydropic villous swelling with central cistern formation[11]. Missaouiet al[12]found that p57 KIP2 expression was present in partial hydatidiform mole, and the expression of p53 and Ki-67 could reflect the pathological development of hydatidiform mole. This may be helpful to the diagnosis of hydatidiform moles. Among all cases, only one patient underwent immunohistochemical examination with positive p57 expression and proliferation index (Ki-67) of trophocytes of 10%[5].
Gestational trophoblastic disease (GTD) includes the tumour spectrum of hydatidiform mole (complete and partial), invasive mole, choriocarcinoma, and placental-site trophoblastic tumour. Recently, the majority of all the reported cases of cesarean scar GTD are molar pregnancy, and only two cases of cesarean scar choriocarcinoma have been described. Sorbiet al[13]reported a case of cervical choriocarcinoma that had been misdiagnosed as a cesarean scar ectopic pregnancy in 2013. The patient was admitted to hospital for irregular vaginal bleeding of 10 d duration and sovrapubic pain. Qianet al[14]revealed a second case of cesarean scar choriocarcinoma, which was also misdiagnosed as a normal cesarean scar pregnancy in 2014. The patient complained amenorrhea for 47 d and irregular vaginal bleeding for half a month. The rarity and non-specific clinical signs and symptoms of this disease highlight the importance of early consideration of choriocarcinoma when suspecting a GTD in the cesarean scar.
