两种椎管内阻滞麻醉对潜伏期分娩镇痛产妇不同时段体温的影响
张富杰 孟凡浩 赵付华 纪云兆

[摘要] 目的 比較两种椎管内阻滞麻醉对潜伏期分娩镇痛产妇不同时段体温的影响。 方法 选择2017年6月~2018年7月河北中石油中心医院收治的240例符合条件的孕足月初产妇,依据随机数字表法分为连续硬膜外阻滞镇痛组(A组)、腰硬联合阻滞组(B组)、对照组(C组),各组80例。A组患者宫口开1~2 cm时给予连续硬膜外阻滞麻醉,实验量给予0.1%盐酸罗哌卡因8 mL,30 min后硬膜外导管接自控电子镇痛泵(电子泵内均配置0.1%盐酸罗哌卡因及0.5 μg/mL舒芬混合液100 mL)。B组患者宫口开1~2 cm时给予腰硬联合阻滞麻醉,蛛网膜下腔注射0.1%罗哌卡因3 mg,30 min后硬膜外导管接自控电子泵。C组产妇正常分娩。分娩结束立即撤出分娩镇痛。分别记录三组产妇入产房时体温、宫口开2 cm时体温、宫口开4 cm时体温、宫口开全时体温、分娩结束后2 h及24 h体温;所有产妇产前及产后24 h抽取静脉血检测C反应蛋白(CRP)及白细胞计数(WBC)水平。结果 A、B组产妇>37.3℃发热率显著高于C组,差异有统计学意义(P < 0.05)。三组产妇产后CRP水平均较产前升高,且A、B组产妇产后CRP水平高于C组,差异有统计学意义(P < 0.05)。 结论 两种椎管内麻醉均会导致分娩时体温上升,但产后24 h可恢复正常,其体温升高与感染关系不大。
[关键词] 分娩镇痛;体温;C反应蛋白;白细胞
[中图分类号] R714.3 [文献标识码] A [文章编号] 1673-7210(2019)07(a)-0121-04
Effects of two kinds of intraspinal block anesthesia on body temperature during different periods of labor in patients with latent labor analgesia
ZHANG Fujie MENG Fanhao ZHAO Fuhua JI Yunzhao
Department of Anesthesiology, Hebei Petroleum Central Hospital, Hebei Province, Langfang 065000, China
[Abstract] Objective To compare the effects of two kinds of intraspinal block anesthesia on body temperature during different periods of labor in patients with latent labor analgesia. Methods From June 2017 to July 2018, 240 eligible pregnant who was the first-time mothers in Heibei Petroleum Center Hospital were selected, according to the random number table method, they were randomly divided into continuous epidural block and analgesia group (group A), combined lumbar stiffness block and analgesia group (group B) and no labor analgesia group (group C), 80 cases in each group. Patients in group A were given continuous epidural block anesthesia when the uterine opening was 1-2 cm, and 0.1% Ropivacaine Hydrochloride was given 8 mL. After 30 min, the epidural catheter was connected with the automatic electronic analgesic pump (the electronic pump was equipped with 0.1% Ropivacaine Hydrochloride and 0.5 μg/mL mixed solution of Sufentanil 100 mL). Patients in group B were treated with lumbar hard combined block anesthesia when the uterine opening was 1-2 cm, followed by subarachnoid injection of 0.1% Ropivacaine 3 mg. After 30 minutes, the epidural catheter was connected with the automatic electronic pump. Group C was in normal delivery. Withdrawing the labor analgesia when the delivery was ending. The maternal temperature was measured at the time of delivery, the temperature at 2 cm of the uterine opening, the temperature at 4 cm of the uterine opening, the temperature at the full time of the uterine opening, and the temperature at 2 h and 24 h after the delivery in three groups. All parturients were tested for CRP and WBC by venous blood sampling before and after 24 h. Results The fever rate of >37.3℃ in group A and group B was significantly higher than that in group C, and the difference was statistically significant (P < 0.05). Postpartum CRP levels of three groups were higher than those of prenatal women, and the levels of postpartum CRP in group A and group B were higher than those in group C, the differences were statistically significant (P < 0.05). Conclusion Both kinds of intraspinal anesthesia can cause the rise of body temperature during childbirth, but it can return to normal 24 h after delivery. The increase of body temperature has little relationship with infection.
