Prediction of cervical lymph node metastases in papillary thyroid microcarcinoma by sonographic features of the primary site
Xi Wei, Meng Wang, Xiaoqing Wang, Xiangqian Zheng, Ying Li, Yi Pan, Yueguo Li, Jiali Mu, Yang Yu,Dapeng Li, Ming Gao, Sheng Zhang
1Department of Diagnostic and Therapeutic Ultrasonography; 2Department of Thyroid and Cervical Tumor; 3The Third Department of Breast Cancer; 4Department of Pathology; 5Department of Clinical Laboratory, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, Tianjin's Clinical Research Center for Cancer, Tianjin 300060, China
ABSTRACT Objective: To study the sonographic features of the primary site of papillary thyroid microcarcinoma (PTMC) for the prediction of cervical lymph node metastasis during preoperative diagnosis.Methods: A total of 710 PTMC patients between 2013 and 2016 with a diagnosis of cervical lymph node metastases were reviewed.We analyzed the sonographic features of the PTMC primary site to predict ipsilateral or central lymph node metastases in univariate and multivariate models. The ratio of abutment/perimeter of the PTMC primary site was utilized to evaluate cervical lymph node status.Results: Regarding clinical characteristics, multifocality and extrathyroidal extension were associated with cervical lymph node involvement. In the multivariate regression model, calcification and the abutment/perimeter ratio of lesions were evaluated as independent factors in level VI, ipsilateral or skip cervical lymph node metastases. The cut-off value of the ratio of abutment/perimeter of the PTMC primary site (25%) was significantly correlated with cervical lymph node metastases (P = 0.000).Conclusions: Independent sonographic features, including lesion size, lesion location, calcification, and the ratio of abutment/perimeter of the primary site, were associated with cervical lymph node metastases in PTMC patients.
KEYWORDS Ultrasonography; thyroid; lymph nodes; metastasis; evaluation
Introduction
Papillary thyroid microcarcinoma (PTMC) was defined as small thyroid tumors with a size ≤ 1 cm as the greatest diameter1. Most clinical or occult papillary thyroid microcarcinomas are nonpalpable but can be detected by neck ultrasonography, computerized tomography (CT) or other imaging modalities2,3. Although papillary thyroid microcarcinoma presents indolent clinical behaviors, the local recurrent rate of PTMC was reported to be as high as 12%, with lymph node metastasis being one of the most important risk factors4-6. Thus, cervical lymph node metastases should be taken into account to assess the risk of relapse in patients with PTMC. Although active surveillance is an essential strategy in PTMC7-9, its drawback is that if patients want to accept it, they need to have no potential of cervical lymph node metastases before enrollment9. To date,surgery is the initial and standard treatment for PTMC with lymph node metastases. Therefore, the option for PTMC operation or active surveillance depends on the status of cervical lymph node metastases, which indicates that preoperative assessment is critical for PTMC patients.
Clinical examination and imaging modalities are considered effective tools to predict lymph node metastases in PTMC1. However, preoperative ultrasound (US) and CT imaging procedures have been reported to have relatively low sensitivity (20%-40%) for the detection of lymph node metastases in PTMC10because US and CT images cannot clearly present neoplastic diseases or inflammation of cervical lymph nodes. Due to this possible confusion, clinicians must accelerate the diagnostic sensitivity in the preoperative assessment of cervical lymph node involvement in PTMC patients11. This retrospective study aims to explore the clinical and US features of the primary PTMC site to identify metastatic central or lateral cervical lymph nodes to enrich PTMC treatment options.
Materials and methods
Subjects
In this retrospective study, a total of 710 PTMC patients(475 females and 235 males) were identified by pathological examination and enrolled from October 2013 to September 2016. The ages ranged from 7 to 80 years old (the average age was 44 years old). All patients were submitted to cervical lymph node dissection. Of the 710 PTMC patients,401 underwent total thyroidectomy, while the other 309 underwent thyroidectomy. A total of 486 patients underwent cervical level VI lymph node dissection, with prophylactic level VI dissection in 400 patients and therapeutic dissection in 86 cases. Therapeutic dissection of ipsilateral lymph nodes was performed in 297 patients. The retrospective study was approved by the Ethics Committee of Tianjin Medical University Cancer Institute and Hospital.
