可溶性髓系细胞表达触发受体-1评估重症肺炎病情的价值
杨志明 陈鸣娣 刘晓月 邹天士 林颖


[摘要] 目的 分析重症肺炎患者血浆可溶性髓系细胞表达触发受体-1(sTREM-1)水平变化及临床意义。 方法 选取2018年6月~2019年3月在广东医科大学附属第二医院重症监护室治疗的重癥肺炎24例(设为重症肺炎组),其中有15例病情好转(好转组),选取健康体检者19例作为对照组,采用ELISA方法检测重症肺炎组入住ICU第1天、好转组病情稳定转至普通病房当天及对照组体检当天的sTREM-1水平,并记录重症肺炎患者入住ICU第1天及其转出病房当天的急性生理学与慢性健康状况(APACHE Ⅱ)评分。比较各组sTREM-1水平差异,统计分析sTREM-1与APACHE Ⅱ评分的相关性。 结果 血浆sSTREM-1水平在重症肺炎组、好转组和对照组比较,差异无统计学意义(P>0.05)。重症肺炎组APACHE Ⅱ评分较好转组明显升高,差异有统计学意义(P<0.05)。重症肺炎患者第1天血浆sTREM-1水平与APACHⅡ评分无明显相关性(r=-2.53,P=0.223)。 结论 sTREM-1用于重症肺炎的病情评估、预后判断尚需持谨慎态度。
[关键词] 可溶性髓系细胞表达触发受体-1;重症肺炎;APACHE Ⅱ评分
[中图分类号] R563.1 [文献标识码] A [文章编号] 1673-9701(2020)05-0034-04
Value of soluble myeloid cells triggering receptor-1 expression in the assessment of severe pneumonia
YANG Zhiming1 CHEN Mingdi2 LIU Xiaoyue3 ZOU Tianshi1 LIN Ying1
1.Department of Respiratory Medicine, the First People's Hospital of Zhaoqing City in Guangdong Province, Zhaoqing 526000, China; 2.Intensive Care Unit, the Second Affiliated Hospital of Guangdong Medical University, Zhanjiang 524003, China; 3.Science Education Museum (Guangdi Geological Sanatorium), Guangdong Provincial Geological Bureau, Zhaoqing 526000, China
[Abstract] Objective To analyze the changes of plasma soluble myeloid cells triggering receptor-1 (sTREM-1) levels and their clinical significance in patients with severe pneumonia. Methods 24 patients with severe pneumonia from June 2018 to March 2019 in the ICU of the Second Affiliated Hospital of Guangdong Medical University were selected and set as severe pneumonia group, of whom 15 cases were improved(improved group). 19 healthy physical examination cases were selected as the control group. STREM-1 levels of the severe pneumonia on the first day of ICU, on the day of stable transfer to the general ward of the improved group and on the day of the physical examination of the control group were detected by ELISA method. The acute physiology and chronic health status (APACHE Ⅱ) scores of patients with severe pneumonia on the first day of admission to the ICU and the day they were transferred out of the ward were recorded. The differences of sTREM-1 level in each group were compared, and the correlation between sTREM-1 and APACHE Ⅱ score was statistically analyzed. Results There was no statistically significant difference of plasma sTREM-1 level among the severe pneumonia group, the improved group and the control group(P>0.05). The APACHE Ⅱ score in the severe pneumonia group was obviously higher than that in the improved group, with statistically significant difference(P<0.05). There was no significant correlation between plasma sTREM-1 level and APACHⅡ score on the first day in patients with severe pneumonia(r=-2.53, P=0.223). Conclusion sTREM-1 should be used with caution in assessing the condition and prognosis of severe pneumonia.
