Status, challenges, and future prospects of stem cell therapy in pelvic floor disorders
Juan Cheng, Ya-Li Miao, Department of Obstetrics and Gynecology, Key Laboratory of Birth Defects and Related Diseases of Women and Children of MOE, West China Second University Hospital, West China Campus, Sichuan University, Chengdu 610041, Sichuan Province, China
Juan Cheng, Ling Wang, Jiang Wu, Deep Underground Space Medical Center, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
Zhi-Wei Zhao, Ji-Rui Wen, Jing-Yue Xiao, Fei Fang, West China School of Basic Medical Sciences & Forensic Medicine, Sichuan University, Chengdu 610041, Sichuan Province,China
Li-Wei Huang, West China School of Stomatology Medicine, Sichuan University, Chengdu 610041, Sichuan Province, China
Yan-Lin Yang, Feng-Nian Zhao, West China School of Medicine/West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
Abstract
Pelvic floor disorders (PFDs) represent a group of common and frequentlyoccurring diseases that seriously affect the life quality of women, generally including stress urinary incontinence and pelvic organ prolapse. Surgery has been used as a treatment for PFD, but almost 30% of patients require subsequent surgery due to a high incidence of postoperative complications and high recurrence rates. Therefore, investigations of new therapeutic strategies are urgently needed. Stem cells possess strong multi-differentiation, self-renewal,immunomodulation, and angiogenesis abilities and they are able to differentiate into various cell types of pelvic floor tissues and thus provide a potential therapeutic approach for PFD. Recently, various studies using different autologous stem cells have achieved promising results by improving the pelvic ligament and muscle regeneration and conferring the tissue elasticity and strength to the damaged tissue in PFD, as well as reduced inflammatory reactions, collagen deposition, and foreign body reaction. However, with relatively high rates of complications such as bladder stone formation and wound infections, further studies are necessary to investigate the role of stem cells as maintainers of tissue homeostasis and modulators in early interventions including therapies using new stem cell sources, exosomes, and tissueengineering combined with stem cell-based implants, among others. This review describes the types of stem cells and the possible interaction mechanisms in PFD treatment, with the hope of providing more promising stem cell treatment strategies for PFD in the future.
Key words: Pelvic floor disorders; Pelvic organ prolapse; Stress urinary incontinence;Mesenchymal stem cells; Stem cell therapy
INTRODUCTION
Pelvic floor disorders (PFD) is a term used for a group of clinical conditions, generally including stress urinary incontinence (SUI), pelvic organ prolapse (POP), overactive bladder syndrome, sexual dysfunction, and fecal incontinence, which seriously affect quality of life in women[1]. SUI and POP are highly related to childbirth-associated pelvic floor injury[2]. Studies have estimated that over 50% of parous women have different degrees of SUI and POP, and the incidences increase with age, especially in middle-aged and elderly women. Research has shown that the overall prevalence of POP among middle-aged women is approximately 30% in China and 19% in Australia, while the prevalence of POP among the population of women over age 60 in the United States is higher than 50%. In addition, the risk of SUI is 67% higher with vaginal delivery than caesarian section in the SWEPOP[3]. Wuet al[4]predicted that by 2050 the number of women suffering from symptomatic POP will increase by a minimum of 46% in the United States.
At present, the treatment for these conditions is still conservative and symptombased. Women who have failed or reduced conservative treatment are candidates for surgery, generally including non-absorbable mesh implant repair and autologous tissue or fascia repair. Shahet al[5]also demonstrated that a surprisingly high number of younger women are also undergoing surgical treatment, with 11% of women over the age of 80 years undergoing surgery. Autologous tissue or fascia repair always exhibits a high recurrence rate of approximately 7%, as reported by Quirozet al[6].Recently, the mesh implant for POP repair has been used to reduce the risk of recurrence. The Food and Drug Administration (FDA) cites estimates that one out of three POP surgeries used mesh, and three out of four POP surgeries and more than 80% of SUI surgeries were performedviathe transvaginal mesh (TVM). Vaginal mesh exposure, extrusion, persistent pain, and urethral and/or bladder erosion are the most common complications following TVM-based repair; however, approximately 10% of women undergoing TVM-treated POP experience mesh erosion within 12 mo, with 38.6% of complaints to the FDA pertaining to vaginal pain and/or dyspareunia[7]and 36% to vaginal extrusion[8,9]. Other complications include infection and urinary retention, among others. According to the FDA, more than 1000 adverse events concerning complications after mesh implantation have been reported with the treatment of POP and SUI during the period from 2005 to 2007, while the number of adverse events continued to increase between 2008 and 2010. According to the FDA database, 2874 cases of PFD-related injury, death, and failure were reported, including 1503 cases related to POP and 1371 cases to SUI, which increased five-fold over the 2005-2007 periods. In addition, there were seven cases of death, two cases of intestinal perforation, and one case of bleeding, four of which died due to postoperative medical complications, leading to two warnings issued by the FDA on the repair of POPviaTVM in 2008 and 2011[10]. Thus, POP repair using the transvaginal mesh has not been shown to improve clinical benefit over traditional non-mesh repair, with almost 30% of recipients requiring subsequent surgery[3,11]. Overall, reconstruction of the pelvic floor support structure at the level of molecules and tissue physiological functions, and maintenance of the balance of the micro-environment of the pelvic floor support structure are crucial for the treatment of PFD.