So far, there has been no definitive consensus regarding the treatment of cesarean scar molar pregnancy[2]. Based on our literature review, two cases were treated by suction evacuation, one case was managed with methotrexate, one case was treated with methotrexate and hysterectomy, two cases were cured by suction evacuation and uterine arterial embolization, one case was treated by hysterectomy, and our patient was treated by suction evacuation, uterine arterial embolization, and chemotherapy.In all cases, except for one patient who was lost to follow-up[9], the levels of HCG/β-HCG returned to normal and no corresponding complications occurred. In our case,the HCG decreased visibly after surgery and declined to normal after subsequent chemotherapy. However, intraoperative hemorrhage took place. This involves a high risk of hysterectomy and maternal death, and subsequent uterine arterial embolization was performed.
CONCLUSION
In conclusion, we have documented a case of cesarean scar molar pregnancy successfully cured by comprehensive treatment including suction evacuation, uterine arterial embolization, and chemotherapy. We also performed a literature review and found that MRI was only rarely used in the diagnosis of hydatidiform moles. We also found that most cases of cesarean scar molar pregnancy are associated with intraoperative bleeding, and uterine arterial embolization before surgery might help to prevent massive bleeding.
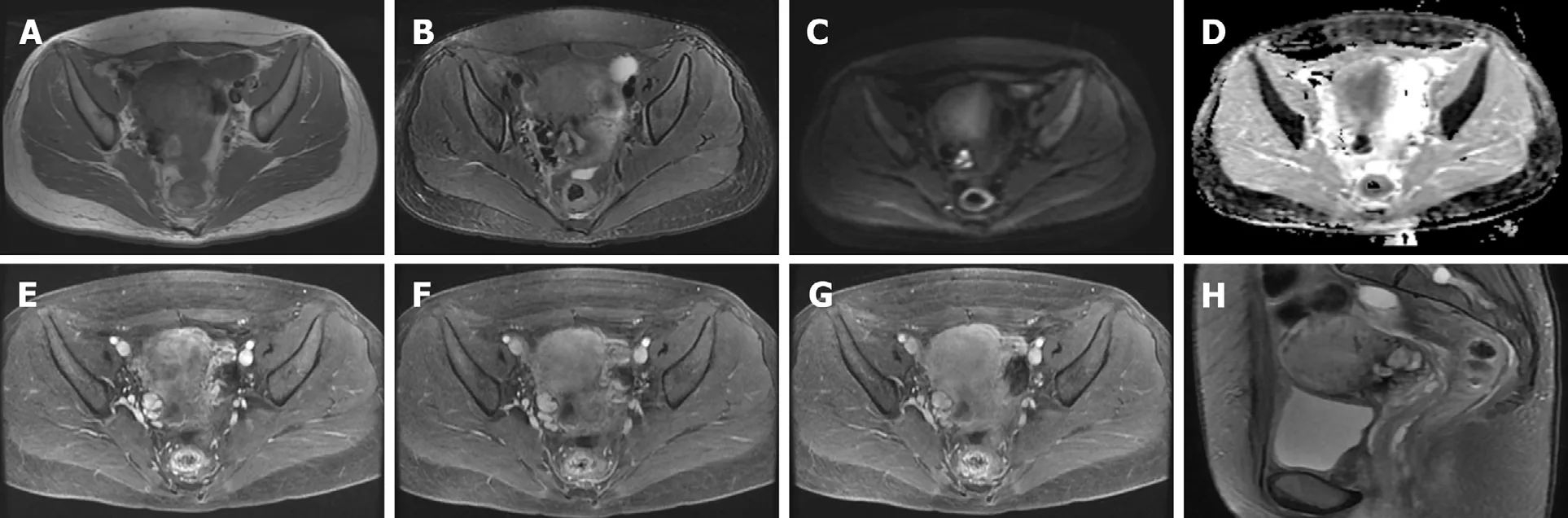
Figure 2 Magnetic resonance imaging of the lesion after treatment. The mass was obviously diminished after treatment (compared with Figure 1). A: The lesion was isointense to hyperintense on T1-weighted image; B: The lesion was isointense on T2-weighted image; C: Heterogeneous hyperintensity was seen on diffusionweighted image; D: