Effect of low-dose aspirin administration on long-term survival of cirrhotic patients after splenectomy: A retrospective single-center study
Zhao-Qing Du, Jun-Zhou Zhao, Jian Dong, Jian-Bin Bi, Yi-Fan Ren, Jia Zhang, Bilawal Khalid, Zheng Wu,Yi Lv, Xu-Feng Zhang, Rong-Qian Wu
Abstract
Key words: Aspirin; Splenectomy; Prognosis; Hepatocellular carcinoma; Overall survival
INTRODUCTION
Splenectomy, a common surgical treatment for cirrhosis with portal hypertension and hypersplenism, can effectively reduce portal pressure, relieve symptoms, and improve liver function[1,2]. It is often used in patients with viral hepatitis-related chronic liver cirrhosis. However, portal thrombosis is not uncommon after splenectomy, documented at 4.8% to 51.5% of cases[3,4]. Previous studies revealed that portal thrombosis could induce portal hypertension, increase postoperative complications, and result in long-term poor prognosis[5-8]. Therefore, the treatment for portal vein thrombosis after splenectomy is particularly significant.
Anticoagulant therapy reduces the incidence of post-splenectomy portal thrombosis by inhibiting thrombus formation. In this regard, many cirrhotic patients take oral anticoagulants including low-dose aspirin after splenectomy[9,10]. However,the long-term impact of postoperative aspirin on cirrhotic patients after splenectomy remains unknown. The purpose of this study was to investigate the effect of low-dose aspirin therapy on HCC development and long-term overall survival in patients who underwent splenectomy for cirrhosis-related portal vein hypertension and hypersplenism.
MATERIALS AND METHODS
Study populationFrom January 2000 to December 2014, a total of 1662 patients were diagnosed with cirrhosis-related hypersplenism and portal hypertension at the First Affiliated Hospital of Xi'an Jiaotong University. Among them, 295 (17.75%) patients underwent splenectomy, of whom 31 (10.51%) were excluded because they had serious coagulation disorders, cardiovascular diseases, or malignant tumors, or used warfarin or low-molecular-weight heparin after surgery instead of aspirin. The remaining 264 patients were enrolled in this study. Among these patients, 109 took aspirin after surgery. Those who did not start taking it within seven days after surgery, who took less than one year, or who did not follow the doctor's advice were excluded. Finally,59 patients were included in the aspirin group. This group of patients took aspirin daily at a basic dose of 100 mg. The study was approved by the Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University and performed in accordance with the provisions of the Helsinki Declaration. No written informed consent was obtained for the retrospective nature of this study.
Data collectionAll clinical variables of these patients were obtained from the electronic medical record system. The general clinical data collected in this study included age, gender,hepatitis status, and underlying concurrent diseases. Laboratory results were collected on the first day after admission, containing routine blood count, liver function, coagulation test, alpha fetoprotein (AFP), and Child-Pugh score. Intraoperative blood loss, spleen size and volume, surgery methods, hospitalization stay, and postoperative complications were also obtained. Portal vein thrombosis was checked by ultrasonography after splenectomy during hospitalization, and anticoagulation information included the initial use of the drugs and detailed name of the drugs.
Follow-upAll patients were followed until October 2017. The median follow-up time was 54(interquartile range: 40, 87.6) mo. The follow-up content mainly included aspirin drugs, clinical manifestations, laboratory examination, and ultrasound imaging findings. All patients received the relevant follow-up. The overall survival (OS) was recorded from the surgery time to last follow-up, and hepatocellular carcinoma(HCC) occurrence was recorded from the surgery to the last time without tumor. HCC was diagnosed based on imaging results and laboratory tests. To reduce the follow-up bias, two researchers completed the work independently.