PFD is a disease that includes POP, SUI, and genital fistula, and it is mainly manifested as uterine prolapse, anterior vaginal wall (posterior wall) prolapse,urinary incontinence, urinary retention, urinary fistula, fecal fistula, uterine prolapse,and sexual dysfunction. The changes in the anatomy and position of the pelvic floor organs (uterus, bladder, urethra, rectum, and anus) caused by quantitative and qualitative defects of collagen, elastin, and fibrin proteins of weak pelvic floor tissues(such as ligament and fascia defects, and levator ani muscle, urethral, and anal sphincter function compromise) due to parity, vaginal delivery, menopause, and aging have been identified as important etiologic factors in the development of PFD.Additionally, nerve (sacral plexus and pudendal nerve) defects and declines in various cell types of the pelvic floor tissues, including muscle cells, fibroblasts, and smooth muscle cells (SMCs), among others, also contribute to PFD[12,13]. The pathophysiology of PFD is directly related to the functional anatomy of the pelvic floor. Therefore, any force or process that interrupts the integrity of the connective or neuromuscular tissue supports and weakness in any of constituents without supplement may lead to an increase in PFD. Various studies have focused on the role of connective tissues and neuromuscles in the pathophysiological development of PFD, particularly in SUI and POP, both of which are related to childbirth injuries[14].Fortunately, stem cells are characterized by their self-renewal capacity, multilineage differentiation potential, growth factor secretion, and immunomodulation, among others, and the application of stem cells in the repair of pelvic tissue defects has attracted more interest in recent years. Under specific induction, stem cells differentiate into various cell types of the pelvic floor tissues, including muscle cells and fibroblasts, as compensation for the defective tissue cells to facilitate tissue repair.In addition, stem cells also possess the anti-apoptotic, anti-inflammatory, and provascular formation abilities. In recent years, various therapeutic approaches to PFD using stem cells have been investigatedin vivo. In this review, we provide an overview of the types of stem cells and the possible interaction mechanisms in PFD treatment with the hope of promoting the repair and regeneration of pelvic floor damaged tissues and providing new ideas for the treatment of PFD.
STEM CELL TYPES IN PFD TREATMENT
Mesenchymal stem cells
Mesenchymal stem cells (MSCs) are important members of the stem cell family derived from the early mesoderm. According to the International Society for Cellular Therapy, minimal requirements for MSC characterization in humans are adherence to plastic, multi-lineage differentiation potential (adipocytes, osteoblasts, and chondroblasts), and expression of a series of surface markers including CD29,CD44,CD73, CD105, and CD105 but not the hematopoietic cell markers CD45, CD34, CD14 or CD11b,CD79a, or CD19 and HLA-DR[15], generally including bone marrow-derived mesenchymal cells (BMSCs), human umbilical cord mesenchymal stem cells(HUMSCs), adipose-derived mesenchymal stem cells (ADMSCs), endometrial mesenchymal stem cells (EMSCs), and the emerging organ-resident perivascular MSCs (MSC-like cells). In the presence of proper growth factors and chemical stimulants, MSCs, with self-renewal capacity and multilineage differentiation potential, can differentiate along distinct mesodermal lineagesin vitroandin vivo,including hepatocytes, myocytes, adipocytes, osteoblasts, and chondroblasts, among others[15]. They also have multi-directional differentiation potential after continuous subculture and cryopreservation, and thus, can be used as ideal transplant cells to achieve tissue and organ repair. Table 1 shows the types of stem cells used for pelvic floor disorder treatment.
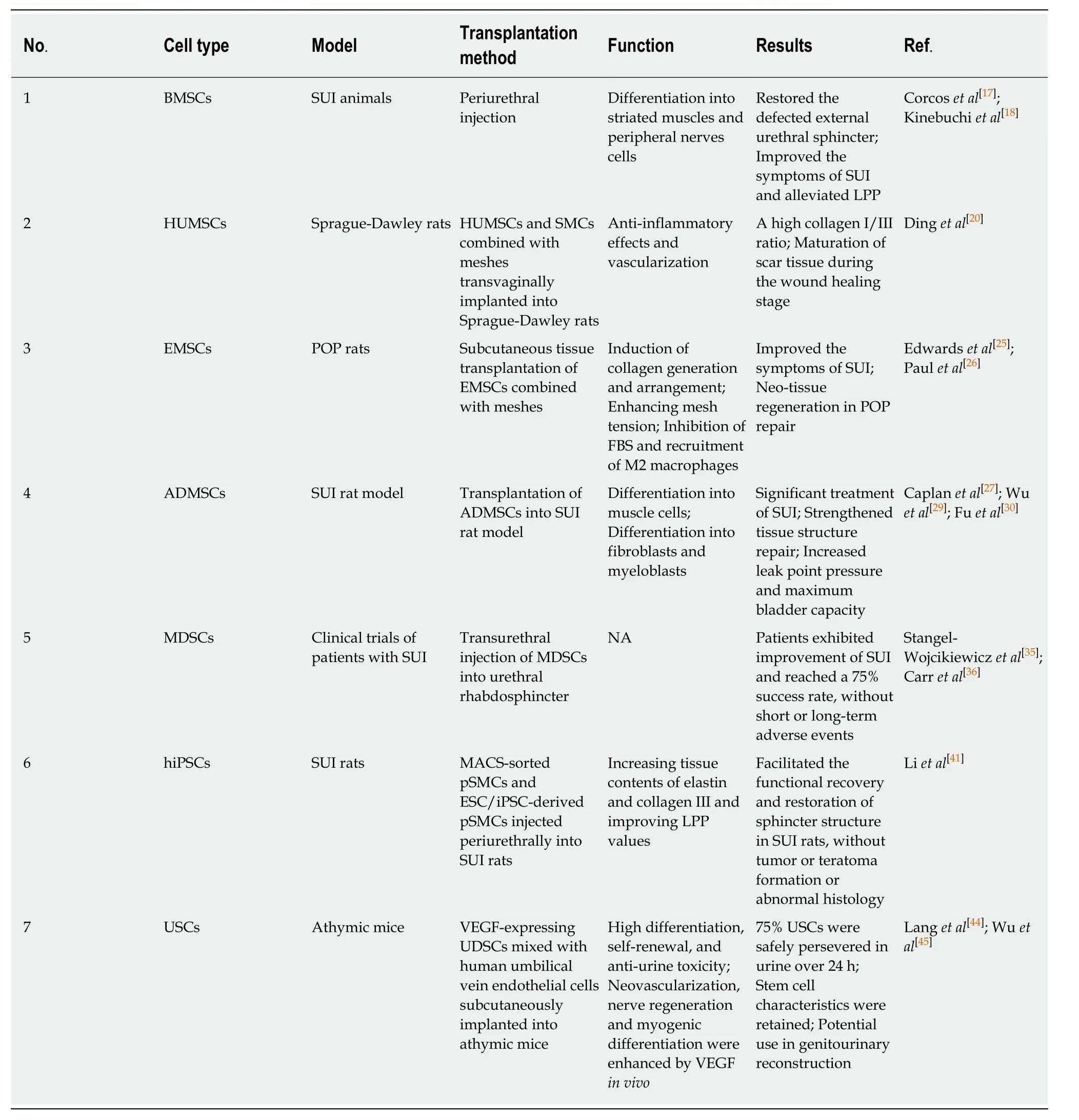