[Key words] Labor analgesia; Body temperature; C reactive protein; White blood cells
连续硬膜外分娩镇痛和腰硬联合分娩镇痛都能有效缓解分娩时疼痛,是两种可靠的分娩镇痛技术。有研究指出,无痛分娩可加速第一产程,使产妇分娩体验更优于正常分娩[1]。然而,另有研究却报道产时的产热可能与此两种椎管内麻醉有关[2-3]。也有报道称此产热与多种因素有关,如重要器官的额外耗氧量增加、使用不必要的抗生素、产生多余的儿茶酚胺以及新生儿的脓毒症[4]。就目前而言,产时的发热具体机制尚不明确。部分学者认为可能是硬膜外镇痛改变了温度的调节机制,另一些研究者则认为椎管内阻滞可能会增加绒毛膜羊毛炎的风险,从而引起产妇发热[5]。故本实验设计了两种椎管内阻滞方法,观察产程中不同时段的体温变化,同时抽取血液测量C反应蛋白(CRP)与白细胞计数(WBC),了解发热是否与感染有关。
1 资料与方法
1.1 一般资料
本研究经河北中石油中心医院(以下简称“我院”)医学伦理委员会批准,患者自愿并签署分娩镇痛知情同意书。选取2017年6月~2018年7月我院240例ASA分极Ⅰ~Ⅱ级,单胎,孕足月初产妇,年龄20~35岁。排除凝血功能障碍、穿刺点有感染等椎管内禁忌证者、阴道分娩禁忌证者、瘢痕子宫、产道异常、头盆不称、分娩前48 h有炎症疾病(如上呼吸道感染、泌尿系统感染以及生殖道感染)。240例患者依据随机数字表法分为连续硬膜外阻滞镇痛组(A组)、腰硬联合阻滞组(B组)、对照组(C组),每组各80例。
1.2 方法
三组患者入产房后均连接心电图、无创血压、脉搏氧饱和度,A组患者宫口开1~2 cm时给予连续硬膜外阻滞麻醉,经硬膜外腔向头端置管3 cm,实验量后给0.1%盐酸罗哌卡因8 mL,30 min后硬膜外导管接患者自控硬膜外镇痛泵(PCEA)。B组患者宫口开1~2 cm时给予腰硬联合阻滞麻醉,蛛网膜下腔注射0.1%罗哌卡因3 mg,30 min后接PCEA泵。A、B组电子泵内均配置0.1%盐酸罗哌卡因及0.5 μg/mL舒芬混合液100 mL。C组除常规自然分娩。电子泵均设置为负荷量6 mL/h,追加量5 mL/次,锁定时间15 min。产程中出现镇痛不全时,由助产士按自控键给药,宫口开全后,停止PCEA泵给药。均在实施镇痛30 min后,由助产士或产科医师根据宫缩情况应用缩宫素。
1.3 评估参数
①产妇体温:产妇温度恒定为26℃,记录所有产妇入产房时、宫口开2 cm时、宫口开4 cm时、宫口开全时、分娩结束后2 h及24 h的鼓膜体温。采用耳温计,产妇体温>38℃视为发热。②所有产妇入产房时及产后24 h抽取末梢静脉血检测全血WBC、CRP。
1.4 统计学方法
应用SPSS 18.0统计软件进行处理。计量资料用均数±标准差(x±s)表示,多组间比较采用单因素方差分析,进一步两两比较采用LSD-t检验;计数资料采用χ2检验;等级资料采用秩和检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 三组产妇基本情况比较
三組产妇年龄、身高、体重、孕龄比较差异无统计学意义(P > 0.05)。见表1。
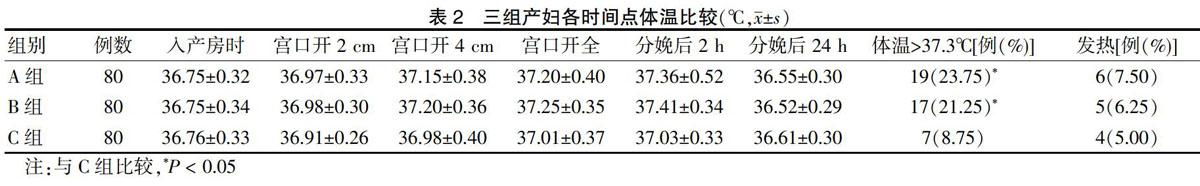
2.2 三组产妇各时间点体温比较
A、B组产妇体温>37.3℃者占比显著高于C组,差异有统计学意义(P < 0.05)。见表2。
2.3 三组产妇产前及产后WBC和CRP比较
三组产妇产后CRP水平均较产前升高,且A、B组产妇产后CRP水平高于C组,差异有统计学意义(P < 0.05)。见表3。