Statistical analysisContinuous variables are expressed as the mean ± standard deviation or median (minmax). Categorical variables are expressed as frequency and percentage. To calculate the difference between two groups, the Student’s t-test or Wilcoxon test was used for continuous variables and the chi-squared test or Fisher’s exact test for categorical data. For three or more groups, analysis of variance was used. Survival curves were estimated using the Kaplan-Meier method and statistical differences were calculated by the log-rank test. If statistical significance was found by univariate analysis, the factor will continue to be calculated through the multivariate log-regression model.All statistical analyzes were performed using PASW Statistics 18.0 software (IBM Corporation, Armonk, NY, United States). Survival curves have been beautified with Graphpad prism 6.0 software (GraphPad Software, Inc. La Jolla, United States). Ρ <0.05 was considered statistically significant.
RESULTS
Patient demographics and characteristicsThe demographics and baseline clinical characteristics of the 264 patients are shown in Table 1. The average age of the patients was 45 years (range: 20-67 years), and there were 194 (73.48%) males and 70 (26.52%) females. Among all the patients, 248(93.94%) had hepatitis B virus (HBV) infection, 14 (5.30%) had hepatitis C virus (HCV)infection, and 2 (0.76%) had both HBV and HCV infections; 33 (12.50%) had a history of alcohol consumption and 65 (24.62%) had a smoking history; 58 (21.97%) and 21(7.95%) had hypertension and diabetes, respectively; 71 (26.89%) had a platelet count below 30 (×109/L) at admission. The average values of fibrinogen and alpha fetoprotein (AFP) at admission were 1.89 g/L (range: 0.60-5.36 g/L) and 10.83 mg/L(range: 0.76-140.90 mg/L), respectively. At admission, 80 (30.30%) cases had Child-Pugh grade A liver function, 165 (62.50%) had Child-Pugh grade B, and 19 (7.20%)had Child-Pugh grade C. The average amount of bleeding during surgery was 425 mL(range: 50-2000 mL). The spleen volume and spleen size were 1410 (range: 156-4896 mm3) and 158 (range: 12-230 mm), respectively. Two hundred and twenty-eight(86.36%) patients underwent open laparotomy and the other 36 (13.64%) patients underwent laparoscopic surgery. The mean length of hospital stay was 27 d (range:11-125 d). Among these patients, 47 patients (17.80%) developed portal vein thrombosis during hospitalization after splenectomy. A total of 59 patients, including 21 who developed portal vein thrombosis and 38 who did not, were given 100 mg/d aspirin within seven days after surgery for at least one year.
Effect of postoperative long-term low-dose aspirin therapy on the development of HCCIn this cohort, 41 (15.53%) patients developed HCC during follow-up and Kaplan-Meier analysis showed that the incidence of HCC in patients with postoperative aspirin (log-rank test, Ρ = 0.028) was significantly lower than that in patients without aspirin (Figure 1). Univariate and multivariate analyses demonstrated that not taking postoperative aspirin (Ρ = 0.016) was the independent risk factor for the development of HCC after splenectomy (Table 2).
成本较高,需要大量人力、物力,且对场所也有要求,要有标准化的考场以及专门的录像设备,便于事后反馈和取证。另外,OSCE毕竟是虚拟的非真实情境,因此也有人提出质疑,说因为受试者知道是考试,所以会“演”出爱心,因此没法测出应试者真正的人文素养。此外,测试结果客观上受考试环境、评分表设计、标准化病人表现以及考官因素影响(如考官注意力不集中等),因此考试判定要有3个考官,如果出现争议,以多数考官的意见为准。
Effect of postoperative long-term low-dose aspirin therapy on overall survival after splenectomyAt the end of follow-up, 37 (14.02%) patients died due to end-stage liver diseases or other serious complications. Overall survival rates at 3, 5, and 10 years after splenectomy were 93.18%, 89.77%, and 87.12%, respectively (Table 3). It could be seen that the overall survival of patients in the aspirin group were significantly better than that of the patients who did not receive early postoperative aspirin after surgery (logrank test, Ρ = 0.041, Figure 2). Next, we used univariate and multivariate analyses to explore factors affecting overall survival after splenectomy. As shown in Table 4, the only factor that was independently associated with overall survival was early postoperative aspirin therapy (Ρ = 0.044). And other factors such as gender, age > 60 years, underlying liver diseases, Child-Pugh score, surgical approach, and spleen volume did not show a statistically significant effect on overall survival.