Table 1 The types of stem cells used for pelvic floor disorders treatment
BMSCs:BMSCs are one of the most well-characterized members of the stem cell family, with great differentiation potential and growth factor secretion that benefit tissue repair[16]. Corcoset al[17]reported that, in SUI animal models, periurethral injection of BMSCs for 4 wk could restore the defective external urethral sphincter and significantly improve the symptoms of SUI. Similar results have been reported by Jinet al[14], who demonstrated that microRNA-29 benefited the transplantation of BMSCs to alleviate pelvic floor disorders by repressing elastin. Studies have shown that injection of autologous BMSCs into periurethral tissues in the persistent urethral sphincter insufficiency rat model significantly increased the numbers of striated muscles and peripheral nerves differentiated from BMSCs, meanwhile alleviating the leak point pressure (LPP). However, the bladder capacities did not change significantly[18]. Gunettiet al[19]obtained human MSCs from whole bone marrow, and subsequent transplantation around the external urethral sphincter ultimately resulted in MSC survival for a long time and migration into muscle among fibers and toward neuromuscular endplates in the absence of immunosuppression, without teratoma formation for 4 mo after transplantation. Since the transplantation of BMSCs is safe and convenient without serious side effects in the pelvic muscles, investigation of the role of BMSCs in PFD therapy is of great importance.
HUMSCs:Researchers have considered that HUMSCs have superior potential over other stem cell sources, contributing to their ability to decrease the risk of viral infection and chromosomal abnormalities[20]. Dinget al[20]applied HUMSCs and SMCs differentiated from HUMSCs to produce tissue-engineered fascia equivalentsin vitro,and transvaginally implanted the meshes into Sprague-Dawley rats. The results showed that the PP mesh with both cells showed a trend toward better antiinflammatory vascularization and a high collagen I/III ratio compared with the PP mesh with single stem cells, indicating the maturation of scar tissue during the wound healing stage[21]. In recent years, BMSCs have shown impressive efficacy in stem-cell therapy, such as the alleviation of LPP and improvement of neovascularization, nerve regeneration, and myogenic differentiation in injured rats[22]. However, HUMSCs might have a potential role in fascia tissue engineering to repair POP in pelvic floor reconstruction in the future with advantages of easy harvesting, culture, and expansionin vitro.
EMSCs:EMSCs as a unique source of human mesenchymal stem cells in the endometrium following menstruation, exhibited high self-renewal and proliferative ability and differentiation potential, as well as low immunogenicity and tumorigenicity. Ulrichet al[23,24]have reported that EMSCs differentiated into multiple mesodermal lineages and induced tissue regeneration through paracrine actions.Edwardset al[25]reported that EMSCs combined with gel-coated nylon mesh applied to the subcutaneous tissue of POP rats induced collagen generation and arrangement,as well as enhanced mesh tension by stimulating EMSCs to produce more oriented fascicles with crimped configuration physiological tissue after implantation for 90 d.These findings indicate that neo-tissue regeneration in POP repair may be strengthened by seeding scaffolds with EMSCs and overcome the foreign body response (FBS) of mesh used alone. Paulet al[26]reported that bioprinting of EMSCs onto 3D melt electrospun mesh and AV-ALG hydrogel could potentially inhibit FBS and recruit a large number of anti-inflammatory M2 macrophages, indicating that EMSCs combined with mesh addition could provide a new approach for tissue engineering and regenerative medicine. However, few reports have examined the repair of damaged pelvic floor tissues with EMSCsin vivo, necessitating further research.