3 讨论
研究表明,分娩过程中运用无痛分娩会增加产妇发热的风险[6]。近期的一项研究也证实了腰硬联合麻醉在提高产妇分娩过程中的体温起了至关重要的作用[7]。故本研究对240例正常初产妇进行研究分析,观察椎管内麻醉相对于常规分娩,其体温是否有明显变化,同时观察腰硬联合麻醉与连续硬膜外麻醉在产妇分娩镇痛中对于体温的影响是否存在差异。
从病理生理角度来看,产程发热的原因很多,目前这种发热的机制并不清楚,最可能的原因是椎管内麻醉的作用导致体温调节中枢产热和散热平衡以及血管调节功能的改变[8]。正常分娩过程中因疼痛、子宫收缩以及肌肉运动的增加均能导致大量的热能产生,即使正常分娩的产妇,体温也会有轻微上升,而实施了硬膜外分娩镇痛之后,疼痛减轻导致的出汗及过度通气减少,故两者所导致的散热也将减少,与此同时,因为硬膜外镇痛导致的血管收缩可使热量丢失减少,从而使产妇热量进一步聚集体内无法排出。另外,麻醉对热、冷觉的阻滞不同步,温热觉阻滞发生较早,使得寒冷刺激持续存在,体温调节中枢得到的信息发生偏差,机体便会反应为产热增加[6]。本研究A、B、C三组随着产程的进展,体温逐渐增高,而A、B两组在产程中的发热率明显高于正常分娩,这也与Tian等[1]及冯艳等[9]的研究一致。
与此同时,许多研究也表明了阿片类药物能影响产妇的体温[5,10-12]。但是目前这种发热的机制尚不清楚,可能与药物作用于体温调节中枢有关[13]。不同的阿片类药物作用于不同的阿片类受体,这些受体主要位于下丘脑前部的视前区(POA)中[14-15]。故阿片类药物可能通过作用这些位于下丘脑视前区的受体从而影响着体温的变化。同时,因为本研究在蛛网膜下腔给予的阿片类药物,而蛛网膜下腔具有丰富的温度感觉受体和复杂的传入通路[16],有可能传入通路从初级热感觉神经元开始,由脊髓-丘脑-皮质通路产生不同的温度感觉。
目前有研究表明,产程中母亲体温的升高与炎症并无太多关系[13,17]。相反,有研究却认为发热与感染有关,而且椎管内穿刺可以增加感染的风险[18]。进一步探寻产程导致发热的原因,Sharma等[19]发现即使预防性使用抗生素,也不能降低接受椎管内阻滞分娩镇痛产妇产程中的发热率。故本研究设计了WBC和CRP产前与产后水平的比较,来观察产妇产程前后的变化。本研究发现三组产妇WBC在产程前后均无明显变化,而对CRP比较发现,进行椎管内阻滞的产妇产后水平高于正常分娩产妇。CRP是在机体受到感染或组织损伤时血浆中一些急剧上升的蛋白质,又称为急性蛋白,有观点认为它是一种非特异性的炎症标志物。椎管内阻滞的产妇CRP高于正常分娩的产妇,可能是因为后者在分娩过程中的剧烈疼痛,导致产程不敢发力,组织损伤较前者更轻微。
本组实验在研究上存在一定缺陷,实验并未进行后续的追踪,并未了解后续的发热及实验室数据的统计。其次没有细化分析,CRP可刺激单核细胞释放炎性介质如IL-6、IL-1β和TNF-α,其中IL-6是一种非常重要的炎性细胞因子,同时也是早期炎性反应的重要标志之一,有强烈的致炎活性,后续研究可进一步深挖此类因子的变化。
综上所述,两种椎管内阻滞分娩镇痛均会导致产程中体温升高,但两者并无明显差异,同时此种发热与感染无关,体温于24 h后可恢复正常。
[参考文献]
[1] Tian F,Wang K,Hu J,et al. Continuous spinal anesthesia with sufentanil in labor analgesia can induce maternal febrile responses in puerperas [J]. Int J Clin Exp Med,2013, 6(5):334-341.
