平台转移技术对种植体周围组织影响的Meta分析
王蕾 刘延山 柏娜 刘杰


[摘要]目的系统评价分析平台转移(PS)技术对种植体边缘骨吸收和牙周组织健康的影响。方法计算机检索PubMed、Web of Science、Cochrane Central、CBM、CNKI、维普、万方数据库并以手工检索为辅助,收集1992—2018年间国内外公开发表的PS与平台匹配(PM)技术的随机对照试验。对所纳入的文献进行数据提取、质量评估,采用RevMan 5.3软件进行Meta分析。结果共纳入18篇文献,643例病人,1 216枚种植体(616枚PS种植体,600枚PM种植体)。Meta分析显示,PS组种植体边缘骨吸收明显少于PM组(MD=-0.28,95% CIS=-0.40~-0.16,P<0.01),探诊深度明显小于PM组(MD=-0.19,95% CIS=-0.29~-0.10,P<0.01)。结论现有的数据表明,PS技术与PM技术相比更有利于种植体周围骨组织和软组织的健康。
[关键词]平台转移;平台匹配;牙种植体;牙槽骨质丢失;牙周组织;Meta分析
[ABSTRACT]ObjectiveTo systematically evaluate the effect of platform switching (PS) on peri`-implant bone resorption and the health of periodontal tissue. MethodsPubMed, Web of Science, Cochrane Central, CBM, CNKI, VIP, and Wanfang Data were searched by computer retrieval and supplementary manual retrieval for randomized controlled trials of PS versus platform matching (PM) published in China and abroad between 1992 and 2018. The quality of the included literature was evaluated, the data were extracted, and a Meta`-analysis was performed using RevMan 5.3 software. ResultsA total of 1 216 implants (616 PS implants and 600 PM implants) from 643 patients in 18 articles were included. Meta`-analysis showed that the PS group had significantly less peri`-implant bone resorption and significantly smaller probing depth than the PM group (MD=-0.28 and -0.19,95% CIS=-0.40 to -0.16 and -0.29 to -0.10, respectively, both P<0.01). ConclusionExisting data show that PS is superior to PM in terms of their respective effect on the health of peri`-implant bone tissue and soft tissue.