DISCUSSION
Cirrhotic patients who underwent splenectomy are at a high risk of developing thrombosis[11]. Due to its convenient administration and relatively low bleeding risk,low-dose aspirin is often used after splenectomy[12]. However, the long-term effects of low-dose aspirin in this specific patient population have not been clarified. Here, we found for the first time that long-term low-dose aspirin use after splenectomy significantly reduced HCC incidence and improved overall survival in cirrhotic patients with hypersplenism.
Splenectomy is a routine surgical procedure[1]. Many studies have indicated that splenectomy improved liver function, delayed hepatic fibrosis, corrected cytopenia,and expanded treatment options for the underlying liver disease[13]. Thus, it is commonly used to treat hypersplenism for patients with cirrhosis. Liver cirrhosis is a major risk factor for HCC[14-16]. Hypersplenism is correlated with an increased risk of HCC in patients with post-hepatitis cirrhosis and splenectomy might reduce HCC risk in those patients[17,18]. A recent retrospective study of 2678 cirrhotic patients with hypersplenism showed that 33.0% of cirrhotic patients who did not undergo splenectomy developed HCC, while only 17.3% of those who underwent splenectomy developed HCC[18]. In the current cohort of 264 cirrhotic patients who underwent splenectomy, a total of 41 (15.5%) developed HCC during follow-up, which is consistent with the early report.
Taking a low-dose aspirin daily has been shown to decrease the risk of developing or dying from many types of cancer[19-21]. A recent study[22]on the chemopreventive effect of aspirin on HCC and death due to chronic liver disease showed that any aspirin use at baseline was associated with a reduced risk of both HCC development and mortality. Non-aspirin NSAID users, on the other hand, were not at a reduced risk of developing HCC[20,23]. The anticancer effects of aspirin are mediated through several interconnected mechanisms[24,25]. Aspirin blocks the production of COX1 and COX2, inhibits WNT-β-catenin signaling, and inactivates platelets and the host immune response[26-28]. Chronic or prolonged inflammation can create an environment in which cancer thrives. Chronic viral hepatitis is the major cause of HCC. Immune-mediated inflammatory responses are considered to be the predominant cause of HCC transformation during chronic