Inclusion criteria
The patients enrolled in this retrospective and consecutive study were selected on the basis of the following criteria.(1) All patients in our series underwent neck ultrasound examination for the evaluation of primary sites and cervical lymph nodes status before operation. (2) Ultrasound-guided fine needle aspiration (FNA) was performed for diagnostic purposes before the operation. Definitive diagnostic cytological findings of thyroid malignancy were determined at initial or follow-up ultrasound-guided FNA. (3) The diagnosis of primary site or cervical lymph node metastases of PTMC was pathologically confirmed after the operation(reviewed by Dr. Pan Y, who has 15 years of experience in thyroid cancer pathological diagnosis).
Ultrasound examination
Using a Phillips iU22 color Doppler ultrasonic diagnostic apparatus (Philips Medical Systems, Bothell, Washington),the 710 patients were scanned in the supine position with shoulder pillows and their necks fully exposed; along with longitudinal and transverse scans, routine examination of the bilateral thyroid lobe, isthmus and bilateral cervical lymph nodes was performed (reviewed by Dr. Wei X and Dr. Zhang S, with 10 and 25 years of experience in thyroid cancer US diagnosis, respectively). The final diagnosis of metastatic LN involvement was made by a pathologist who had 15 years of experience in histological diagnosis of cervical LNs (reviewed by Dr. Pan Y).
Ultrasound features of thyroid lesions
The size, internal echogenicity, shape, and location of the nodule, number of nodules affected, peripheral vascularity,margin, calcification, and abutment of the thyroid capsule were all preoperatively assessed using cervical ultrasonography.The ratio of capsular abutment over the lesion perimeter was calculated by sonography using Image pro plus (IPP)software (Media Cybernetics, Silver Spring, US). The measurement of abutment or protrusion/perimeter in a thyroid lesion was calculated by the average ratio (1/2) on transversal + longitudinal section of a nodule (Figures 1 and 2). For multifocality of suspicious PTMC nodules, we selected the largest nodule to calculate the abutment or protrusion/perimeter ratio. The ratio was graded by values of< 25%, 25%-50%, or > 50%. Capsular abutment is defined as a lack of intervening tissue between PTMC lesions and normal thyroid capsules. Capsular protrusion is defined as disruption of the perithyroidal echogenic line between the primary site of PTMC and the normal thyroid capsule on sonography. The ratio was finally analyzed to assist in predicting cervical lymph node status as confirmed by pathological diagnosis.
Ultrasound features of involved lymph nodes
The sonographic features of involved lymph nodes were based on various criteria, including internal microcalcifications, cystic changes, hyperechogenicity, round shape, loss of hilar echogenicity, vascularity, and size > 5 mm. The locations of lymph nodes in the neck are divided into central and lateral compartments. The central compartment (level VI) is defined as the space between the borders of the bilateral carotid arteries. The lateral compartment extends from the carotid arteries to the medial margins of the trapezius muscle, including levels II, III, IV and V, according to the definitions of the American Head and Neck Society12.Lymph node skip metastases were defined as negative central cervical LNs but positive ipsilateral cervical LNs existing in some patients with PTMC confirmedviahistopathological diagnosis.
Statistical analysis

Figure 1 The average ratio of abutment to perimeter (0.33/33%) of a thyroid nodule was calculated on both transverse (A) and longitudinal images (B). Red line: abutment of the nodule and thyroid capsule. Red line+blue line: perimeter of the thyroid nodule.