[KEY WORDS]platform`-switching; platform`-matching; dental implants; alveolar bone loss; periodontium; Meta`-analysis
种植义齿具有美观、舒适、咀嚼力强等优点,受到了广大医生和病人的青睐。然而,随着种植手术的深入开展和广泛普及,也暴露出一些问题,如种植体边缘骨吸收。多种因素可造成种植体边缘骨吸收,如种植的部位、种植体周围骨的类型、手术的损伤、种植体的类型、种植体周围炎、设计不当等[1`-3]。另外,粗糙的种植体表面更容易造成菌斑的堆积,导致种植体周围炎和种植体周围骨质的吸收,因此,保留种植体周围的骨质已成为重中之重[4`-6]。20世纪90年代,LAZZARA等[7]偶然发现了基台不匹配的种植体在影像学检查中表现出更少的种植体边缘骨吸收,随即提出了平台转移(PS)的概念。已有研究表明,PS能够有效减少炎症的浸润[8]。此外,PS通过将应力集中从密质骨转移到松质骨,从颈部区域转移到基牙界面的中心,可以减少种植体周围颈部的压力[9`-12]。近年来大量研究结果证实,PS技术在种植体边缘骨保留方面存在一定的优势[13`-18]。本文通过与传统的平台匹配(PM)技术进行比较,系统评价分析PS技术对种植体边缘骨吸收和牙周组织健康的影响。现将结果报告如下。
1资料和方法
1.1文献检索
由两名研究员分别独立检索PubMed、Web of Science、Cochrane Central、CBM、CNKI、维普和万方数据库。应用主题词或自由词,以“dental implants”、“platform`-switching”、“platform`-switched implant”、“oral implant”、“marginal bone loss”、“marginal bone preservation”、“probing depth”為英文检索词,以“平台转移”、“平台匹配”、“种植体边缘骨吸收”、“探诊深度”为中文检索词,检索1992—2018年所有发表的中英文文献,根据纳入和排除标准,筛选符合标准的文献,如遇分歧,则由两位研究员讨论解决。
1.2文献纳入和排除标准
纳入标准:①临床随机对照试验研究;②病人年龄大于18岁;③病人心理健康;④随访时间至少为1年;⑤病人数量至少为10例;⑥病人在种植手术之前身体无任何炎症反应。排除标准:①病人处于孕期或哺乳期;②动物实验及非临床随机对照试验研究;③随访时间不足1年;④病人有系统疾病;⑤数据不完整的文献;⑥数据重复发表的文献。
1.3文献质量评价
由两名研究员对所纳入的文献在分配方案、分配隐藏、盲法、对失访的描述及统计处理这几个方面,运用RevMan 5.3软件按照质量评价标准进行严格的质量评估。若有分歧,则讨论解决。
1.4统计学分析
采用Cochrane协作网提供的RevMan 5.3软件进行统计学分析。用I2值判断异质性,若I2≤50%则使用固定效应模型,反之则使用随机效应模型进行Meta分析;使用漏斗图对存在的发表偏倚进行分析。以P<0.05为差异具有统计学意义。