viral hepatitis. The combined anti-platelet and anti-inflammatory effects of aspirin may specifically prevent inflammation-associated tumorigenesis under such conditions[16,29]. Oral administration of aspirin can be used for long-term treatment of patients at risk of thrombosis. Thus, in cirrhotic patients with hypersplenism, daily low-dose aspirin therapy should be recommended after splenectomy.
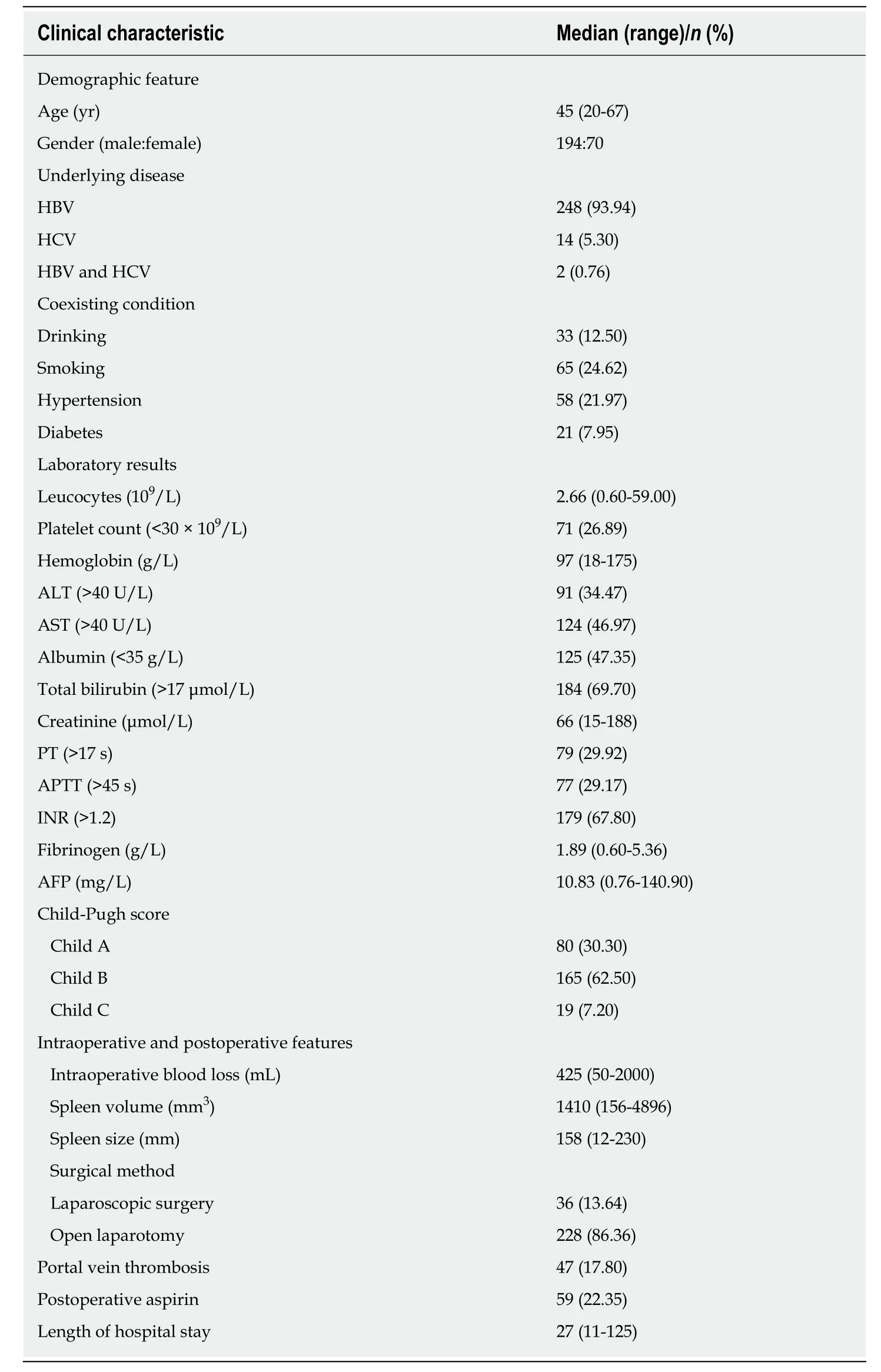
Table 1 General clinical characteristics of the patients

Figure 1 Effect of postoperative long-term low-dose aspirin therapy on the development of hepatocellular carcinoma in cirrhotic patients after splenectomy. Differences in hepatocellular carcinoma (HCC) development between cirrhotic patients who received long-term low-dose aspirin (aspirin group) and those who did not (control group) were compared. The incidence of HCC was assessed by the Kaplan-Meier method and compared by the logrank test. HCC: Hepatocellular carcinoma.
The major strength of our study was the long-term follow-up. However, there were also some limitations in the present study. First, the data in this study originated from a single center, therefore the sample size was relatively small and the incidence of postoperative mortality and morbidity was low. For instance, a relatively small proportion of patients died during follow-up, which may have limited the robustness of the multivariable analysis for adjustment for confounding factors. Second, we only considered the long-term use of low-dose aspirin after splenectomy as anticoagulant therapy in this study; however, some patients, especially those who developed portal vein thrombosis, also received other anticoagulants for a short period of time. More data are needed to investigate the long-term effects of other anticoagulants after splenectomy. Third, only viral hepatitis-related cirrhotic patients were enrolled in this study. Therefore, whether long-term low-dose aspirin has the same effect in preventing HCC development in patients with alcohol-related cirrhosis needs to be determined. Moreover, whether taking a low-dose aspirin daily reduces the risk of developing HCC in cirrhotic patients without splenectomy also warrants further investigation. Finally, due to the retrospective nature of this study, the results were subject to some uncontrollable biases, so further prospective studies would be necessary.