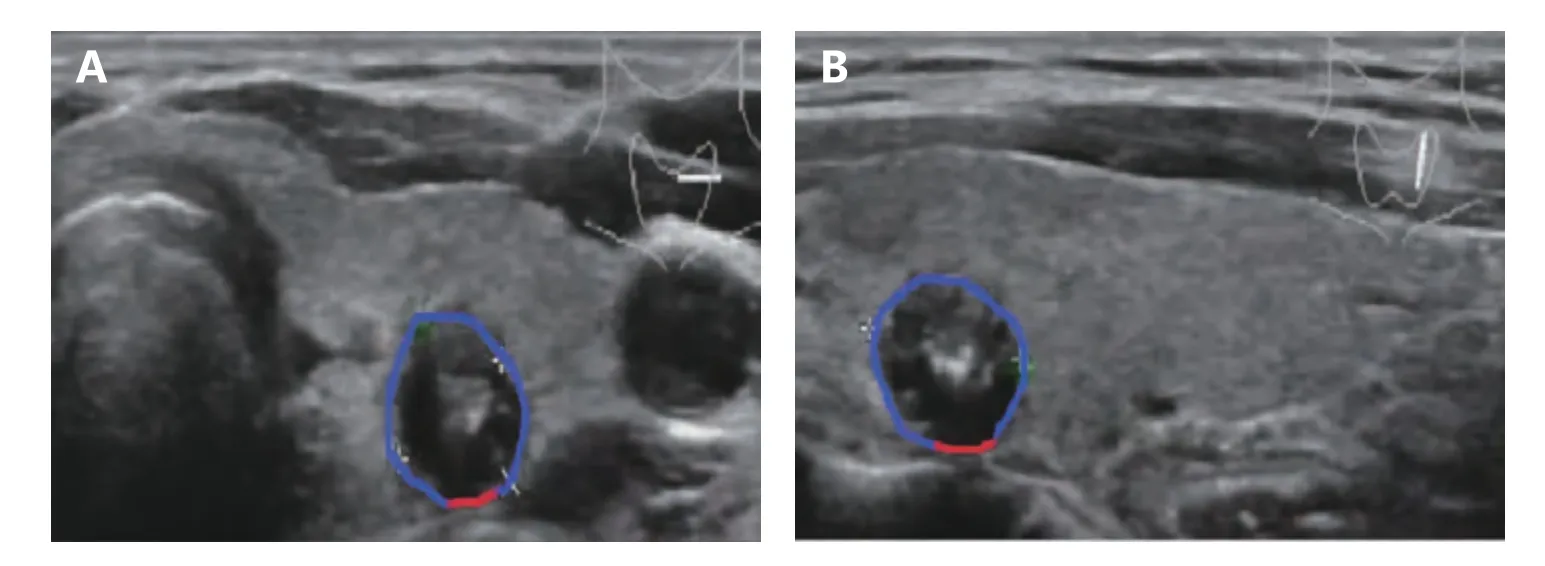
Figure 2 The average ratio of abutment and perimeter (0.12/12%) of a thyroid nodule was calculated on both transverse (A) and longitudinal images (B). Red line: abutment of the nodule and thyroid capsule. Red line+blue line: perimeter of the thyroid nodule.
The data were analyzed using SPSS 22.0 software (IBM Company, California, USA). Univariate statistical analysis was performed using the chi square test; multivariate statistical analysis was performed using the unconditional logistic regression model. The receiver operating characteristic curve (ROC) was determined using SPSS software.P< 0.05 was considered statistically significant.
Results
We reviewed 710 PTMC patients in the analysis of clinical characteristics of PTMC with cervical lymph node metastases. After a further clinical analysis of two different groups (lymph node metastases or not), we found that there was a significant difference between metastatic and nonmetastatic lymph nodes regarding multifocality and extrathyroidal extension (P< 0.05 for these two variables).No significant difference was found in age, gender or Hashimoto thyroiditis in patients with PTMC when predicting cervical lymph node involvement.