2结果
2.1纳入文献基本特征
初步筛选出文献197篇,根据纳入和排除标准,通过仔细阅读题目、摘要和全文,初步排除文献145篇,剩余52篇,进一步排除非严格的随机对照试验文章34篇,最终纳入文献18篇[19`-36]。18篇文献中合计有643例病人,共1 216颗种植体,其中PS组616颗种植体,PM组600颗种植体。纳入文献的基本特征见表1。
2.2质量评价
纳入的18篇文献中有1篇文献为低风险,6篇文献为中度风险,其余11篇文献为高度风险。
2.3异质性检验
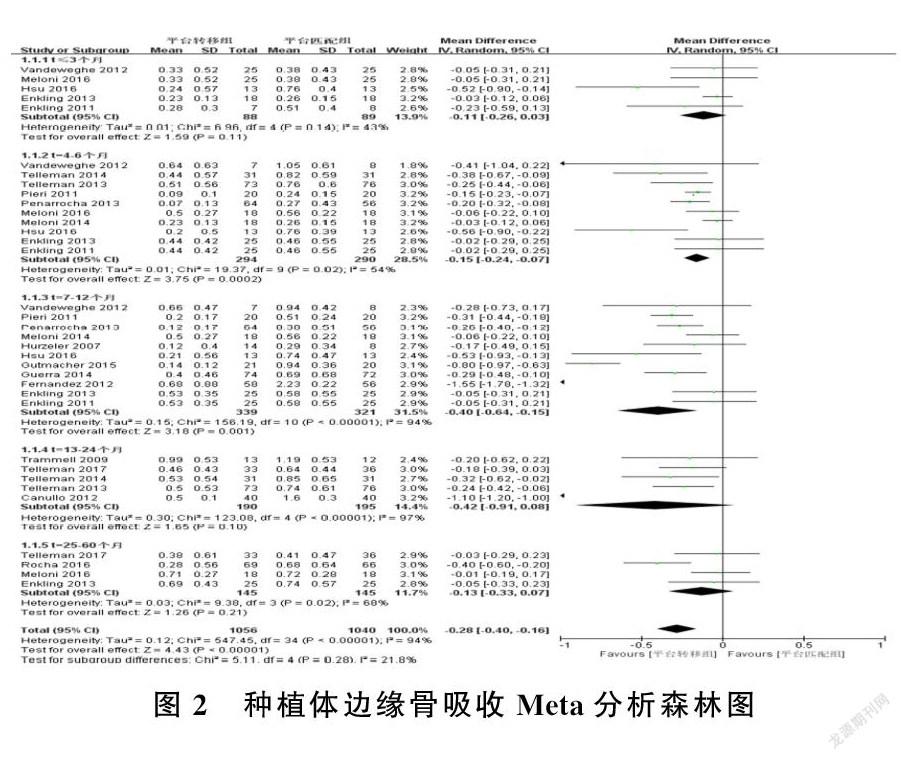
纳入的18篇文献具有异质性(Chi2=547.45,P<0.01,I2=94%),故采用随机效应模型进行 Meta分析。
2.4种植体边缘骨吸收的Meta分析
Meta分析显示,PS组种植体边缘的骨吸收明显少于PM组,差异有统计学意义(MD=-0.28,95% CIS=-0.40~-0.16,P<0.01),表明PS更有利于种植体边缘骨保存。发表偏倚分析显示,边缘骨吸收的漏斗图不对称(图1),提示文献存在发表偏倚。为探讨可能的异质性来源,本研究分别对种植体植入口腔后随访不同时间段(≤3个月、4~6个月、7~12个月、13~24个月、25~60个月)的种植体边缘骨吸收情况进行亚组分析,结果显示,在4~6个月和7~12个月这两个时间段,两组之间比较差异具有统计学意义(MD=-0.15、-0.40,P<0.01),而在其他时间段两组比较差异均无统计学意义(P>0.05)。见图2。
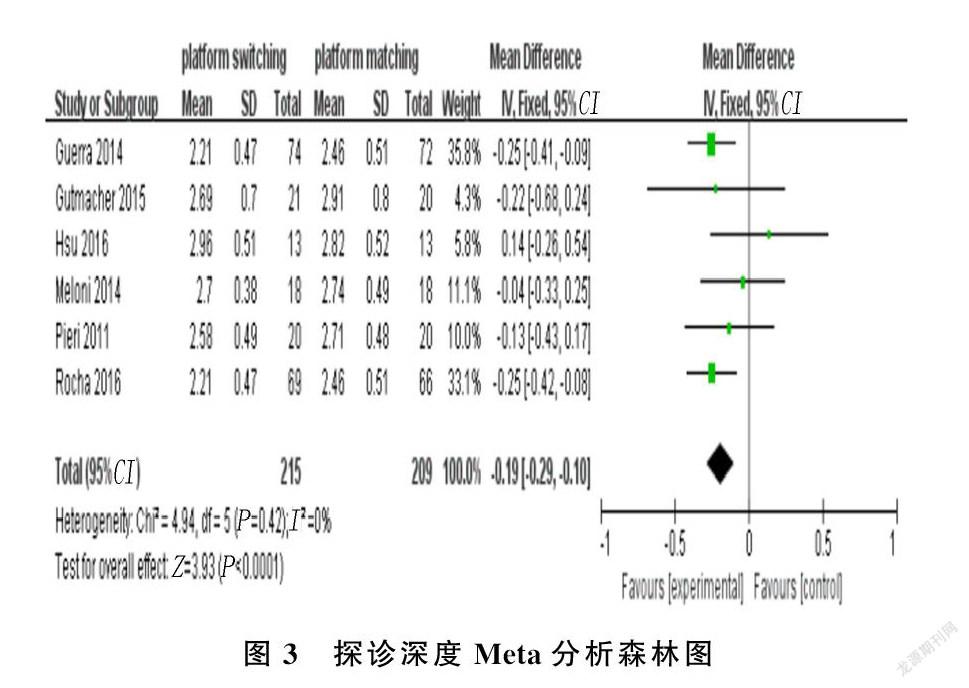
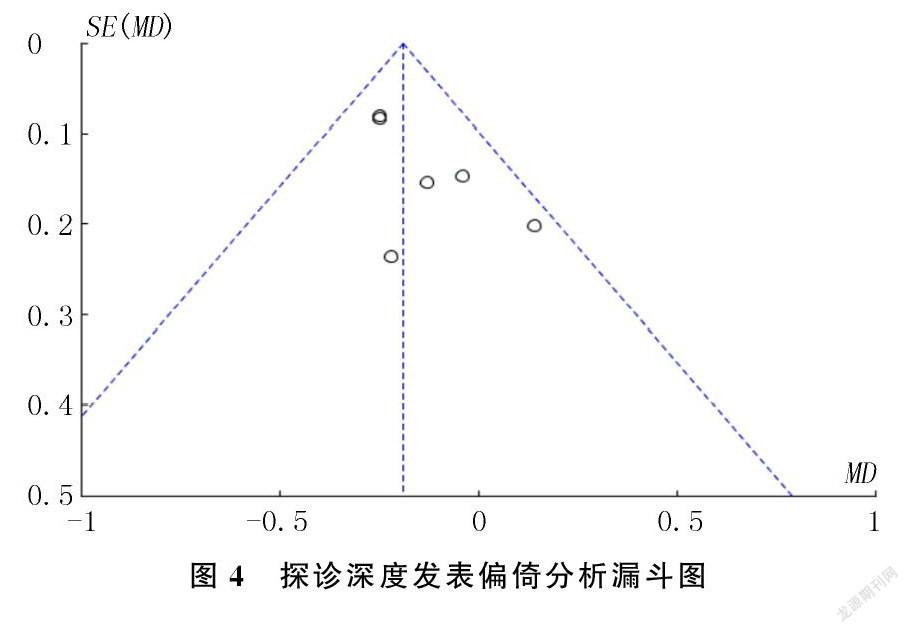
2.5探诊深度的Meta分析
Meta分析显示,PS组探诊深度明显小于PM组,差异有统计学意义(MD=-0.19,95% CIS=-0.29~-0.10,P<0.01),表明PS相对于PM更有利于种植体周围牙周组织的健康。见图3。发表偏倚分析显示,探诊深度的漏斗图对称(图4)。
3讨论
PS概念自提出以来,赢得了越来越多医生的青睐,然而PS在种植体边缘骨保留和牙周组织健康方面的影响还有待进一步探讨。到目前为止,关于PS技术严格的临床随机对照试验文献相对来说还比较匮乏。本文根据纳入和排除标准纳入了18篇严格的临床随机对照试验文献,评价了种植体PS技术和PM技术对种植体边缘骨吸收和探诊深度的影响,Meta分析结果表明,PS技术更有利于种植体边缘骨保存和牙周组织健康。
由于本文纳入文献的异质性较高,故我们根据随访的不同时间段进行亚组分析,结果表明,种植体植入口腔后4~6个月和7~12个月时,PS和PM技术在种植体边缘骨保留方面差异有统计学意义,而在其他时间段两种技术差异无统计学意义。骨组织是一种复杂的物质,其形成和生长是一个复杂的过程,并不是一蹴而就的,植入后骨组织发生一系列生理变化,成骨细胞形成骨组织,破骨细胞吸收骨组织。这两种细胞在骨的发育和形成过程中起着协同作用,这就意味着理想的骨结合不可能在短时间内完成。就目前的研究结果而言,在种植体植入口腔后4~6个月和7~12个月,PS技术更有利于边缘骨的保存。