左炔诺孕酮宫内缓释系统与安宫黄体酮治疗围绝经期异常子宫出血的疗效对比
周霞


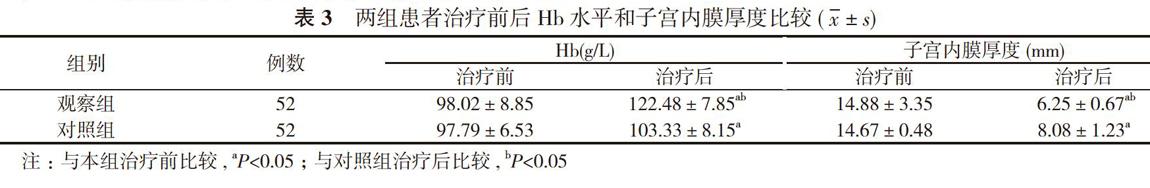
【摘要】 目的 對比左炔诺孕酮宫内缓释系统(LNG-IUS)与安宫黄体酮治疗围绝经期异常子宫出血(AUB)的临床疗效。方法 104例围绝经期异常子宫出血患者, 按照随机数字表法分为观察组和对照组, 每组52例。对照组采用安宫黄体酮治疗, 观察组采用左炔诺孕酮宫内缓释系统治疗。比较两组患者治疗前后月经量及经期时间;治疗前后血红蛋白(Hb)水平和子宫内膜厚度;临床治疗效果;不良反应发生情况。结果 治疗后, 两组患者月经量及经期时间均较治疗前显著减少, 且观察组均明显少于对照组, 差异均具有统计学意义(P<0.05)。治疗后, 两组患者Hb水平均较治疗前显著升高, 且观察组明显高于对照组, 差异均具有统计学意义(P<0.05);治疗后, 两组患者子宫内膜厚度值均较治疗前明显降低, 且观察组子宫内膜厚度值明显低于对照组, 差异均具有统计学意义(P<0.05)。观察组患者临床治疗总有效率为96.15%, 明显高于对照组的82.69%, 差异具有统计学意义(P<0.05)。治疗前后两组患者肝肾功能检查均无明显异常。治疗期间的不良反应主要为阴道点滴出血、恶心头晕及乳房胀痛, 症状均较轻微, 患者可耐受, 停药后均自行缓解。观察组患者不良反应发生率为13.46%, 与对照组的15.38%比较差异无统计学意义(P>0.05)。结论 利用左炔诺孕酮宫内缓释系统治疗围绝经期异常子宫出血的效果优于安宫黄体酮, 临床疗效确切, 用药安全, 无明显不良反应, 值得临床推广。
【关键词】 左炔诺孕酮宫内缓释系统;安宫黄体酮;围绝经期;异常子宫出血;疗效
DOI:10.14163/j.cnki.11-5547/r.2019.23.004
Comparison of the efficacy of levonorgestrel releasing intrauterine system and medroxyprogesterone acetate in the treatment of abnormal uterine bleeding in perimenopausal period ZHOU Xia. Shandong Linyi Linshu County Maternal and Child Health Hospital, Linyi 276700, China
【Abstract】 Objective To compare the clinical efficacy of levonorgestrel releasing intrauterine system (LNG-IUS) and medroxyprogesterone acetate in the treatment of abnormal uterine bleeding (AUB) in perimenopausal period. Methods A total of 104 patients with abnormal uterine bleeding in perimenopausal period were divided by random number table method into observation group and control group, with 52 cases in each group. The control group was treated with medroxyprogesterone acetate, and the observation group was treated with levonorgestrel releasing intrauterine system. Comparison was made on menstrual blood volume and duration of menstruation, hemoglobin (Hb) level and endometrial thickness before and after treatment, clinical treatment effect and occurrence of adverse reactions between the two groups. Results After treatment, both groups had significantly less menstrual blood volume and shorter duration of menstruation than those before treatment, and the observation group was obviously less than the control group. Their difference was statistically significant (P<0.05). After treatment, both groups had significantly higher Hb than that before treatment, and the observation group was obviously higher than the control group. Their difference was statistically significant (P<0.05). After treatment, both groups had obviously thinner endometrial thickness than those before treatment, and the observation group had obviously thinner endometrial thickness than the control group. Their difference was statistically significant (P<0.05). The observation group had obviously higher total effective rate of clinical treatment as 96.15% than 82.69% in the control group, and the difference was statistically significant (P<0.05). There was no significant abnormality in liver and kidney function before and after treatment in both groups. The main adverse reactions during treatment were slight bleeding of vagina, nausea and dizziness, breast swelling and pain. The symptoms were mild, tolerable and self-relief after withdrawal. The observation group had no statistically significant difference in incidence of adverse reactions as 13.46%, compared with 15.38% in the control group (P>0.05). Conclusion Levonorgestrel intrauterine sustained release system shows better effect than medroxyprogesterone acetate in treating abnormal uterine bleeding. The clinical curative effect is definite, the medication is safe, and there is no obvious adverse reaction. It is worthy of clinical promotion.