ADMSCs:ADMSCs are positive for the cell surface markers CD44 and CD90, which is consistent with the MSC phenotype[27], revealing a potential new research strategy for cell-based therapy. Proañoet al[28]illustrated that ADMSCs, similar to MSCs, are capable of differentiating into osteoblasts, cartilage cells, SMCs, and hematopoietic cells through direct induction. Caplanet al[27]confirmed the characteristics of ADMSCs and the potential for differentiation into muscle cells by flow cytometry analysis.Transplantation of ADMSCs isolated from peri-ovary fat rats into the SUI rat model showed a significant treatment effect. These results are similar with some research.Additionally, Wuet al[29]reported that microRNA-214 combined with rADMSCs injected into SUI rats could clearly strengthen rADMSCs transplantation and tissue structure repair by increasing the leak point pressure and maximum bladder capacity.Moreover, this study also illustrated that microRNA-214 promoted rADMSCs differentiation into fibroblasts by up-regulating the expression of type I collagen, type III collagen, type X collagen, elastin, LOX, and fibulin-5. Fuet al[30]induced the differentiation of autologous rat ADMSCs into myeloblastsin vitroand then delivered them into the bladder neck of SUI rats, which significantly increased the leak point pressure and bladder capacity after transplantation. Kuismanenet al[31]first demonstrated that transurethral injection of endogenic ADMSCs combined with collagen into five patients could be used to treat SUI, and the 1-year follow-up findings suggested that the treatment was safe, well-tolerated, and effective based on a negative cough test and improvement of the 24-h pad test in two of five patients as shown in Table 2. ADMSCs are conveniently obtained and cultivatedin vitro, which supports their good application prospects[30,32].
Muscle-derived stem cells:Muscle-derived stem cells are regarded as candidates for SUI therapy due to their properties of easy collection from striated muscle biopsies,capabilities of long-term self-renewal, proliferation, and multipotent differentiation(including differentiation into endothelial, neuronal, and myogenic lineages), and expression of the surface markers desmin, MyoD, and Sca1 and a series of mesenchymal surface markers[33-35]. Stangelet al[35]evaluated the morphology,confirmed the cellular fusogenic potential, and assessed the cell surface maker expression of desmin to characterize MDCs. After their transurethral injection into the urethral rhabdosphincter of women with SUI, symptoms obviously improved, with a 75% success rate without bleeding or infection at the injection site and no instances of voiding dysfunction, urinary retention, or urinary tract infection reported during the 2-year follow-up. Carret al[36]described the 1-year follow-up results of SUI patients who used autologous muscle-derived cells that were isolated and expanded to the desirable cell dose, viability, and functional integrity. Five of eight patients exhibited a 62.5% improvement based on the diary and pad weight tests, one case showed total
continence, and cure or improvement continued for a median period of 10 mo,without serious adverse events[36]. Stem cell use for pelvic floor disorder treatment in clinical trials is shown in Table 2[31,35-39], and various studies have shown that musclederived stem cell-based therapy may lead to significant and durable improvement of SUI. The clinical trial data suggest that stem cell therapy is effective and safe with minor complications such as pain, local reactions, mild self-limited urinary retention,and urinary tract infections, which are commonly observed with conventional therapies. Overall, data from stem cell studies are promising in terms of short-term clinical outcomes. However, the use of stem cells is in its infancy, and the methodology used to obtain these cells through muscle biopsy is a limiting factor.Therefore, large clinical trials with long-term follow-up are needed to demonstrate the optimal technique, concentration, dosage, and long-term follow-up effect of the implanted stem cells.
