Leishmaniasis in the Argentine Republic: Temporal and geographical distribution from 2013 to 2017
Germanó María J, Salomón María C, Neira Gisela, Lozano Esteban,4, Mackern-Oberti Juan P,4,Cargnelutti Diego E,✉
1Consejo Nacional de Investigaciones Científicas y Técnicas, Centro Científico y Tecnológico de Mendoza, Instituto de Medicina y Biología Experimental de Cuyo, Mendoza, Argentina
2Universidad Nacional de Cuyo, Facultad de Ciencias Médicas, Área de Parasitología, Mendoza, Argentina
3Universidad Juan Agustín Maza, Facultad de Ciencias Veterinarias y Ambientales, Centro de Investigación en Parasitología Regional, Mendoza, Argentina
4Universidad Nacional de Cuyo, Facultad de Ciencias Médicas, Instituto de Fisiología, Mendoza, Argentina
Keywords:Leishmaniasis Epidemiology Argentine Republic Temporal distribution Geographical distribution
ABSTRACT Objective: To assess the temporal and geographical distribution of confirmed cases of cutaneous, mucocutaneous and visceral leishmaniasis in the Argentine Republic from 2013 to 2017.Methods: A retrospective study was carried out using data collected from the Integrated Surveillance Bulletin database of the National System of Health Surveillance. Confirmed cases of cutaneous, mucocutaneous and visceral leishmaniasis up to the 52nd epidemiological week of each year was included.Results: In the 5 years period, 1 295 confirmed leishmaniasis cases were reported in the Argentine Republic. One thousand twenty-eight (1 028) cases corresponded to cutaneous leishmaniasis (87.10%), being the most common type of leishmaniasis. Mucocutaneous leishmaniasis was in the second place in the country with 115 cases reported, mostly in the Northwest and Northeast regions. A total of 52 individuals with visceral leishmaniasis were identified and Misiones Province was the most affected.Conclusions: It is important to analyze the temporal and geographical distribution of leishmaniasis in order to provide an adequate management and surveillance.
1. Introduction
Leishmaniasis is a group of diseases caused by different parasites belonging to the Trypanosomatidae family, genus Leishmania,which is transmitted to humans by the bite of the sandfly species belonging to Lutzomyia genus in America. The species involved in the transmission of leishmaniasis in the Argentine Republic are:Lutzomyia (Lu.) [Nyssomyia (N.)] whitmani, Lu. (N.) neivai, Lu.[Migonemyia (Mg.)] migonei and Lu. [Evandromyia (Ev.)] cortelezzii(to cutaneous and mucocutaneous leishmaniasis) and Lu. longipalpis(to visceral leishmaniasis)[1]. Four species of Leishmania have been identified in human cases in the Argentine Republic: Leishmania(L.) braziliensis, L. amazonensis, L. guyanensis, which are associated with cutaneous leishmaniasis and L. infantum, linked to visceral leishmaniasis[1].
The infection can be asymptomatic or lead to a spectrum of diseases with different clinical characteristics, such as cutaneous,mucocutaneous and visceral leishmaniasis according to the Leishmania species and host background[1]. It is estimated that about 12 million people are affected by the disease; furthermore, an estimated 50 000 to 90 000 new cases of visceral leishmaniasis, and 600 000 to 1 000 000 new cases of cutaneous leishmaniasis occur annually[2].
Leishmaniasis is a re-emerging infectious disease, and it has been categorized by the World Health Organization (WHO) as one of the neglected diseases, mainly affecting low income populations with restricted access to health services[2].
Leishmaniasis is endemic in the Argentine Republic and 17 other American countries[3] and it is of compulsory notification in all these countries. The National Disease Surveillance System is used to collect data on the occurrence of leishmaniasis in some countries,while in others there are specific tools for data collection[4].Unfortunately, there is no updated study of overall epidemiological data on human leishmaniasis in the Argentine Republic, except for reported leishmaniasis cases in the Northwest of the Argentine Republic[5].
Health indicators contain data that provide important information regarding to the status and the performance of a health system. They reveal the sanitary conditions of a population and are suitable for surveillance. These indicators provide inputs for analysis, promoting professional analytical capacity and the development of information systems[6]. In consequence, the indicators are used by governments and international organizations as tools to guide health policy, to administer resources and to execute public health strategies.