[Key words] Soluble myeloid cells express trigger receptor-1; Severe pneumonia; APACHEⅡ score
重症肺炎是一种进展性肺部炎症,短时间内进展迅速,且可引起肾脏、神经系统等并发症,病死率高,严重危及患者的生命安全[1]。早诊断和早治疗十分重要,可降低死亡率,所以寻找特异性和敏感性高的生化指标,对病情的评估及预后判断有着重要意义。目前临床上常用白细胞和C-反应蛋白等指标对疾病严重程度及其预后进行评估,但敏感性和特异性较差。髓系细胞触发受体-1(TREM-1)是新近发现的一种炎症激发受体,当机体受炎症感染时在中性粒细胞及单核细胞表面呈高表达状态,能促进炎性因子分泌、诱导促炎介质以及抑制抗炎因子产生,其介导的信号转导在炎症反应的发生和级联放大中起重要作用[2],能够在感染期间进入血液,与机体感染程度及预后有一定相关性[3]。本文观察sTREM-1及APACHE Ⅱ评分在重症肺炎中的变化及其之间的关系,探讨其临床价值,以指导临床诊疗,现报道如下。
1 资料与方法
1.1 一般资料
选取2018年6月~2019年3月在广东医科大学附属第二医院重症监护室治疗的重症肺炎24例作为重症肺炎组,其中15例作为病情好转(好转组)。其中男11例,女13例,平均年齡(69.3±4.7)岁。另选19例健康体检者作为对照组,男11例,女8例,平均年龄(62.2±8.2)岁。各组受试者在性别、年龄方面的比较差异无统计学意义(P>0.05),具有可比性。所有患者符合重症CAP的诊断标准[4]:符合下列1项主要标准或≥3项次要标准者可诊断为重症肺炎,需密切观察,积极救治,有条件时收住ICU治疗(ⅡA)。主要标准:(1)需要气管插管行机械通气治疗;(2)脓毒症休克经积极液体复苏后仍需要血管活性药物治疗。次要标准:(1)呼吸频率≥30次/min;(2)氧合指数≤250 mmHg(1 mmHg=0.133 kPa);(3)多肺叶浸润;(4)意识障碍和(或)定向障碍;(5)血尿素氮≥7.14 mmol/L;(6)收缩压<90 mmHg需要积极的液体复苏。对照组均排除呼吸系统疾病、心脑血管疾病及急慢性感染者。本研究通过医院伦理委员会批准,所有研究对象知情同意。好转组入选标准:重症肺炎患者病情好转,氧合改善,可以撤有创呼吸机辅助通气,休克纠正且停用血管活性药物,酸碱平衡纠正等,好转组患者已不再符合重症肺炎诊断标准是最基本的入选标准。
1.2 方法
1.2.1 血浆sTREM-1水平测定 重症肺炎组于入院第1天,好转组于病情稳定转出普通病区当天检测血浆中sTREM-1的表达。对照组于体检当天抽静脉血5 mL。4℃,3500 r/min离心15 min,取上清液,将其置于-20℃冰箱冻存被检。使用ELISA法测定血浆人可溶性髓系细胞触发受体-1(sTREM-1),ELISA试剂盒购于上海劲马实验设备有限公司。
1.2.2 急性生理学与慢性健康(APACHE Ⅱ)评分[5] 急性生理学与慢性健康(APACHE Ⅱ)评分,即由急性生理评分、年龄评分及慢性健康评分组成。其中急性生理评分包括体温、平均动脉压、心率、呼吸频率、氧分压、血气pH值或碳酸氢根浓度、血钾、血钠、血肌酐、白细胞比容、白细胞计数、格拉斯哥昏迷评分(GCS)在内的12项生理指标;慢性健康评分要求患者符合慢性器官功能不全或免疫功能抑制,内容包括肝脏功能、心血管、呼吸系统、肾脏功能及免疫功能抑制情况。最终APACHE Ⅱ评分等于急性生理评分、年龄评分与慢性健康评分之和。重症肺炎患者在入院第1天和好转组于病情稳定转普通病区当天作急性生理学与慢性健康(APACHEⅡ)评分[5]。
