益生菌制剂对妊娠期糖尿病患者肠道微生物组成情况以及母婴结局的影响
谭莉莎 孙荣革 刘志红

[摘要]目的 研究益生菌制劑对妊娠期糖尿病(GDM)患者肠道微生物组成以及母婴结局的影响。方法 选择2017年3月~2018年9月在我院定期产检的106例GDM患者作为研究对象,将其随机分为对照组(50例)和治疗组(56例)。两组患者均进行血糖控制治疗,治疗组患者在孕龄28~37周时使用益生菌制剂治疗。比较两组患者的不良母婴结局情况,采集两组的粪便样本,进行微生物检测。结果 两组患者治疗前后丰度较高的菌均为拟杆菌属、栖粪杆菌属、普氏菌属。两组患者治疗前的菌群丰度比较,差异无统计学意义(P>0.05);对照组患者治疗前后的菌群丰度比较,差异无统计学意义(P>0.05);治疗组患者治疗后的拟杆菌属和栖粪杆菌属丰度均明显低于治疗前,普氏菌属和另枝菌属丰度均明显高于治疗前,差异有统计学意义(P<0.05);治疗组患者治疗前后的考拉杆菌属、毛螺菌属、副杆菌属、布劳特氏菌属、巨单胞菌属丰度比较,差异无统计学意义(P>0.05);治疗组患者治疗后的拟杆菌属、栖粪杆菌属、考拉杆菌属丰度均明显低于对照组,普氏菌属、另枝菌属、毛螺菌属丰度均明显高于对照组,差异有统计学意义(P<0.05);两组患者治疗后的副杆菌属、布劳特氏菌属、巨单胞菌属丰度比较,差异无统计学意义(P>0.05)。治疗组患者的不良母婴结局总发生率明显低于对照组,差异有统计学意义(P<0.05)。结论 使用益生菌制剂能够减少GDM患者不良母婴结局的发生,对GDM母娠结局的改善具有重要意义。
[关键词]妊娠期糖尿病;肠道;不良母婴结局;益生菌
[中图分类号] R574 [文献标识码] A [文章编号] 1674-4721(2019)10(b)-0118-04
[Abstract] Objective To study the influence of Probiotics Preparation on intestinal microbiota composition and maternal and infant outcomes in patients with gestational diabetes mellitus (GDM). Methods A total of 106 patients with GDM who underwent regular check-ups in our hospital from March 2017 to September 2018 were enrolled in the study. They were randomly divided into the control group (50 cases) and the treatment group (56 cases). Both groups of patients were treated with glycemic control, and the patients in the treatment group were treated with Probiotics Preparation at 28-37 weeks of gestational age. The incidence of adverse maternal and child outcomes in the two groups were compared, and the stool samples of the two groups were collected for microbiological detection. Results The bacteria with higher abundance before and after treatment in the two groups were all Bacteroides, Faecalibacterium and Prevotella. There was no significant difference in the abundance of the two groups before treatment (P>0.05). There was no significant difference in the abundance of the control group between before treatment and after treatment (P>0.05). The abundances of Bacteroides and Faecalibacterium in the treatment group after treatment were significantly lower than those before treatment, the abundances of Prevotella and Alistipes were significantly higher than those before treatment, and the differences were statistically significant (P<0.05). There were no significant differences in the abundances of Phascolarctobacterium, Lachnospira, Parabacteroides, Blautia and Megamonas between before treatment and after treatment in the treatment group (P>0.05). The abundances of Faecalibacterium and Phascolarctobacterium in the treatment group after treatment were significantly lower than those in the control group, the abundances of Prevotella, Alistipes and Lachnospira were significantly higher than those in the control group, and the differences were statistically significant (P<0.05). There were no significant differences in the abundances of Parabacteroides, Blautia and Megamonas between the two groups after treatment (P>0.05). The total incidence rate of adverse maternal and infant outcomes in the treatment group was significantly lower than that in the control group, and the difference was statistically significant (P<0.05). Conclusion The use of Probiotics Preparation can reduce the incidence of adverse maternal and child outcomes in GDM patients, which is important for the improvement of maternal outcomes in GDM.