In summary, post-splenectomy long-term administration of low-dose aspirin reduces the incidence of HCC and improves the long-term overall survival in patients with viral hepatitis-related cirrhosis. Thus, long-term low-dose aspirin therapy should be recommended to cirrhotic patients with hypersplenism after splenectomy.

Table 2 Univariate and multivariate analyses of risk factors for the development of hepatocellular carcinoma after splenectomy
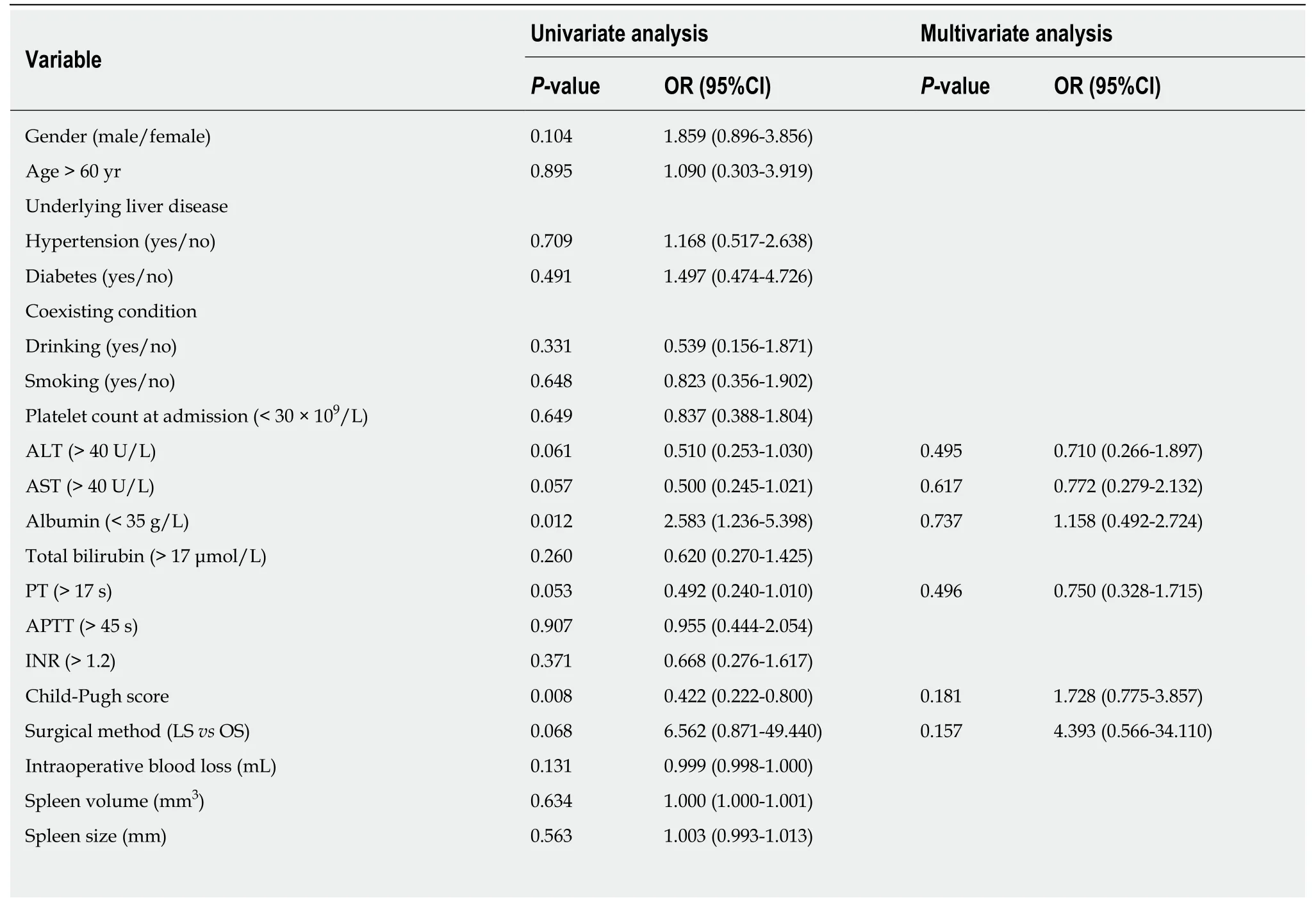
Table 3 Univariate and multivariate analyses of risk factors for overall survival
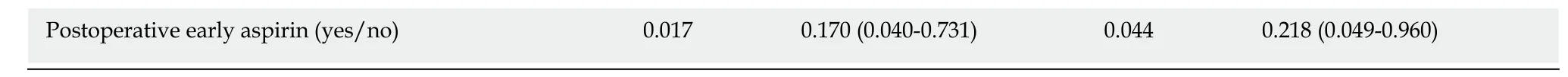
ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; PT: Prothrombin time; APTT: Activated partial thromboplatin time; INR: International normalized ratio; LS: Laparoscopic surgery; OS: open surgery.