To investigate US features of the PTMC primary site for the prediction of cervical ipsilateral lymph node metastases,we analyzed univariate and multivariate logistic regression of 710 PTMC patients. Of these, 218 (30.7%) patients had positive ipsilateral cervical lymph nodes, and 492 (69.3%)had negative nodes; furthermore, 53 (7.5%) patients had positive skip cervical lymph nodes, and 657 (92.5%) had negative nodes. In the univariate model, tumor size (≤ 0.5 and > 0.5, < 1 cm), tumor location, calcification, margin and the abutment/perimeter ratio were significantly associated with increased metastatic risk of ipsilateral lymph node involvement (Table 1), and tumor size (≤ 0.5 and > 0.5,< 1 cm), tumor location, calcification, taller-than-wide dimensions and the abutment/perimeter ratio were significantly associated with skip metastasis of lymph nodes(Table 2). In the multivariate regression model, tumor size,tumor location, calcification and the abutment/perimeter ratio were evaluated as independent high-risk factors in the ipsilateral lymph node metastases group (Table 1). The tumor size, tumor location, taller-than-wide dimensions, and the abutment/perimeter ratio of the PTMC primary site were independent high-risk factors in the skip lymph node metastases group (Table 2).
There is a low sensitivity for the diagnosis of cervical central lymph nodes in PTMC by direct neckultrasonography [sensitivity: 48.3%, specificity: 83.7%, area under the curve (AUC): 0.660, 95% CI: 0.619-0.701]13(Figure 3A). For the prediction of level VI lymph node involvement in 486 patientsviaultrasound features of the primary site, the univariate regression analysis demonstrated the following results: the tumor size (≤ 0.5 and > 0.5, < 1 cm), taller-than-wide dimensions, location, echogenicity,calcification, margin and abutment/perimeter ratio of the PTMC primary site were all significant factors for the prediction of level VI lymph node metastases. The multivariate analysis showed that both calcification and the abutment/perimeter ratio were significant with regard to metastatic cervical level VI lymph nodes (P= 0.011 and 0.003, respectively, Table 3).