本文所纳入的文献在4~6个月和7~12个月这两个随访阶段的数量最多,更能说明PS技术有利于种植体边缘骨保存。而在≤3个月时,PS组和PM组边缘骨吸收差异无统计学意义。这种现象可能是由于种植体放置时间较短和种植体周围骨组织重塑不明显所致。此外,由于本文所纳入的一些文献没有报告在3个月内骨吸收的变化,因此在此期间进行Meta分析的文章数量较少。所以今后需要更多追蹤此阶段的文献来对种植体边缘骨吸收进行进一步的探讨。当随访时间超过12个月时,PS组和PM组边缘骨吸收差异也无统计学意义。推测可能是以下原因导致了这一现象:首先,由于随访时间相对较长,病人的依从性较差,一些有吸烟习惯的病人可能没有严格遵循医嘱继续吸烟,从而加速了种植体周围的骨吸收;其次,在所纳入的文献中,追踪时间超过1年的文献相对较少;另外,一些学者认为种植体与基台之间存在微间隙,种植体植入牙槽骨后,随着时间的延长,口腔中的一些细菌可以通过微间隙进入种植体周围,从而加速种植体边缘骨吸收[37`-39]。但是总体来说,PS技术与PM技术相比更有利于种植体周围骨的保存。
本文对探诊深度Meta分析的结果显示,两组探诊深度差异具有统计学意义,表明PS技术相对于PM技术来说更有利于种植体周围软组织的健康。但是,在本文所纳入的18篇文献中,并不是所有的文献都对探诊深度进行了测量,故今后需要收集更多高质量的文献对这一方面进行进一步的研究和分析。
本研究严格遵循PRISMA声明和PICO原则,根据纳入和排除标准,选取了18篇可信度较高的临床随机对照试验文献,对种植体周围的骨吸收状况和探诊深度进行Meta分析,结果表明PS技术相对于PM技术来说更有利于种植体周围的骨保存和软组织健康。然而,本文也存在一些缺陷,所纳入的18篇文献对种植体周围骨的测量全都是间接测量,其结果会存在一定的误差,所以测量方法有待于进一步优化。
[參考文献]
[1]SHI Junyu, JIE Ni, ZHUANG Longfei, et al. Peri`-implant conditions and marginal bone loss around cemented and screw`-retained single implant crowns in posterior regions: a retrospective cohort study with up to 4 years follow`-up[J]. PLoS One, 2018,13(2):e0191717.
[2]GOTHBERG C, GRONDAHI K, OMAR O, et al. Bone and soft tissue outcomes, risk factors, and complications of implant`-supported prostheses:5`-years RCT with different abutment types and loading protocols[J]. Clinical Implant Dentistry and Related Research, 2018,20(3):313`-321.