采用SPSS 18.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;计数资料采用率表示,组间比较采用χ2检验,以P<0.05为差异有统计学意义。
2结果
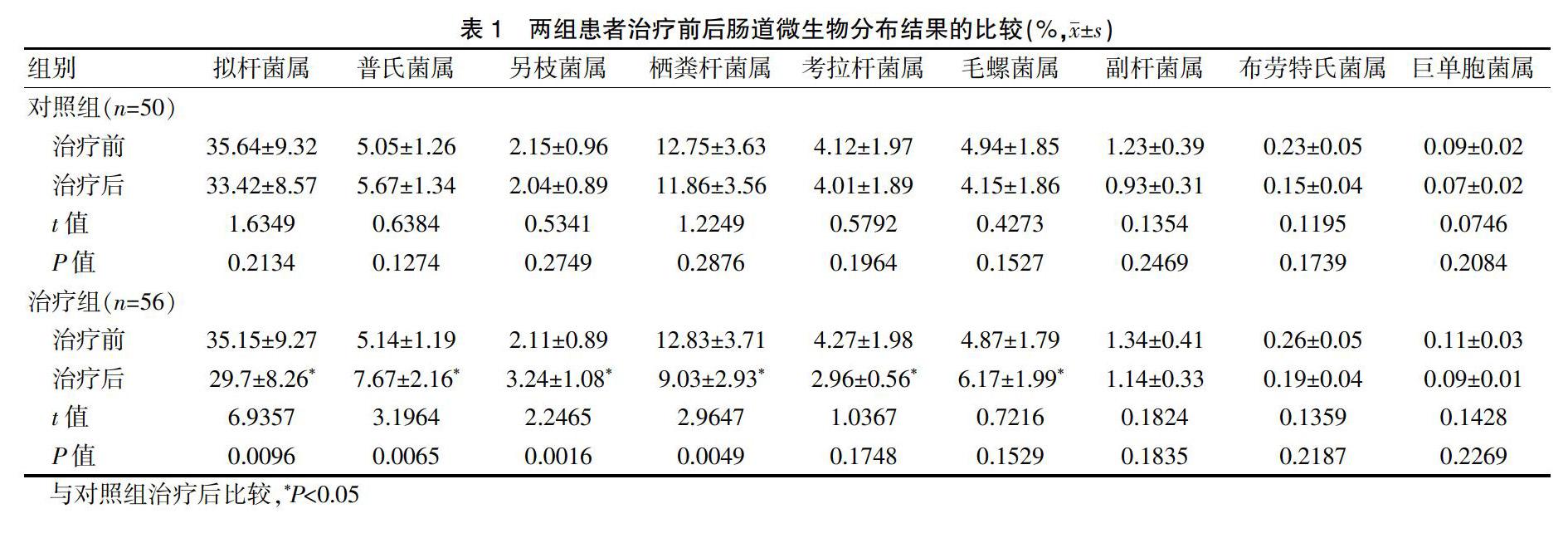
2.1两组患者治疗前后肠道微生物分布结果的比较
两组患者治疗前后丰度较高的菌均为拟杆菌属、栖粪杆菌属、普氏菌属。
两组患者治疗前的菌群丰度比较,差异无统计学意义(P>0.05);对照组患者治疗前后的菌群丰度比较,差异无统计学意义(P>0.05);治疗组患者治疗后的拟杆菌属和栖粪杆菌属丰度均明显低于治疗前,普氏菌属和另枝菌属丰度均明显高于治疗前,差异有统计学意义(P<0.05);治疗组患者治疗前后的考拉杆菌属、毛螺菌属、副杆菌属、布劳特氏菌属、巨单胞菌属丰度比较,差异无统计学意义(P>0.05);治疗组患者治疗后的拟杆菌属、栖粪杆菌属、考拉杆菌属丰度均明显低于对照组,普氏菌属、另枝菌属、毛螺菌属丰度均明显高于对照组,差异有统计学意义(P<0.05);两组患者治疗后的副杆菌属、布劳特氏菌属、巨单胞菌属丰度比较,差异无统计学意义(P>0.05)(表1)。
2.2两组患者不良母婴结局总发生率的比较
治疗组患者的不良母婴结局总发生率明显低于对照组,差异有统计学意义(P<0.05)(表2)。
3讨论
GDM的发病率正在全球上升,GDM对女性及其后代产生长期影响,包括孕妇及后代肥胖、代谢综合征和2型糖尿病的风险增加。研究认为,这可能通过微生物组传播[7]。有研究显示[8-9],肠道微生物具有调控糖代谢的作用,如罗斯氏菌和柔嫩梭菌能产生丁酸,提高机体胰岛素敏感性。此外,柔嫩梭菌、阿克曼氏菌都因为在肥胖、2型糖尿病中对代谢起有利作用而成为潜在的治疗靶点。相关研究[10]显示,益生菌可以预防治疗2型糖尿病。临床研究[11-14]显示,益生菌对防治2型糖尿病具有一定有效性,能降低患者血糖血脂等生化指标,其有效性主要与益生菌制剂的菌株选择、存活的细胞浓度和配方有关。益生菌的这种作用主要与其对肠道微生物的影响有关,提示益生菌能通过调控肠道微生物来调节糖尿病患者的糖代谢。
本研究结果显示,拟杆菌属、栖粪杆菌属、普氏菌属是两组治疗前丰度最高的3个菌属,这与之前的研究相似[2]。有研究顯示,GDM患者相对于正常孕妇,肠道细菌丰富度增加,厚壁菌门、拟杆菌和放线菌减少[11-14],而益生菌具有调节肠道菌群,有利于肠道菌群恢复正常的作用[15-19]。本研究结果显示,治疗组患者的不良母婴结局总发生率明显低于对照组,差异有统计学意义(P<0.05),提示益生菌治疗的GDM患者其不良妊娠结局发生率明显降低,这可能是因为益生菌调节GDM患者肠道菌群,有利于其血糖、血脂等指标的恢复,从而减少巨大儿等不良妊娠结局的发生。
综上所述,使用益生菌制剂能够减少GDM患者不良母婴结局的发生,对GDM母娠结局的改善具有重要意义。但是本研究也存在不足,如样本量较少、所选择的孕妇多为本地人、受外界因素影响较小,所以得出的结果不足以代表所有GDM患者的肠道菌群特征,还有待进一步的研究。
[参考文献]
[1]Billionnet C,Mitanchez D,Weill A,et al.Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012[J].Diabetologia,2017,60(4):636-644.