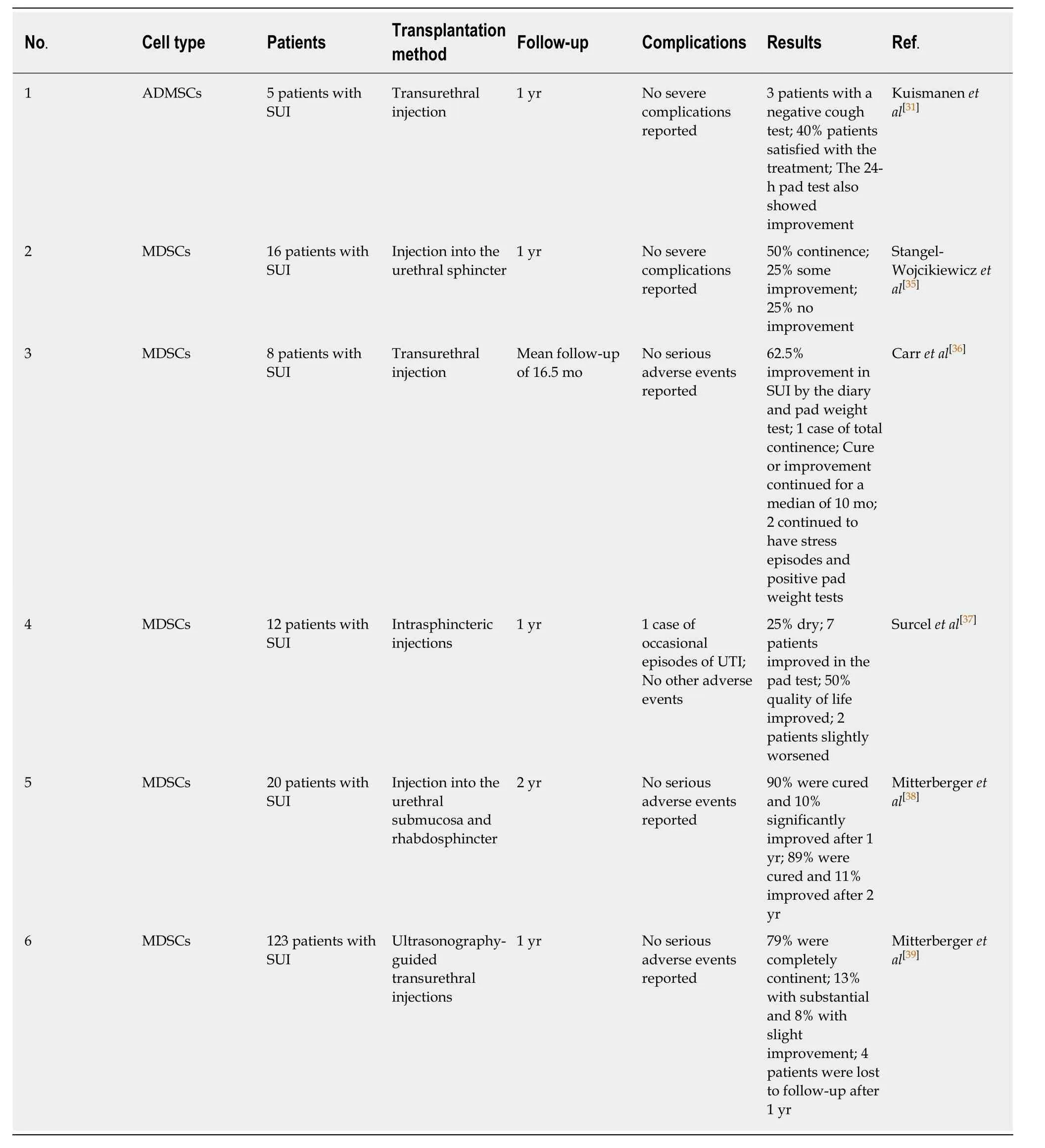
Table 2 Clinical trials of stem cells used for pelvic floor disorders treatment
Human induced pluripotent stem cells:Human induced pluripotent stem cells(hiPSCs) are derived from somatic cells of individual patients, and can be used to provide unlimited autologous tissue and organ-specific cells through targeted differentiationin vitro. Hence, hiPSCs hold great promise for the treatment of many debilitating diseases[40]. Liet al[41]injected immuno-magnetically sorted smooth muscle progenitor cells derived from human-induced pluripotent stem cells (MACS-sorted pSMCs) periurethrally into SUI rats, which efficiently increased elastin genesis in the lower urinary tract and promoted the functional recovery of the damaged urethral sphincter. pSMCs derived from hiPSCs showed promise for the treatment of SUI without tumor or teratoma formation or abnormal histology after transplantation.Another similar study demonstrated that human embryonic stem cells/iPSC-derived pSMCs can facilitate the restoration of the sphincter structure in a SUI rat model when injected periurethrally into female immunodeficient Rowett nude rats with urethral injury or intramuscularly into 8-10-wk-old CB17 severe combined immunodeficiency(SCID) female mice to investigate the effects of pSMCs on injured urethra and longterm survivalin vivo. According to the results, the tissue contents of elastin and collagen III and the LPP value increased significantly after pSMCs transplantation for 5 wk, and long-term survival of these cells was observed in the host urethra for at least 10 wk in SCID mice. Although the innervation and blood supply of the rat bladder and the urethra were likely damaged during cell transplantation after urethrolysis, no other side effects were reported[42]. At present, it is difficult to control the heterogeneity of differentiated hiPSC progeny, which is a persistent obstacle to the clinical transformation of stem cell therapy. Therefore, isolating and purifying the required cells for hiPSC-based cell therapy is necessary.
Urine-derived stem cells:Urine-derived stem cells (USCs) can be obtained from human urine and expandedin vitrowithout enzymatic digestion, which are easily obtained and well tolerated. Urine is a highly cytotoxic agent in urologic regenerative medicine, not only with cytotoxic effects on stem cells but also influencing their differentiation[43]. However, USCs possess strong differentiation, self-renewal, and anti-urine toxicity capacities, and studies have shown that up to 75% of fresh USCs can be safely maintained in urine over 24 h while retaining the initial stem cell characteristics[44]. Wuet al[45]isolated UDSCs from 31 urine samples of six healthy individuals and subcutaneously implanted vascular endothelial growth factor(VEGF)-overexpressing UDSCs mixed with HUVECs into athymic mice. Their results showed that the survival, neovascularization, nerve regeneration, and myogenic differentiation of UDSCs were enhanced by overexpression of VEGFin vivo, implying the USCs may be the most promising source of stem cell-based therapy. However, few studies have examined the treatment of PFD with USCs to date.