The lesion was obviously hypointense on apparent diffusion coefficient maps; E: Gadolinium-enhanced MRI indicated that the lesion was enhanced in the arterial phase; F and G: The edge of the lesion was still persistently enhanced in the venous and delayed phases; H: Sagittal T2-weighted image displaying localized widening of the upper cervical canal.
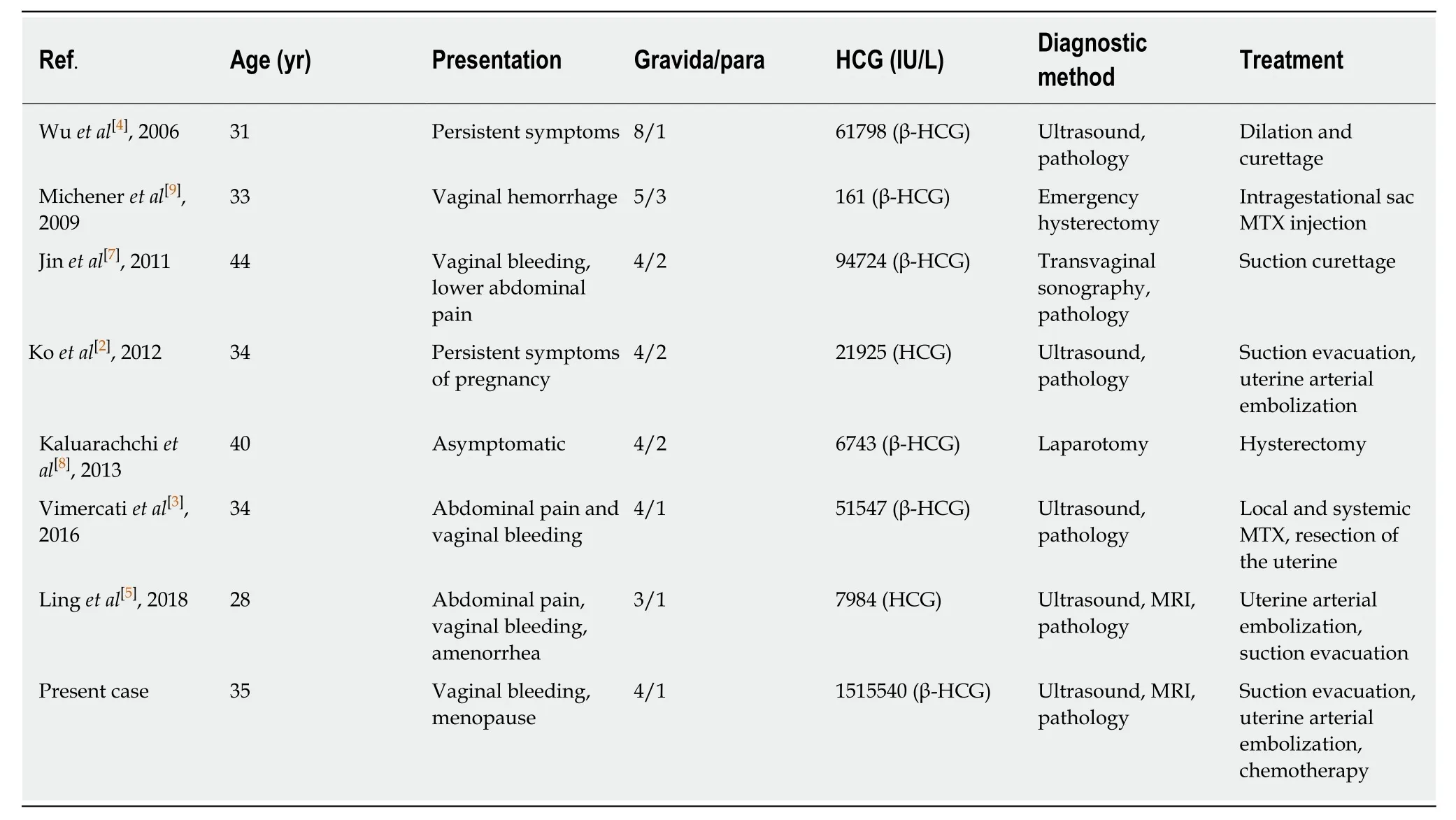
Table 1 Summary of reported cases of molar pregnancy in prior cesarean scar
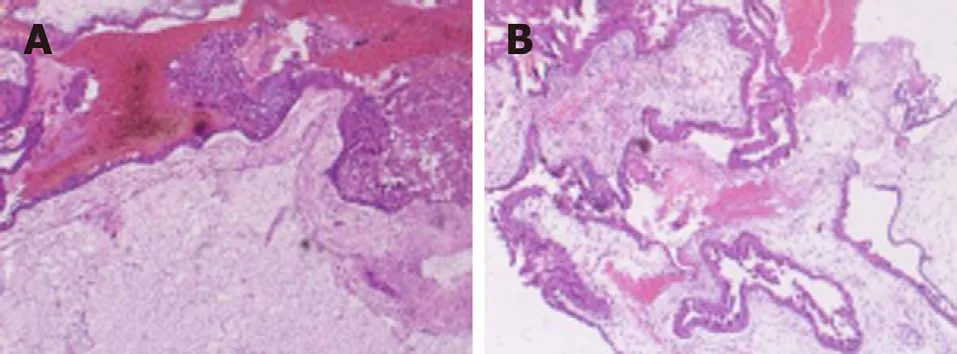
Figure 3 Pathological images. A: Hematoxylin-eosin staining revealed mild or moderate hyperplasia of placental villus trophoblasts (magnification, ×100); B:Hematoxylin-eosin staining showed interstitial edema and central pool formation (magnification, ×100).
ACKNOWLEDGEMENTS
We thank the Gynaecology and Obstetrics Department of the First Hospital of Shanxi Medical University for providing the case information and the assistance of the patient.
 World Journal of Clinical Cases2020年8期
World Journal of Clinical Cases2020年8期
- World Journal of Clinical Cases的其它文章
- Clinicopathological differences and correlations between right and left colon cancer
- Bedside score predicting retained common bile duct stone in acute biliary pancreatitis
- Stability and infectivity of coronaviruses in inanimate environments
- Status, challenges, and future prospects of stem cell therapy in pelvic floor disorders
- Unusual presentation of congenital radioulnar synostosis with osteoporosis, fragility fracture and nonunion: A case report and review of literature
- Predictive factors for central lymph node metastases in papillary thyroid microcarcinoma