[2] Chen SY,Lin PL,Yang YH,et al. The effects of different epidural analgesia formulas on labor and mode of delivery in nulliparous women [J]. Taiwan J Obstet Gynecol,2014, 53(1):8-11.
[3] 甘果,李诚,袁力勇,等.瑞芬太尼病人静脉自控镇痛用于分娩镇痛[J].医学研究杂志,2011,40(9):87-91.
[4] 薛璇,侯雯雯,贾瑞喆,等.硬膜外分娩镇痛下产间发热临床分析[J].南京医科大学学报:自然科学版,2013(12):1763-1765.
[5] Mantha VR,Vallejo MC,Ramesh V,et al. Maternal and cord serum cytokine changes with continuous and intermittent labor epidural analgesia:a randomized study [J]. Scientific World J,2012,2012:607938.
[6] Riley LE,Celi AC,Onderdonk AB,et al. Association of epidural-related fever and noninfectious inflammation in term labor [J]. Obstet Gynecol,2011,117(3):588-595.
[7] de Orange FA,Passini RJ,Amorim MM,et al. Combined spinal and epidural anaesthesia and maternal intrapartum temperature during vaginal delivery:a randomized clinical trial [J]. Br J Anaesth,2011,107(5):762-768.
[8] Irestedt L. The rise in maternal temperature associated with regional analgesia in labour is harmful and should be treated [J]. Int J Obstet Anesth,2003,12(4):284-286.
[9] 冯艳,张广兰.硬膜外分娩镇痛与产時发热的关系[J].中华围产医学杂志,2012,15(6):368-370.
[10] Baker A,Meert T. Morphine and D-amphetamine nullify each others′ hypothermic effects in mice [J]. Pharmacol Toxicol,2003,92(2):64-70.
[11] Goetzl L,Evans T,Rivers J,et al. Elevated maternal and fetal serum interleukin-6 levels are associated with epidural fever [J]. Am J Obstet Gynecol,2002,187(4):834-838.
[12] Baker AK,Meert TF. Functional effects of systemically administered agonists and antagonists of mu,delta,and kappa opioid receptor subtypes on body temperature in mice [J]. J Pharmacol Exp Ther,2002,302(3):1253-1264.
[13] de Orange FA,Passini RJ,Amorim MM,et al. Combined spinal and epidural anaesthesia and maternal intrapartum temperature during vaginal delivery:a randomized clinical trial [J]. Br J Anaesth,2011,107(5):762-768.
[14] Salmi P,Kela J,Arvidsson U,et al. Functional interactions between delta- and mu-opioid receptors in rat thermoregulation [J]. Eur J Pharmacol,2003,458(1-2):101-106.
[15] Sevarino FB,Johnson MD,Lema MJ,et al. The effect of epidural sufentanil on shivering and body temperature in the parturient [J]. Anesth Analg,1989,68(4):530-533.
[16] Romanovsky AA. Thermoregulation:some concepts have changed. Functional architecture of the thermoregulatory system [J]. Am J Physiol Regul Integr Comp Physiol,2007,292(1):R37-R46.
[17] Anim-Somuah M,Smyth RM,Cyna AM,et al. Epidural versus non-epidural or no analgesia for pain management in labour [J]. Cochrane Database Syst Rev,2018, 5:D331.
[18] Dashe JS,Rogers BB,McIntire DD,et al. Epidural analgesia and intrapartum fever:placental findings [J]. Obstet Gynecol,1999,93(3):341-344.
[19] Sharma SK,Rogers BB,Alexander JM,et al. A randomized trial of the effects of antibiotic prophylaxis on epidural-related fever in labor [J]. Anesth Analg,2014, 118(3):604-610.