APPLICATION OF STEM CELLS FOR TREATMENT OF PFD AND UNDERLYING MECHANISMS
Induction of differentiation
A large number of studies have described the application of stem cells for the treatment of PFD and the possible mechanism underlying the differentiation of stem cells into tissue cells, which may be represented by the specific functions of the cellcell and cell-matrix interactions and the induction of various signaling molecules, as shown in Figure 1. Kinebuchiet al[18]transplanted autologous BMSCs into injured rat urethral sphincter, which significantly alleviated the LPP in injured rats, an effect that was attributed to BMSC survival and differentiation into striated muscle cells, skeletal muscle cells, and peripheral nerve cells. However, current studies have reported a high rate of complications, such as bladder stone formation and wound infection induced by chronic inflammation. Chenet al[46]illustrated that endometrial regenerative cells (ERCs) obtained from menstrual blood have the ability to proliferate extensively and clonogenic activity leading to their differentiation into SMCs following induction in a transforming growth factor β1-based medium.However, vaginal contact may increase the risk of ERC contaminations, and the ERCs derived from older adult patients with POP have self-renewal limitations. Therefore,ERCs collected from patients of a younger age for storage may be of high therapeutic value. In addition, FGF-2 facilitates BMSC differentiation into fibroblasts induced by basic fibroblast growth factor (bFGF) and further promotes pelvic tendon and ligament reconstruction[47]. Suet al[48]illustrated that EMSCs seeded on gelatin-coated mesh (PA+G) scaffolds are able to differentiate into SMCs and fibroblast-like cells induced by connective tissue growth factor (CTGF), thus improving neo-tissue regeneration and conferring tissue elasticity and strength to the damaged fascia tissue in POP. The above experiments confirm that stem cells are able to repair damaged pelvic floor tissues through differentiation under specific induction. However, with high complication and FBS rates, further studies are necessary to decrease the chronic inflammation and improve the urethral function recovery, as well as to elucidate the regeneration mechanism.
Synergism with growth factors
Figure 1 shows that cytokines and growth factors, such as transforming growth factorβ1 (TGF-β1), VEGF, and bFGF have the ability to stimulate stem cell growth and direct phenotypic cell differentiation. Therefore, the delivery of growth factors to a transplant site or in combination with stem cells to enhance their differentiation is an effective therapeutic strategy. bFGF, as a member of the fibroblast growth factor family, has the capacity to stimulate BMSC differentiation into fibroblasts and the expression of extracellular matrix proteins[47,49]. Researchers have illustrated that transplanted elastin-expressing BMSCs into vaginal distension-induced damaged tissue in PFD rats stimulates fibroblast differentiation and collagen and elastin secretion, and this beneficial effect can be further enhanced by sustained release of bFGF from poly lactic-co-glycolic acid nanoparticles. However, the short half-life of bFGF and thus maintenance of a stable local concentration requiring repeated injections lead to a high cost of relevant therapies. Nevertheless, tracing of the fate and phenotype of engrafted BMSCs in tissues remains a big challenge[14]. Additionally,TGF-β1, platelet-derived growth factor-β, and CTGF induce the differentiation of EMSCs into SMC-specific protein-expressing SMCs. CTGF induces the differentiation of EMSCs into tenascin-C and collagen type I-producing fibroblast-like cells,improving neo-tissue reconstruction of the damaged fascia tissue in POP[48]. Wuet al[45]illustrated that the survival, neovascularization, nerve regeneration, and myogenic differentiation of UDSCs were enhanced by overexpression of VEGF following the injection of autologous VEGF-expressing USCs combined with HUVECs into adult female athymic mice. The VEGF-overexpressing USCs possessed enhanced abilities to improve nerve regeneration and neovascularization, among others, compared with non-VEGF-expressing grafts, implying that USC grafts might have an advantage over common bulking agents and hyaluronic acid owing to their longer viabilityin vivo. At present, since VEGF is associated with urothelial cancer, the safety of VEGF-overexpressing cell grafts remains a concern. Therefore, further long-term follow-up studies after implantation of USCs expressing VEGF are required.
Exosome secretion
In contrast to previous stu dies, recent increasing evidence suggests that the tissue repair and immunomodulatory functions of MSCs are largely attributed to intercellular communication mediated by exosomes through the delivery of biomolecules, including mRNA and miRNA, to recipient cells, rather than their capability to differentiate into other cell types, as shown in Figure 1[50]. Liuet al[51]isolated and purified exosomes from human ADMSCs and transferred them to the fibroblast cytoplasm of periurethral vaginal wall tissues of women with SUI, and they observed that exosomes secreted by ADMSCs (ADMSC-Exos) promoted fibroblast proliferation and collagen synthesis by upregulating the levels of TIMP metallopeptidase inhibitor 1 (TIMP-1), TIMP-3, and type I collagen and downregulating the expression levels of matrix metallopeptidase-1 (MMP-1) and MMP-2. Similar results were found with exosomes from ADMSC-conditional medium, in which ADMSC-Exos could be taken up and internalized by fibroblasts to stimulate collagen synthesis and metabolism, cell migration, and proliferation[52].Researchers also illustrated that MSC-like cell exosomes (iMSC-exos) were capable of enhancing neovascularization, proliferation, and maturation of human umbilical vein endothelial cell (HUVEC) vessels, as well as collagen and elastin protein secretion through activated PI3K/AKT signaling[53]. In addition, MSC-derived exosomes possessed anti-inflammatory abilityviainhibition of STAT3 signaling[54]. Above all,previous studies have reported that the decreased collagen and elastin contents and altered morphologic features in the pelvic support tissues of women will eventually lead to SUI, with exosomes playing a crucial role in regulating collagen metabolism in SUI patient[55,56]. Therefore, the provision of a safe and efficient alternative to MSCExos-based therapies for SUI treatment is needed. Present studies focusing on exosome function are in the early stage; thus, determination of the production,administration route, and dosage are crucial. Moreover, the application of large and immune-competent disease animal models in comprehensive studies of the absorption, distribution, metabolism, and excretion of exosomes is urgently needed[50].