The aim of this study is to describe the temporal and geographical distribution of leishmaniasis cases in the Argentine Republic between 2013 and 2017.
2. Materials and methods
2.1. Study area
This study was conducted in the Argentine Republic, the eighth largest country in the world and the second largest in Latin America,with a total area of 3 761 274 km2. The Argentine Republic comprises 23 provinces and a federal district, the Autonomous City of Buenos Aires. The Argentine Republic can be grouped into 5 regions:Northwest, Northeast, Center, Cuyo and South (Figure 1). The geographic regions were integrated as follows in accordance with Argentina’s National Institute of Statistics and Census[7]: Northwest(JY: Jujuy, SA: Salta, CA: Catamarca, TUC: Tucumán, SE: Santiago del Estero and LR: La Rioja); Northeast (FO: Formosa, CH: Chaco,CR: Corrientes, MI: Misiones); Center (CB: Córdoba, SF: Santa Fe,ER: Entre Ríos, BA: Buenos Aires and Autonomous City of Buenos Aires); Cuyo (SJ: San Juan, MZ: Mendoza and SL: San Luis); and South (LP: La Pampa, NQ: Neuquén, RN: Río Negro, CT: Chubut,SC: Santa Cruz and TF: Tierra del Fuego).
2.2. Data collection
A retrospective study was conducted using data obtained from the Integrated Surveillance Bulletin database by the National System of Health Surveillance. Confirmed cases of cutaneous, mucocutaneous and visceral leishmaniasis up to the 52nd epidemiological week of each year in the period of 2013-2017 was collected. In the Argentine Republic, notification to the public health authorities has been compulsory since 1960 for more than 40 diseases (national law No.15 465), including leishmaniasis.
2.3. Data analysis
The geographical provinces of the Argentine Republic were implemented as units of analysis in order to evaluate the differences among them. The maps were generated in accordance with the total confirmed cases of cutaneous, mucocutaneous and visceral leishmaniasis collected between 2013 and 2017. The Arc-Gis version 10.2.1 GIS software (ESRI; Redlands, USA) was used. The administrative boundaries at country level were obtained from the SIG-250 of the National Geographic Institute (http://www.ign.gob.ar/sig250).
Reported cases of each clinical manifestation of leishmaniasis were graphed according to year using Graph Pad Prism version 5.0 software (La Jolla California, USA). In order to confirm if the northern regions are the areas with the highest prevalence,differences of leishmaniasis prevalence between the Northwest and Northeast towards the rest of the country were analyzed by prevalence ratio test. Confirmed leishmaniasis cases per year were analyzed by distribution Chi-square one-way test.
2.4. Ethical approval
Legal principles and ethical aspects were both considered and respected. This investigation was performed according to public domain data from the Argentine Republic Ministry of Health,without the possibility of identifying subjects, thereby dispensing the need for approval by an institutional review board for human research.
3. Results
In the period between 2013 and 2017, a total of 1 295 cases of confirmed leishmaniasis was reported in the Argentine Republic(Table 1). Among them, 1 128 (87.10%) cases corresponded to cutaneous leishmaniasis, with an annual average of 225.6 cases(ranging from 127 to 343). The highest number of notifications was recorded in 2015 (Pearson Chi-square test: χ2=128.93, df =4,P<0.000 1), with 343 cases (30.41%). Six hundred eighty (680) of the reported cutaneous leishmaniasis cases (60.28%) were from the Northwest; 400 (35.46%) from the Northeast; 43 (3.81%) from the Central region; four (0.35%) from the South and one (0.08%) from the Cuyo region (Figure 2 A).

Figure 1. Political and administrative division of the Argentine Republic into 5 regions. Northwest (JY: Jujuy, SA: Salta, CA: Catamarca, TUC: Tucumán,SE: Santiago del Estero and LR: La Rioja); Northeast (FO: Formosa, CH: Chaco, CR: Corrientes, MI: Misiones); Center (CB: Córdoba, SF: Santa Fe, ER:Entre Ríos, BA: Buenos Aires and CABA: Autonomous City of Buenos Aires); Cuyo (SJ: San Juan, MZ: Mendoza and SL: San Luis); and South (LP: La Pampa, NQ: Neuquén, RN: Río Negro, CT: Chubut, SC: Santa Cruz and TF: Tierra del Fuego).