1.3统计学分析
采用SPSS17.0统计学软件处理数据。符合正态分布的计量资料以均数±标准差(x±s)表示,不符合正态分布的计量资料采用中位数(四分位间距)M(P25,P75)表示;对于符合正态分布的计量资料组间比较采用t检验;不符合正态分布的采用非参数秩和检验,两个独立样本用Mann-Whitney检验,两个相关样本采用Wilcoxon检验;两变量符合双变量联合正态分布,采用Pearson相关分析,不满足Pearson相关分析条件的采用Spearman相关分析,P<0.05为差异有统计学意义。
2 结果
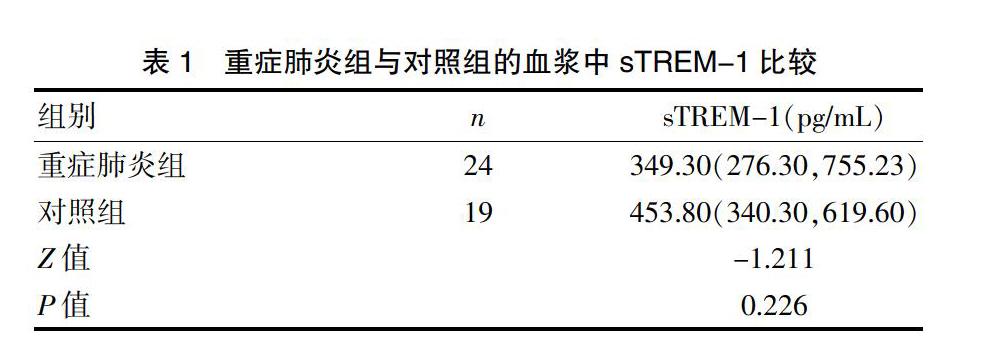
2.1 重症肺炎组与对照组的血浆中sTREM-1比较
重症肺炎组血浆sTREM-1水平与对照组比较,差异无统计学意义(Z=-1.211,P=0.226),见表1。
2.2 重症肺炎组与好转组血浆中sTREM-1、APACHE Ⅱ评分比较
重症肺炎组APACHE Ⅱ评分较好转组明显升高,差异有统计学意义(P<0.05);重症肺炎组血浆中sTREM-1与好转组比较差异无统计学意义(P>0.05),见表2。
2.3 好转组与对照组血浆中sTREM-1的比较
好转组血浆中sTREM-1与对照组比较,差异无统计学意义(P>0.05),见表3。
2.4 sTREM-1与急性生理和慢性健康评估(APACHE Ⅱ)评分相关分析
重症肺炎组患者sTREM-1与APACHE Ⅱ评分无明显相关性(r=-2.53,P=0.223)。
3 讨论
重症肺炎属于一种全身性的炎性反应,肺部感染严重,由于受到病原体、炎性因子、毒性代谢产物的侵害,重症肺炎具有发病迅速、治疗难度大等特点,可出现意识障碍、休克,导致多脏器功能衰竭,其产生与病原体感染后体内瀑布样炎性反应及抗炎反应失代偿相关,使局部炎症向全身性炎症演变,而非单纯病原菌和毒素损伤的结果。细胞因子介导的炎症反应在重症肺炎的发生、发展及转归中发挥着重要的作用。虽然在危重患者肺部感染的诊断和治疗方面已经取得了很大的进展,但为了降低发病率和死亡率,仍需要寻找更准确的生物标志物来诊断肺部感染及判断预后。
髓系细胞触发受体-1(TREM-1)属于免疫球蛋白超家族,于2000年被首次发现[6]。可溶性髓样细胞触发受体-1(sTREM-1)是TREM-1的可溶性形式,其作为调节因子在炎症反应中起着重要作用,TREM-1在细胞外细菌、真菌或炎症介质刺激时表达增加[7-8],因此可作为诊断感染性疾病的标志物[9-11]。肺炎患者肺泡灌洗液及脓毒症患者血浆内sTREM-1水平均出现增高。研究表明,sTREM-1可作为重症肺炎严重程度评估指标,在重症肺炎患者血清中高表达,可作为重症肺炎的辅助诊断[12-13]。Gibot S等[14]研究认为,sTREM-1血清水平可有效预警SIRS和脓毒症,其价值高于PCT及CRP。陈明科等[15]研究认为,腹腔引流液sTREM-1水平对腹部创伤脓毒症的诊断具有参考价值,动态监测腹腔引流液sTREM-1水平变化,有利于评估腹部创伤脓毒症的治疗效果和判断预后。Grover V等[16]研究发现,单核细胞和中性粒细胞上表达TREM-1(mTREM-1)水平, BALF中sTREM-1水平较无脓毒症证据的通气对照组与无临床感染的非通气对照组明显升高,认为包含sTREM-1在内的7-标记生物核可以准确区分VAP和非肺部感染。