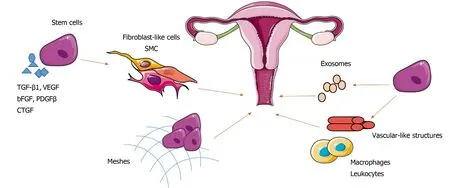
Figure 1 Application of stem cells for the treatment of pelvic floor disorders and the possible underlying mechanisms. Stem cell synergistic cytokines and growth factors or the combination with meshes can promote the differentiation of stem cells into fibroblast-like cells and smooth muscle cells, thus improving neotissue regeneration and repairing the damaged tissue/fascia. Stem cells stimulate collagen synthesis and metabolism, cell migration, proliferation, neovascularization,and anti-inflammatory effects to facilitate repair of the pelvic floor by secreting exosomes or recruiting macrophages and leukocytes. SMC: Smooth muscle cells; TGF-β1: Transforming growth factor-β1; VEGF: Vascular endothelial growth factor; bFGF: Basic fibroblast growth factor; PDGF-β: Platelet-derived growth factor-β; CTGF:Connective tissue growth factor.
Pro-vascular formation and anti-inflammatory effects
Ben Menachem-Zidonet al[57]illustrated that both systemic and local transplantation of MSCs in a vaginal injury rat model improved the capacity for new vascular-like structure formation through differentiation into endothelial cells. Previous studies have shown that MSCs stimulated to undergo endothelial differentiationin vitrowith appropriate stimulating factors including insulin-like growth factor 1 and VEGF[58-61],followed by transplantation of these early-differentiation-stage cells into SCID mice,clearly promoted neo-vascular structure formationin vivo[62]. Nevertheless, it is beneficial to avoid immune response reactions through the use of endothelial cells in the early stage of differentiation. At present, a large number of studies have shown that endothelial cells differentiated from stem cells can develop into capillaries under induction with VEGF and other stimulatory factors. However, the conditions and efficiency of the endothelial cells for identifying the disrupted endothelial network and determining the involvement in angiogenesis have remained obscure to date[63].Researchers have implanted gelatin-coated polyamide knitted mesh seeded with EMSCs in a rat wound model of POP repair surgery, which demonstrated a significant decrease in M2 and M1 macrophages and leukocytes surrounding the mesh filaments at 90 d. These findings indicated that EMSC possess long-term antiinflammatory effects and induce wound repair by promoting neo-tissue formation, as shown in Figure 1. Notably, it also appears that the type of macrophage activity might be influenced by EMSC cytokines in the wound healing response[23]. At present, the exact immunomodulatory mechanism of MSCs and whether EMSC are capable of reducing the inflammatory response and modulating the healing microenvironment through paracrine effects over the long term are still unclear[64,65], and related studies of stem cells in this respect are rare.
Possible mechanisms
Overall, stem cell-based therapy generally requires trans- or periurethral injections of different stem cell preparations (including stem cells alone, stem cells combined with cytokines or seeded on mesh, or the secretion of exosomes) into the bladder neck,external sphincter, or submucosa[66-68]for PFD treatment. To assess the success of treatment, the Incontinence Score (a 24-h voiding diary, 24-h pad test, and patient questionnaire)[69], incontinence quality of life test[70], urodynamic tests (including pressure flow studies, urethral pressure profiles, voiding cystometry, and urethral profilometry)[71], kinesiological electromyography measurements, and the highfrequency transducer imaging technique among others, were used before and after treatment to assess the pattern of individual muscle activity, and any therapeutic effect on urethral closure pressures and the morphology and function of the urethra and rhabdosphincter[72]. MSCs have shown impressive efficacy in most of PFD patients, with alleviation of LPP, improvement of quality of life, the pad test, and negative cough test, an increase in resting tone and voluntary contractile force, and improvement of the rhabdosphincter and urethral submucosa regeneration without serious side effects such as scars, hyperplasia, tumors, or inflammation, as shown in Table 2.
In conclusion, under induction by a series of cytokines and growth factors,including VEGF, platelet-derived growth factor-β, CTGF, TGF-β1, FGF-2, and bFGF,MSCs were originally thought to improve tissue repair by transdifferentiation[27,73,74]into the required cell types, such as striated muscle cells, SMCs, fibroblasts, and peripheral nerve cells, among others. Additionally, improvements have been observed in collagen, elastin, and tenascin-C protein secretion and cell migration,proliferation, and neovascularization[45,47,48], thus improving connective or neuromuscular tissues or any weak constituent regeneration and conferring tissue elasticity and strength in PFD. However, recent increasing evidence suggests that MSCs promote tissue repair largely due to intercellular communication mediated by exosomes through the delivery of copious quantities of bioactive molecules around the site of injury to promote angiogenesis by enhancing the migration and proliferation of tissue-specific progenitor cells such as microvascular endothelial cells through upregulation of the expression of angiogenic factors such as VEGF-A and bFGF. Additionally, exosomes can inhibit apoptosis, fibrosis, and scarring by promoting fibroblast and muscle cell proliferation and collagen and elastin protein synthesis and metabolism through upregulating the expression levels of TIMP-1,TIMP-3, and type I collagen and downregulating those of MMP-1 and MMP-2[27,52,53].Exosomes can also inhibit inflammation by recruiting macrophages and leukocytes.Present studies are focused on exosome function in the early stage, and further research is necessary.