Table 1 Univariate and multivariate analysis of 710 PTMC primary sites with US features for predicting ipsilateral lymph node metastasis
In addition, Figure 1 shows the ratio of tumor abutment to perimeter described by IPP software, assisting in predictions of lymph node metastases (ipsilateral and level VI). We constructed a cut-off value (25%) as a predictive ratio of US features based on a previous study14and our ROC curve results (P= 0.000 and 0.003, respectively, Figure 3B and 3C). The sensitivity and specificity of the abutment/perimeter ratio of the thyroid primary site with cut-off value(25%) were 62.1% and 63.3% for level VI LN involvement and 62.2% and 52.5% for ipsilateral LN involvement. (The AUC values were 0.688 with 95% CI: 0.640-0.737 and 0.612 with 95% CI: 0.570-0.654, respectively).
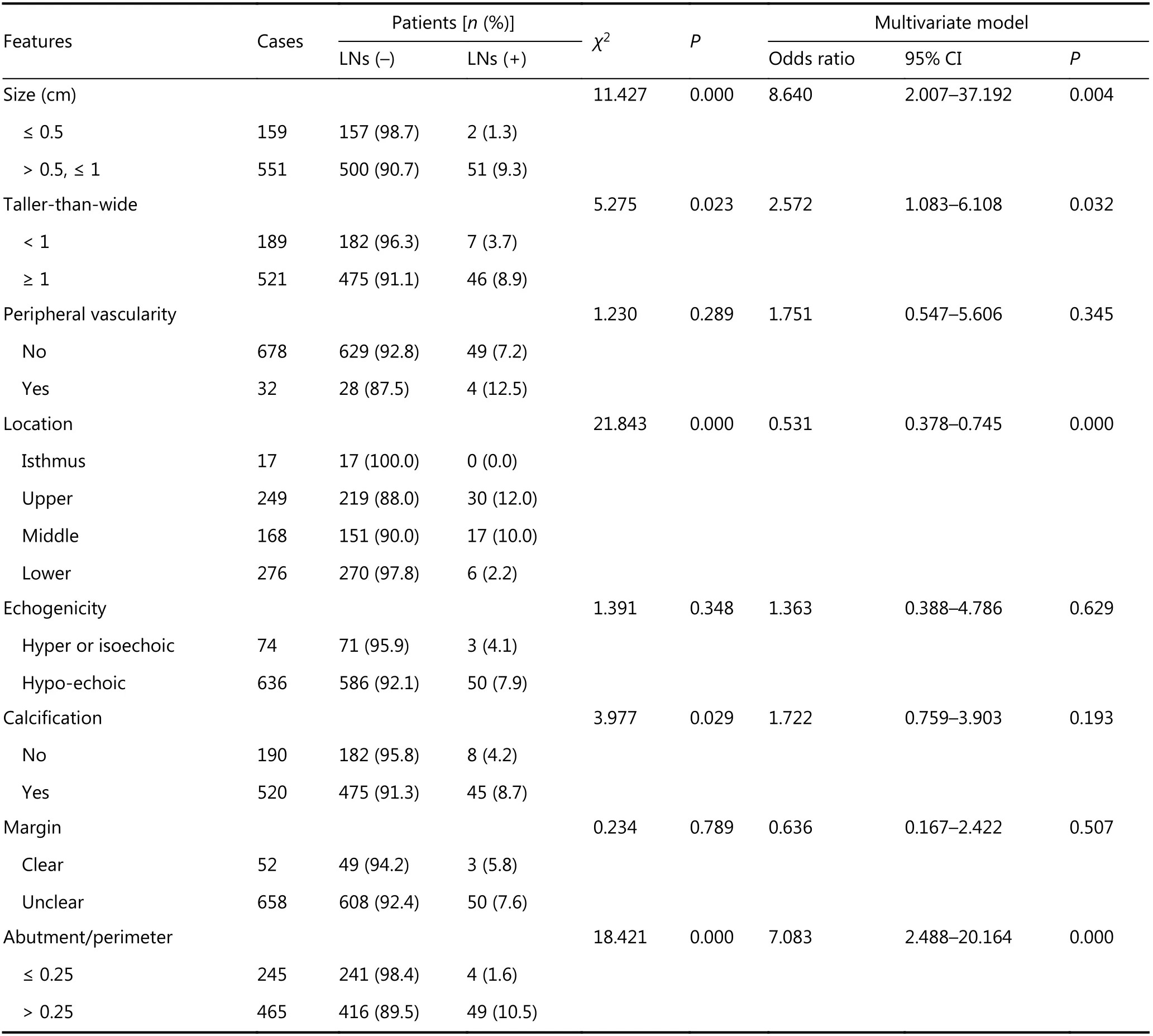
Table 2 Univariate and multivariate analysis of 710 PTMC primary sites with US features for predicting skip metastasis of lymph nodes
Discussion
There has been a substantially increasing incidence of thyroid cancer in developed countries, and most cases are PTMC,with an excellent clinical prognosis15,16. However, the prevalence of cervical lymph node metastases of PTMC has been reported to be as high as 24%-64%17. The sensitivity of both physical examination and ultrasonography in the prediction of cervical central lymph node involvement was found to be as low as 15%-30%, although ultrasound can directly assess lymph node metastases13,18. Our retrospective study aimed to predict cervical lymph node involvementviaUS features of the primary site, increasing the preoperative selection of high-risk PTMC to assist surgeons in the decision-making process.