但本研究却发现,重症肺炎组患者血浆sTREM-1水平较对照组患者無明显升高,差异无统计学意义;sTREM-1水平在病情好转组表达较重症肺炎组并没有明显下降。重症肺炎组患者血浆sTREM-1水平与APACHE Ⅱ评分无明显的相关性。这结果不排除其他干扰因素所致,如入选患者在入院前可能已接受抗感染或激素治疗;不同的致病菌可能会影响sTREM-1表达水平,故尚不能说明sTREM-1在重症肺炎发生、发展不起作用。当然也有研究发现sTREM-1并不能反映疾病严重程度。Bopp C等[17]研究发现,血浆中sTREM-1表达水平在SIRS组、重度脓毒症组及脓毒症休克组较对照组并没有升高,生存组和死亡组中血浆sTREM-1水平比较差异无统计学意义。一项纳入11项研究共1795例患者的Meta分析[18]显示,sTREM-1在区分SIRS 和脓毒症方面有一定帮助,然而血浆sTREM-1作为单一指标诊断脓毒症并不可靠。在新生儿迟发型败血症中sTREM-1的诊断价值不如IL-6[19]。最近Esposito S等[20]研究表明,社区获得性肺炎患儿血中sTREM-1水平难以鉴别是细菌还是病毒感染,对严重病例的鉴别能力较差。另外一项系统分析[21],就血浆sTREM-1水平在诊断儿童全身性炎症反应综合征(SIRS)脓毒症中的准确性进行系统回顾评价,该系统分析了包括961例患儿在内的9项研究,结果发现目前的资料不足以支持sTREM-1在儿童脓毒症中的诊断价值。sTREM-1作为重症肺炎或脓毒症的准确预警和判断预后的指标需持谨慎态度。
综上所述,血浆sTREM-1水平在重症肺炎组、好转组、对照组中差异无统计学意义,各组的sTREM-1水平与APACHE Ⅱ评分均无相关性,sTREM-1用于重症肺炎的病情评估、预后判断需持谨慎态度;或者说sTREM-1作为单一指标诊断评价重症肺炎并不可靠,应从临床各个方面,结合相关辅助检查及生物标志物综合评估重症肺炎病情及预后。
[参考文献]
[1] Perrone T,Quaglia F.Lung US features of severe interstitial pneumonia:Case report and review of the literature[J].Jultrasound,2017,20(3):247-249.
[2] Bouchon A,Faechetti F,Weigand MA,et al.TREM-l amplifies inflammation and is a crucial mediator of septic shock[J].Nature,2001,410(6832):1103-1107.
[3] 李冀,黄奕江,吴海洪,等. 可溶性髓样细胞触发受体 1 和降钙素原联合检测在重症社区获得性肺炎中的应用价值[J]. 海南医学,2017,28(11):1782-1785.
[4] Salih W,Schembri S,Chalmers JD.SimplificaIion of the IDSA/ATS criteria for severe CAP using meta-analvsis and observational data[J].Eur Respir J,2014,43(3):842-851.
[5] Ryan HM, Sharma S, Magee LA, et al. The usefulness of the APACHE Ⅱ score in obstetric critical care:A structured review[J]. J Obstet Gynaecol Can,2016,38(10):909-918.