[2]Kuang YS,Lu JH,Li SH,et al.Connections between human gut microbiome and gestational diabetes mellitus[J].Gigascience,2017,6(8):1-12.
[3]Hasan S,Aho V,Pereira P,et al.Gut microbiome in gestational diabetes:across-sectional study of mothers and offspring 5 years post-partum[J].Acta Obstet Gynecol Scand,2018,97(1):38-46.
[4]Koren O,Goodrich JK,Cullender TC,et al.Host remodeling of the gut microbiome and metabolic changes during pregnancy[J].Cell,2012,150(3):470-480.
[5]Arihiro S,Satoshi Y,Noriko Y,et al.Intestinal microbiota is different in women with preterm birth:results from terminal restriction fragment length polymorphism analysis[J].PLoS One,2014,9(11):e111374.
[6]Lundgren SN,Madan JC,Emond JA,et al.Maternal diet during pregnancy is related with the infant stool microbiome in a delivery mode-dependent manner[J].Microbiome,2018, 6(1):109.
[7]Singh S,Karagas MR,Mueller NT.Charting the maternal and infant microbiome:whatis the role of diabetes and obesity in pregnancy?[J].Curr Diab Rep,2017,17(2):11.
[8]孙璐,李一卉,袁庆新.妊娠期糖尿病与肠道菌群关系的研究进展[J].中国临床医学,2018,25(1):141-146.
[9]黄启涛,周琳,钟梅.肠道菌群及益生菌与妊娠期并发症的相关性研究进展[J].妇产与遗传(电子版),2017,7(1):59-63.
[10]Li C,Xin L,Han H,et al.Effect of probiotics on metabolic profiles in type 2 diabetes mellitus:a meta-analysis of randomized,controlled trials[J].Medicine (Baltimore),2016, 95(26):e4088.
[11]Sáez-Lara MJ,Robles-Sanchez C,Ruiz-Ojeda FJ,et al.Effects of probiotics and synbiotics on obesity,insulin resistance syndrome,type 2 diabetes and non-alcoholic fatty liver disease:areview of human clinical trials[J].Int J Mol Sci,2016,17(6):E928.
[12]Ferrocino I,Ponzo V,Gambino R,et al.Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus (GDM)[J].Sci Rep,2018,8(1):12 216.
[13]張晓黎,周晓聪,张晓黎.益生菌与妊娠糖尿病的相关性[J].国际内分泌代谢杂志,2018,38(5):313-316.
[14]谷婷婷,赖东梅.肠道菌群与妇产科疾病的相关性研究进展[J].上海交通大学学报(医学版),2018,38(8):967-972.
[15]刘春娟,印义琼,文曰,等.胃肠道疾病患者外科围手术期应用益生菌治疗的研究进展[J].肿瘤预防与治疗,2011, 24(6):344-346.
[16]徐珂莹.益生菌制剂对老年血脂异常患者肠道微生态的临床研究[D].杭州,浙江大学,2017.
[17]杨爱国.晚孕期孕妇口服益生菌制剂对新生儿肠道菌群及脐血IL-4、IFN-γ水平的影响分析[J].临床医药文献电子杂志,2017,4(49):9564-9564.
[18]徐洪根.益生菌联合早期肠内营养辅助治疗重症急性胰腺炎的疗效[J].中国现代医生,2017,55(3):59-61,64.
[19]杨延萍.晚孕期孕妇口服益生菌制剂对新生儿肠道菌群及脐血IL-4、IFN-γ水平的影响分析[J].赣南医学院学报,2018,38(8):759-761.
(收稿日期:2019-04-12 本文编辑:任秀兰)