Figure 2 Effect of postoperative long-term low-dose aspirin therapy on overall survival of cirrhotic patients after splenectomy. Differences in overall survival rates between cirrhotic patients who received long-term low-dose aspirin (aspirin group) and those who did not (control group) were compared. The survival rate was assessed by the Kaplan-Meier method and compared by the log-rank test.
ARTICLE HIGHLIGHTS
Research backgroundCirrhosis is a major risk factor for the development of hepatocellular carcinoma (HCC). Portal vein thrombosis is not uncommon after splenectomy in cirrhotic patients, and many such patients take oral anticoagulants including aspirin. However, the long-term impact of postoperative aspirin on cirrhotic patients after splenectomy remains unknown.
Research motivationThe motivation of this research was to investigate the effect of low-dose aspirin therapy on HCC development and long-term overall survival in patients who underwent splenectomy for cirrhosis-related portal vein hypertension and hypersplenism.
Research objectivesThe main objectives of this study was to investigate the effect of postoperative long-term lowdose aspirin on the development of HCC and long-term survival of cirrhotic patients after splenectomy.
Research methodsThe clinical data of 264 adult patients with viral hepatitis-related cirrhosis who underwent splenectomy at the First Affiliated Hospital of Xi’an Jiaotong University from January 2000 to December 2014 were analyzed retrospectively. Among these patients, 59 who started taking 100 mg/d aspirin within seven days were enrolled in the aspirin group. The incidence of HCC and overall survival were analyzed.
Research resultsForty-one (15.53%) patients developed HCC and 37 (14.02%) died due to end-stage liver diseases or other serious complications in this study. Postoperative long-term low-dose aspirin therapy reduced the incidence of HCC from 19.02% to 3.40% after splenectomy. Univariate and multivariate analyses showed that not undertaking postoperative long-term low-dose aspirin therapy was the only independent risk factor for the development of HCC. Similarly, patients in the aspirin group survived longer than those in the control group. Univariate and multivariate analyses showed that the only factor that was independently associated with improved overall survival was postoperative long-term low-dose aspirin therapy.
Research conclusionsPost-splenectomy long-term administration of low-dose aspirin reduces the incidence of HCC and improves the long-term overall survival in patients with viral hepatitis-related cirrhosis.
Research perspectivesLong-term low-dose aspirin therapy should be recommended to cirrhotic patients with hypersplenism after splenectomy. Further prospective and multi-center studies should be performed to verify our conclusions.
 World Journal of Gastroenterology2019年28期
World Journal of Gastroenterology2019年28期
- World Journal of Gastroenterology的其它文章
- Role of sodium-glucose co-transporter-2 inhibitors in the management of nonalcoholic fatty liver disease
- lmportance of fatigue and its measurement in chronic liver disease
- Acute kidney injury spectrum in patients with chronic liver disease:Where do we stand?
- Neoadjuvant and adjuvant treatment strategies for hepatocellular carcinoma
- Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery
- Current approaches to the management of patients with cirrhotic ascites