[6] Bouchon A,Facchetti F,Weigand MA,et al. TREM-1 amplifies inflammationand is a crucial mediator of septic shock[J]. Nature,2001,410(6832):1103-1107.
[7] Colonna M,Facchetti F. TREM-1(triggering receptor expressed on myeloid cells):A new player in acute inflammatory responses[J]. J Infect Dis,2003,187 Suppl 2:S397-S401.
[8] Kamei K,Yasuda T,Ueda T,et al. Role of triggering receptor expressed on myeloid cells-1 in experimental severe acute pancreatitis[J]. J Hepatobiliary Pancreat Sci,2010,17(3): 305-312.
[9] Saldir M,Tunc T,Cekmez F,et al. Endocan and soluble triggering receptor expressed on myeloid cells-1 as novel markers for Neonatal sepsis[J]. Pediatr Neonatol,2015,56(6):415-421.
[10] Halim B,■zlem T,Melek ?觭,et al. Diagnostic and prognostic value of procalcitonin and sTREM-1 levels in sepsis[J]. Turk J Med Sci,2015,45(3):578-586.
[11] Xie J,Zhang XH,Zhu WY. Values for serum procalcitonin, C-reactive protein, and soluble triggering receptor expressed on myeloid cells-1 in predicting survival of patients with early-onset stroke-associated pneumonia[J]. Genet Mol Res,2015,14(2):4716-4723.
[12] 田鑫. 重癥肺炎患者血清中sTREM-1、纤维蛋白原及D-二聚体水平变化及临床意义[J].临床肺科杂志,2018, 23(9):1699-1702,1719.
[13] 赵纪维,琚国文,白丽梅. sTREM-1、IL-17、PCT及PA联合检测在重症肺炎中的诊断价值[J]. 中国现代医生,2018,56(3):34-37.
[14] Gibot S,Kolopp-Sarda MN,Béné MC,et al.Plasma level of a triggering receptor expressed on myeloid cells·l:Its diagnostic accuracy in patients with suspected sepsis[J].Ann Intern Med,2004,141(1):9-15.
[15] 陈明科,朱永,谢晓红,等. 腹部创伤脓毒症患者腹腔引流液可溶性髓样细胞触发受体-1水平变化的临床意义[J]. 疑难病杂志,2019,18(4):374-378.
[16] Grover V,Pantelidis P,Soni N,et al. A biomarker panel (Bioscore) incorporating monocytic surface and soluble TREM-1 has high discriminative value for ventilator-associated pneumonia:A prospective observational study[J]. PloS One,2014,9(10):e109686.
[17] Bopp C,Hofer S,Bouchon A,et al. Soluble TREM-1is not suitable for distinguishing between systemic inflammatoary response syndrome and sepsis surviors and nonsurvivors in the early stage of acute inflammation[J]. Eur Anaesthesiol,2009,26(6):504-507.
[18] Wu Y,Wang F,Fan X,et al.Accuracy of plasma sTREM·l for sepsis diagnosis in systemic inflammatory patients:A systematic review and meta-analysis[J].Crit Care,2012, 16(6):R229.
[19] Sarafidis K,Soubasi-Griva V,Piretzi K,et al. Diagnostic utility of elevated serum soluble triggering receptor expressed on myeloid cells(sTREM)-1 infected neonate fected neonates[J]. Intensive Care Med,2010,36(5):864-868.
[20] Esposito S,Di Gangi M,Cardinale F,et al. Sensitivity and specificity of soluble triggering receptor expressed on myeloid cells-1,midregional proatrial natriuretic peptide and midregional proadrenomedullin for distinguishing etiology and to assess severity in community-acquired pneumonia[J]. PloS One,2016,11(11):e0163262.
[21] Pontrelli G,De Crescenzo F,Buzzetti R,et al. Diagnostic value of soluble triggering receptor expressed on myeloid cells in paediatric sepsis:A systematic review[J]. Italian Journal of Pediatrics,2016,42:44.
(收稿日期:2019-29-30)