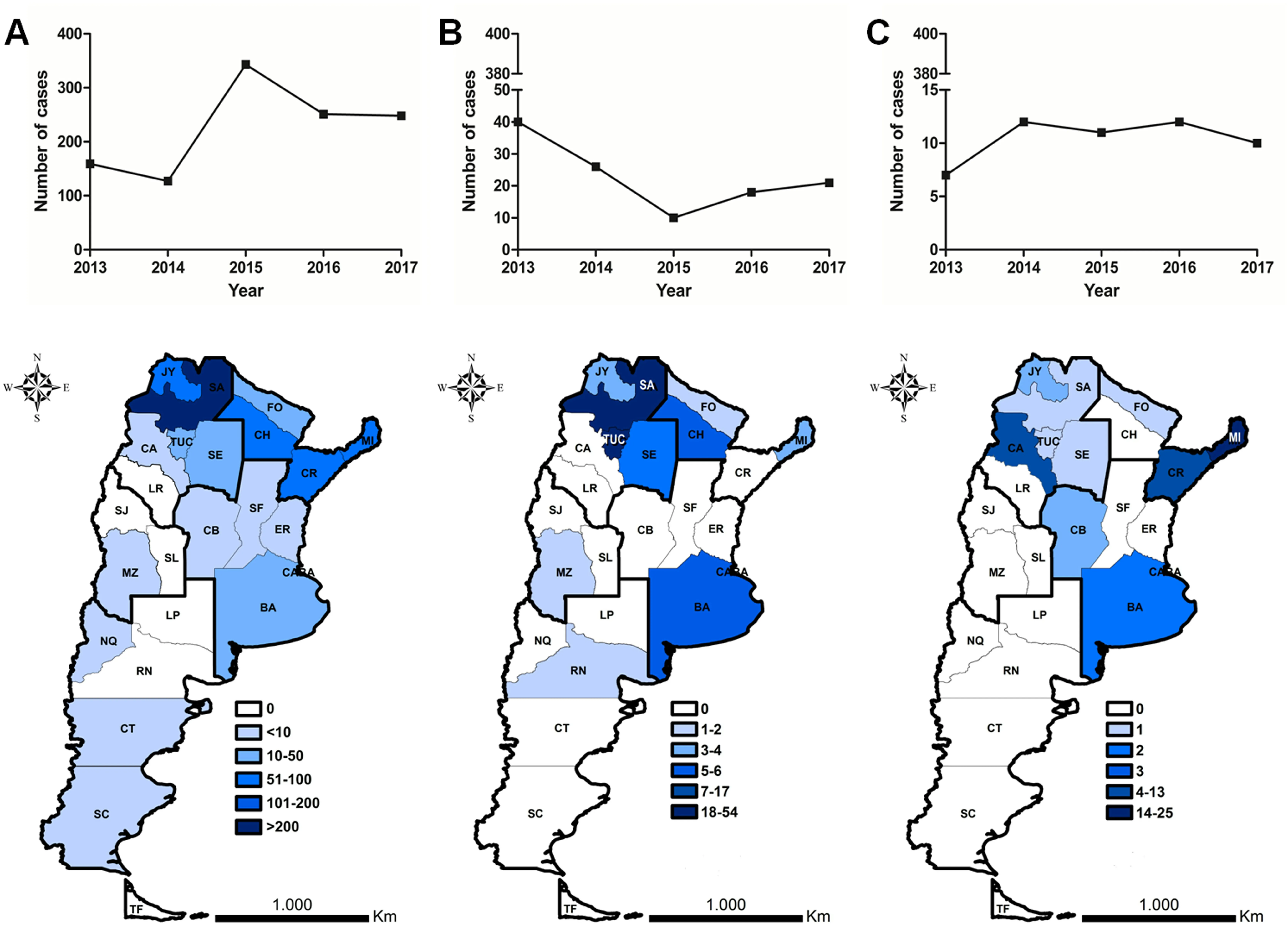
Figure 2. Temporal (above) and geographical (under) distribution of human leishmaniasis cases from 2013 to 2017. (A) cutaneous leishmaniasis, (B) mucocutaneous leishmaniasis, (C) visceral leishmaniasis. JY: Jujuy, SA: Salta, CA: Catamarca, TUC: Tucumán, SE: Santiago del Estero and LR: La Rioja, FO: Formosa, CH: Chaco,CR: Corrientes, MI: Misiones, CB: Córdoba, SF: Santa Fe, ER: Entre Ríos, BA: Buenos Aires and CABA: Autonomous City of Buenos Aires, SJ: San Juan, MZ:Mendoza and SL: San Luis, LP: La Pampa, NQ: Neuquén, RN: Río Negro, CT: Chubut, SC: Santa Cruz and TF: Tierra del Fuego.