[3]SANZ`-SANCHEZ I, CARRILLO DE AIBORNOZ A, FIGUERO E, et al. Effects of lateral boneaugmentation procedures on peri`-implant health or disease: a systematic review and meta`-analysis[J]. Clin Oral Implants Res, 2018,29 (Suppl 15):18`-31.
[4]ADELL R, LEKHOLM U, ROCKLER B, et al. Marginal tissue reactions at osseointegrated titanium fixtures (Ⅰ). A 3`-year longitudinal prospective study[J]. International Journal of Oral and Maxillofacial Surgery, 1986,15(1):39`-52.
[5]BRAGGER U, HAFELI U, HUBER B, et al. Evaluation of postsurgical crestal bone levels adjacent to non`-submerged dental implants[J]. Clinical Oral Implants Research, 1998,9(4):218`-224.
[6]SCHWARZ F, HERTEN M, BIELING K, et al. Crestal bone changes at nonsubmerged implants(Camlog)with different machined collar lengths: a histomorphometric pilot study in dogs[J]. International Journal of Oral & Maxillofacial Implants, 2008,23(2):335`-342.
[7]LAZZARA R J, PORTER S S. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels[J]. The International Journal of Periodontics & Restorative Dentistry, 2006,26(1):9`-17.
[8]LUONGO R, TRAINI T, GUIDONE P C, et al. Hard and soft tissue responses to the platform`-switching technique[J]. International Journal of Periodontics & Restorative Dentistry, 2008,28(6):551`-557.
[9]MARTINI A P, FREITAS J, ROCHA E P, et al. Straight and angulated abutments in platform switching: influence of loading on bone stress by three`-dimensional finite element analysis[J]. Journal of Craniofacial Surgery, 2012,23(2):415`-418.