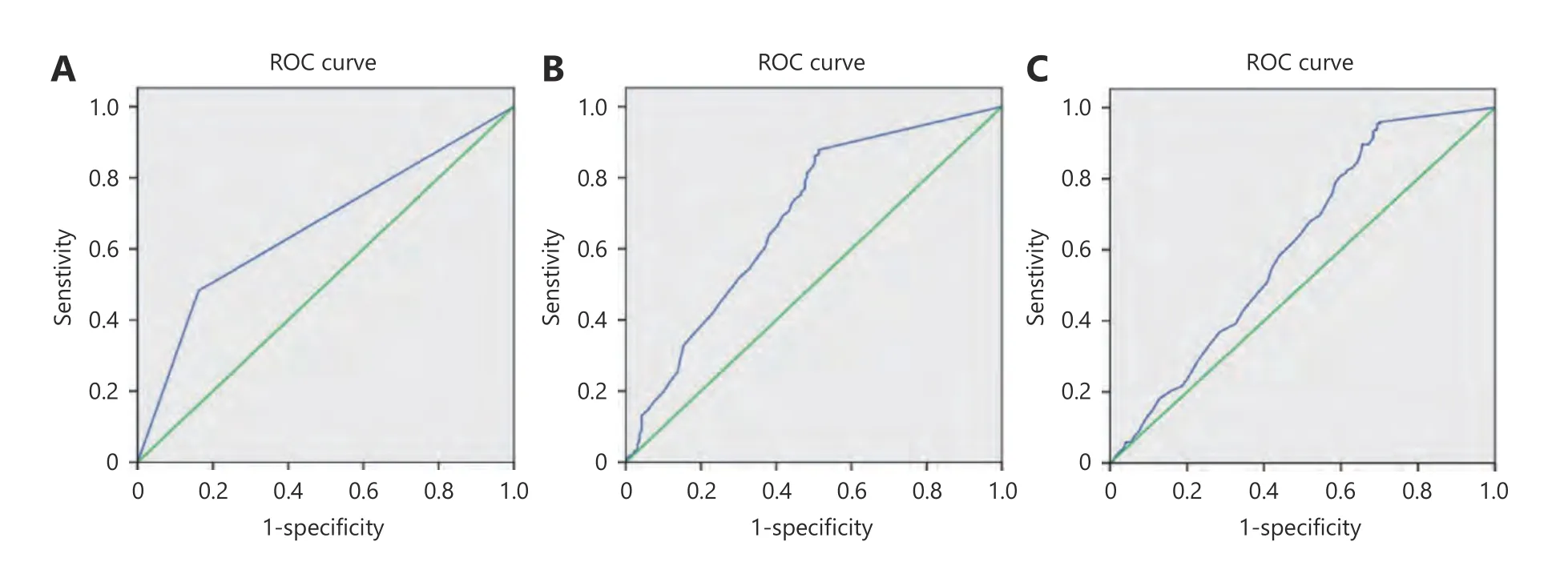
Figure 3 A. The ROC curve showed that ultrasonographic diagnosis of level VI involved lymph nodes with only evaluation of lymph nodes;The ROC curve demonstrated that assessment of level VI (B) or ipsilateral (C) involved lymph nodes via abutment/perimeter of primary thyroid lesion.
We first analyzed the correlation between clinical characteristics and positive cervical lymph node metastasis in PTMC. The clinical results suggested that multifocality and extrathyroidal extension (ETE) were both associated with cervical lymph node metastases (including ipsilateral and central LNs) in 710 PTMC patients. In agreement with a previous study, multifocality and ETE were both considered independent factors of PTMC with the involvement of lymph nodes19. Then, we investigated the correlation between sonographic features of primary thyroid lesions and cervical lymph node involvement in 710 PTMC cases. The size,location and echogenicity, calcification, margin and abutment/perimeter ratio were calculated to be associated with cervical lymph node metastases in the preoperative diagnosis of PTMC. Among these factors, we found that the cut-off value of 5 mm in nodular diameter, location,calcification and the abutment/perimeter ratio of the tumor were significantly associated with positive cervical lymph node metastasis (including ipsilateral and central LNs) of PTMC in the multivariate analysis. The “cut-off” point of the size of PTMC tumors was divided as 5, 6, 7 or 8 mm, but some results failed to identify a statistically significant value,and even a 3 mm tumor was found to be associated with disease recurrence4,20. Therefore, tumor size (> 5 mm),which was preoperatively measured by a sonographer, can assist in the decision to perform surgery.