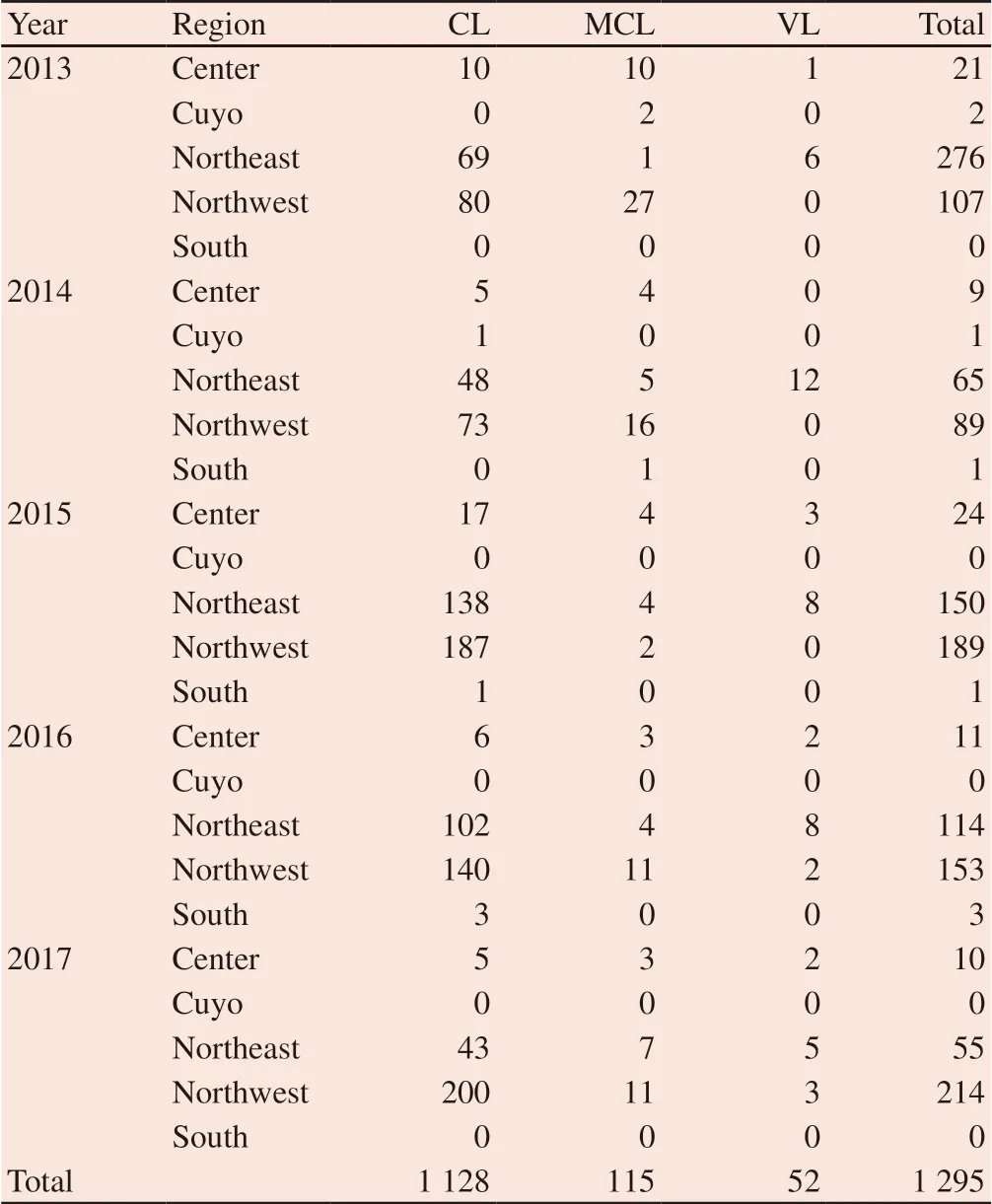
Table 1. Confirmed leishmaniasis cases per year and occurred regions.