[10]MAEDA Y, MIURA J, TAKI I, et al. Biomechanical analysis on platform switching: is there any biomechanical rationale[J]? Clinical Oral Implants Research, 2007,18(5):581`-584.
[11]CHANG C L, CHEN C S, HSU M L. Biomechanical effect of platform switching in implant dentistry: a three`-dimensional finite element analysis[J]. The International Journal of Oral & Maxillofacial Implants, 2010,25(2):295`-304.
[12]CIMEN H, YENGIN E. Analyzing the effects of the platform`-switching procedure on stresses in the bone and implant`-abutment complex by 3`-dimensional fem analysis[J]. Journal of Oral Implantology, 2012,38(1):21`-26.
[13]NAYAK R, DEVANNA R, DHARAMSI A M, et al. Crestal bone loss around dental implants: platform switching vs platform matching`-a retrospective study[J]. The Journal of Contemporary Dental Practice, 2018,19(5):574`-578.
[14]SALAMANCA E, LIN J C, TSAI C Y, et al. Dental implant surrounding marginal bone level evaluation: platform switching versus platform matching`-one`-year retrospective study[J]. BioMed Research International, 2017, 2017:7191534.
[15]OSKARSSON M, OTSUKI M, WELANDER M, et al. Peri`-implant tissue healing at implants with different designs and placement protocols: an experimental study in dogs[J]. Clinical Oral Implants Research, 2018,29(8):873`-880.
[16]SPINATO S, GALINDO`-MORENO P, BERNARDELLO F A. Minimum abutment height to eliminate bone loss: influence of implant neck design and platform switching[J]. Internatio`-nal Journal of Oral & Maxillofacial Implants, 2018,33(2):405`-411.
[17]ALRABEAH G O, BRETT P, KNOWLES J C. The effect ofmetal ions released from different dental implant`-abutmentcouples on osteoblast function and secretion of bone resorbingmediators[J]. Journal of Dentistry, 2017,66:91`-101.
[18]LIU Yang, WANG Jiawei. Influences of microgap and micromotion of implant`-abutment interface on marginal bone loss around implant neck[J]. Archives of Oral Biology, 2017,83:153`-160.
[19]VANDEWEGHE S, DE BRUYN H. A within`-implant comparison to evaluate the concept of platform switching: a randomised controlled trial[J]. European Journal of Oral Implantology, 2012,5(3):253`-262.
[20]TRAMMELL K, GUERS N C, O'NEAL S J, et al. A prospective, randomized, controlled comparison of platform`-switched and matched`-abutment implants in short`-span partial denture situations[J]. International Journal of Periodontics & Restorative Dentistry, 2009,29(6):599`-605.
[21]TELLEMAN G, RAGHOEBAR G M, VISSINK A, et al. Impact of platform switching on inter`-proximal bone levels around 8.5 mm implants in the posterior region; 5`-year results from a randomized clinical trial[J]. Journal of Clinical Perio`-dontology, 2017,44(3):326`-336.
[22]TELLEMAN G, RAGHOEBAR G M, VISSINK A, et al. Impact of platform switching on peri`-implant bone remodeling around short implants in the posterior region, 1`-year results from a split`-mouth clinical trial[J]. Clinical Implant Dentistry and Related Research, 2014,16(1):70`-80.
[23]TELLEMAN G, MEIJER H, VISSINK A, et al. Short implants with a nanometer`-sized CaP surface provided with either a platform`-switched or platform`-matched abutment connection in the posterior region: a randomized clinical trial[J]. Clinical Oral Implants Research, 2013,24(12):1316`-1324.
[24]ROCHA S, WAGNER W, WILTFANG J, et al. Effect of platform switching on crestal bone levels around implants in the posterior mandible:3 years results from a multicentre randomized clinical trial[J]. Journal of Clinical Periodontology, 2016,43(4):374`-382.