This is the first study to establish a ratio of tumor abutment/perimeter of the primary site to assess cervical lymph node metastases, providing a visible and feasible tool to evaluate the risk of PTMC metastasis. In this process,sonographers drew a circle along the abutment to compare the measurement with the perimeter of the lesion, which provided useful information for capsular invasion to analyze the possibility of cervical lymph node status. The 1/4 (25%)perimeter of thyroid lesion was established as the cut-off value in our study. The abutment or protrusion of capsular extension was associated with lymph node metastases in PTMC. Kwak et al21and Park et al22both used an abutment perimeter ratio and calculated a diameter ratio of greater than 50% as the most accurate predictive factor in extrathyroidal extension evaluation. Lee CY et al14concluded that the thyroid capsular abutting ratio or the measure capsular protrusion was a useful predictive factor for extrathyroidal extension. Thus, preoperative sonographic features (abutment/perimeter ratio or ETE) of PTMC primary sites were proven to be a high specificity tool in the assessment of cervical lymph node metastases (including ipsilateral and central LNs) of PTMC.
Because cervical level VI LN involvement is difficult to preoperatively diagnose in PTMC, we speculated that some US features of lesions would be independent factors for the prediction of metastatic lymph nodes in the central cervical area. The results of calcification and the abutment/perimeter ratio (0.25 is cut-off value) were associated with positive lymph nodes in level VI. The abutment/perimeter ratio of 0.25 (1/4) facilitates visible risk prediction in the diagnosis of PTMC primary lesions when sonographic operators are able to draw a 1/4 line along capsular abutment or protrusion of the lesion. These categories will tailor adjuvant treatment regimens and long-term surveillance.
Determination of PTMC lesion calcification was feasible by sonography. Four patterns of calcification were classified as microcalcification, macrocalcification, rim calcification and noncalcification23. In a previous report, the microcalcification rate was higher in patients with lymph node metastasis than in those without lymph node metastasis. The mechanism of microcalcification formation in PTMC is thought to be through the rapid proliferation of cancer cells, leading to an absence of blood supply and necrosis, which consequently cause calcium accumulation and calcification24. The incidence of microcalcification in PTMC is 35.9%-53.5%, which is associated with a higher number of metastatic neck nodes23. Calcification of PTMC lesions should be carefully assessed by preoperative sonography25. In addition, we also studied the relationship between US features of PTMC primary sites and skip lymph node metastases. We found that tumor size (≤ 0.5 and > 0.5,< 1 cm), tumor location, calcification, taller-than-wide dimension and the abutment/perimeter ratio were significantly associated with skip lymph node metastases.Therefore, these US features of the PTMC primary site were risk factors for cervical lymph node metastases, aiding in tailoring PTMC treatment.

Table 3 Univariate and multivariate logistic regression analysis of 486 PTMC primary sites with US features for predicting level VI lymph node metastases
Some limitations that should be addressed are as follows.(1) This study is a retrospective analysis of patients from one center, which may contribute to a higher rate of lymph node metastases of PTMC in our series. (2) Future studies should focus on predicting occult lymph node metastases in patients who are sonographically negative. (3) In the future cohort,the clinical node negative or positive status (CN+/-) should be considered as intercrossed factors in US diagnosis of negative or positive lymph nodes, while investigating the preoperative prediction of cervical lymph nodes in PTMC patients.
Conclusions
Preoperative sonography of thyroid lesions is a practical and useful tool in the diagnosis of PTMC with involved cervical lymph nodes26. We summarized a number of independent ultrasound features, such as lesion size, lesion location,calcification and the ratio of tumor abutment/perimeter of the primary lesion, as independent risk factors in cervical lymph node metastases of PTMC.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 81771852).
Conflict of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2019年3期
Cancer Biology & Medicine2019年3期
- Cancer Biology & Medicine的其它文章
- TNFα inhibitor C87 sensitizes EGFRvIII transfected glioblastoma cells to gefitinib by a concurrent blockade of TNFα signaling
- A four-gene signature-derived risk score for glioblastoma:prospects for prognostic and response predictive analyses
- Decrease in the Ki67 index during neoadjuvant chemotherapy predicts favorable relapse-free survival in patients with locally advanced breast cancer
- Incidence, distribution of histological subtypes and primary sites of soft tissue sarcoma in China
- Prevalence and clinical significance of pathogenic germline BRCA1/2 mutations in Chinese non-small cell lung cancer patients
- Incomplete radiofrequency ablation provokes colorectal cancer liver metastases through heat shock response by PKCα/Fra-1 pathway