MSCs also inhibit the inflammatory response and modulate both the innate and adaptive immune systems, while the exact immunomodulatory mechanism of MSCs in PFD repair is still unclear. Previous studies have reported that MSCs can drive a phenotypic change from pro-inflammatory M1 macrophages to anti-inflammatory M2 macrophages through the interaction of prostaglandin E2 with macrophage prostanoid receptors[75,76]. It is also well known that BDMSCs can induce immunosuppression by decreasing pro-inflammatory cytokines such as TNF-a, IL-6 IL-1α, and IL-1β and increasing anti-inflammatory cytokines such as IL-10, as well as suppressing T lymphocytes, dendritic cells, and natural killer cells to downregulate innate inflammatory and acquired immune responses[76,77].
CHALLENGES AND FUTURE PROSPECTS
PFD is a widespread disease in both middle-aged and elderly women, and traditional surgical therapeutics are traumatic and costly, with high postoperative complications and recurrence rates, mainly targeting severe patients. The emergence of cell-based therapy with stem cells provides new ideas for the treatment of PFD. However,current research is mainly focused on animal experiments, clinical trials are rare, and the mechanism of stem cell therapy for PFD requires further study. Due to the short observation stage, long-term effects such as tumorigenicity, thrombosis, and foreign body reactions (FBRs) cannot be evaluated; thus, the clinical application of stem cell therapy, alone or in combination with mesh implantation, still requires a large number of long-term studies.
Traditional POP surgery with transvaginal implant synthetic polypropylene meshes often causes serious FBR, and the long-term durability and safety of the synthetic mesh remain unknown due to the mesh exposure and erosion[78,79]. Recently,a large number of studies have focused on improving the tissue properties and biocompatibility of meshes, including the use of adult stem cells. The application of stem cells for tissue engineering has promoted tissue integration and regeneration, as well as reduced inflammatory reactions, collagen deposition, and FBR in the long term over traditional mesh implants, indicating that the combination of stem cells with synthetic biomaterial scaffolds is a valuable treatment and potentially can achieve long-term mechanical integrity for tissue repair in PFD[80]. In addition, cellfree treatments that achieve the same therapeutic effect through the paracrine action of stem cells and that deliver biomolecules including mRNA and miRNA into recipient cells can avoid FBR of stem cellsviatransplantation directly into the damaged tissue. Recently, an increasing number of studies have been dedicated to investigating the effect of exosomes secreted by stem cells on the treatment of POP,which indeed alleviated POP and reduced the incidence of FBR compared with stem cells transplanted directly into the body[50]. At present, studies focusing on the function of exosomes are in the early stage, and thus, comprehensive studies of the absorption, distribution, metabolism, and excretion of exosomes are urgently needed.
Additionally, organ-resident perivascular MSCs (MSC-like cells) are characterized by their self-renewal and multi-lineage differentiation capacity and growth factor secretion, which have been reported and isolated from various tissues and organs including the umbilical cord, skeletal muscle, adipose tissue, lung, heart, and liver,among others. These findings indicate that MSC-like cells may be a potential source of stem cell therapy for PFD. However, the emerging MSC-like cells display commonalities in MSC surface marker expression without a real consensus or a single surface marker leading to the identity of these cells difficultly[81,82]. Therefore, the identification of specific cell surface markers of MSC-like cells requires further study,and it will also be meaningful to isolate, culture, and identify the MSC-like cell population in pelvic floor organs. Moreover, EMSCs, as a unique source of human MSCs within the endometrium following menstruation, can be harvested in relatively large quantities with minimal morbidity compared with bone marrow and exhibit immense potential for PFD treatment due to their accessibility and effectiveness.Various types of MSCs have been used to treat SUI, demonstrating safety and feasibility in humans[35], However, harvesting and expanding these adult stem cellsin vitrois difficult, and the exact mechanism underlying the improved clinical outcome has not been well defined. hiPSCs have great promise for the treatment of many debilitating diseases due to their unlimited differentiationin vitro. However, many challenges persist, and a clinical-scale method for purifying or enriching the required cells from a differentiated hiPSC cell population is urgently needed[30,32]. HUMSCs and USCs represent a promising source of stem cell-based therapy for PFD, while related studies are rare, necessitating further investigation. Studies examining stem cells derived from the dermis for PFD treatment have not been reported to date.
This paper examines the status and highlights the feasibility of stem cell-based therapeutic strategies targeting POP and SUI, proposing challenges and future prospects for stem cell therapies to promote the development of stem cell therapy for PFD treatment.
 World Journal of Clinical Cases2020年8期
World Journal of Clinical Cases2020年8期
- World Journal of Clinical Cases的其它文章
- Clinicopathological differences and correlations between right and left colon cancer
- Bedside score predicting retained common bile duct stone in acute biliary pancreatitis
- Stability and infectivity of coronaviruses in inanimate environments
- Unusual presentation of congenital radioulnar synostosis with osteoporosis, fragility fracture and nonunion: A case report and review of literature
- Predictive factors for central lymph node metastases in papillary thyroid microcarcinoma
- Suicide attempt using potassium tablets for congenital chloride diarrhea: A case report