[25]PIERI F, ALDINI N N, MARCHETTI C, et al. Influence of implant`-abutment interface design on bone and soft tissue le`-vels around immediately placed and restored single`-tooth implants: a randomized controlled clinical trial[J]. The International Journal of Oral & Maxillofacial Implants, 2011,26(1):169`-178.
[26]PENARROCHA`-DIAGO M A, FLICHY`-FERNANDEZ A J, ALONSO`-GONZALEZ R, et al. Influence of implant neck design and implant`-abutment connection type on peri`-implant health. Radiological study[J]. Clinical Oral Implants Research, 2013,24(11):1192`-1200.
[27]MELONI S M, JOVANOVIC S A, PISANO M, et al. Platform switching versus regular platform implants:3`-year post`-loading results from a randomised controlled trial[J]. Euro`-pean Journal of Oral Implantology, 2016,9(4):381`-390.
[28]MELONI S M, JOVANOVIC S A, LOLLI F M, et al. Platform switching vs regular platform implants: nine`-month post`-loading Results from a randomised controlled trial[J]. Euro`-pean Journal of Oral Implantology, 2014,7(3):257`-265.
[29]HUERZELER M, FICKL S, ZUHR O, et al. Peri`-implant bone level around implants with platform`-switched abutments: preliminary data from a prospective study[J]. Journal of Oral and Maxillofacial Surgery, 2007,65(7,1):33`-39.
[30]HSU Y T, CHAN H L, RUDEK I, et al. Comparison of clinical and radiographic outcomes of platform`-switched implants with a rough collar and platform`-matched implants with a smooth collar: a 1`-year randomized clinical trial[J]. International Journal of Oral & Maxillofacial Implants, 2016,31(2):382`-390.
[31]GUTMACHER Z, LEVI G, BLUMENFELD I, et al. Soft and hard tissue changes around tissue`-oriented tulip`-design implant abutments: a 1`-year randomized prospective clinical trial[J]. Clinical Implant Dentistry and Related Research, 2015,17(5):891`-897.
[32]GUERRA F, WAGNER W, WILTFANG J, et al. Platform switch versus platform match in the posterior mandible`-1`-year results of a multicentre randomized clinical trial[J]. Journal of Clinical Periodontology, 2014,41(5):521`-529.
[33]FERNANDEZ`-FORMOSO F, RILO B, MORA M J, et al. Radiographic evaluation of marginal bone maintenance around tissue level implant and bone level implant: a randomised controlled trial. A 1`-year follow`-up[J]. Journal of Oral Rehabilitation, 2012,39(11):830`-837.
[34]ENKLING N, JOEHREN P, KATSOULIS J, et al. Influence of platform switching on bone`-level alterations: a three`-year randomized clinical trial[J]. Journal of Dental Research, 2013,92(S12,12,SI):139S`-145S.
[35]CANULLO L, ROSA J C, PINTO V S, et al. Inward`-inclined implant platform for the amplified platform`-switching concept:18`-month follow`-up report of a prospective randomized matched`-pair controlled trial[J]. International Journal of Oral & Maxillofacial Implants, 2012,27(4):927`-934.
[36]ENKLING N, JOEHREN P, KLIMBERG V, et al. Effect of platform switching on peri`-implant bone levels: a randomized clinical trial[J]. Clinical Oral Implants Research, 2011,22(10):1185`-1192.
[37]HERMANN J S, BUSER D, SCHENK R K, et al. Biologic width around one`-and two`-piece titanium implants[J]. Clinical Oral Implants Research, 2001,12(6):559`-571.
[38]MOMBELLI A, VAN O A, SCHURCH E J, et al. The microbiota associated with successful or failing osseointegrated titanium implants[J]. Oral Microbiology and Immunology, 1987,2(4):145`-151.
[39]KING G N, HERMANN J S, SCHOOLFIELD J D, et al. Influence of the size of the microgap on crestal bone levels in non`-submerged dental implants: a radiographic study in the canine mandible[J]. Journal of Periodontology, 2002,73(10):1111`-1117.