Mucocutaneous leishmaniasis is the second most reported type of leishmaniasis in the Argentine Republic: 115 cases were reported(8.88%), with an annual average of 23 cases (ranging from 10 to 40).A pronounced decrease in the notification of new cases was recorded from 2013 to 2015. The highest notification of mucocutaneous leishmaniasis was recorded in the Northwest and Northeast regions of the country (Figure 2B).
A total of 52 cases (4.01%) with visceral leishmaniasis were identified with an annual average of 10.4 cases. Figure 2C shows the areas with the highest reported cases. Misiones Province, on the Northeast region of the country, is the most affected by this parasitic disease, totaling 25 human cases, followed by Corrientes Province,with 13 reported cases.
Statistically significant differences were found when prevalence of total leishmaniasis cases in the North was compared with prevalence in the rest of the country (Prevalence Ratio=53; Interval limits:l1=47.4, l2= 60.8, by test of prevalence ratio).
4. Discussion
In the Argentine Republic, as in the rest of the countries of the region, cutaneous leishmaniasis is the clinical form with the highest number of cases. Over the period studied, 87.10% of the patients reported suffered from cutaneous leishmaniasis. Researches made by the Pan American Health Organization/WHO show that this clinical presentation reached a peak in the year 2002 in the Argentine Republic, with 748 cases; whereas the period 2003-2011 registered an annual average of 235 diagnosed cases[8]. This annual average reported by the Pan American Health Organization/WHO is close to the annual average reported by our work for the period 2013-2017, with 225.6 cases, suggesting that cutaneous leishmaniasis prevalence is maintained over time in this region. Despite this, the notified confirmed cases of cutaneous leishmaniasis have recorded a significant increase (Pearson Chi-square test: χ2=128.93, df =4,P<0.000 1), which intensified in 2015.
In contrast to cutaneous leishmaniasis, a lower number of cases were reported for mucocutaneous leishmaniasis over this period,with 8.88% of the patients being recorded under this clinical presentation.
Studies carried out in Salta Province (Northwest of the Argentine Republic) over the period 2000-2014 show that out of 95 confirmed cases of leishmaniasis, 35.85% of which suffered from mucocutaneous leishmaniasis, showing a similar prevalence to cutaneous leishmaniasis[5]. Some discrepancies exist with previous studies also conducted in the Northwest region of the Argentine Republic, which indicate a higher frequency in cases of cutaneous leishmaniasis[9].
In addition, studies in this region also show a prevalence of cutaneous leishmaniasis over mucocutaneous leishmaniasis, with 10.5% cases of mucocutaneous leishmaniasis in Formosa between 1992 and 2001[10], and 10% cases of this type of leishmaniasis in Corrientes, Formosa and Chaco, diagnosed between 1988 and 2000[11].
The increase of commercial flow from 1970 favored the appearance of the endemic events of visceral leishmaniasis in the south of Brazil and Paraguay[12]. The first indigenous case of human visceral leishmaniasis in the Argentine Republic was reported in 2006 in Posadas city, Misiones Province, where L. infantum has been isolated from humans, dogs and sandfly vectors[13]. Posadas is a border city near Paraguay, which is considered as an endemic country[14]. This shows that dispersion occurs by geographical contiguity of human leishmaniasis due to social migrations and the spread of the vector from endemic areas. From May 2006 to July 2012, 103 cases of visceral leishmaniasis were confirmed, with an annual average of 14.7 cases[15], whereas in our period of study, an annual average of 10.4 cases was recorded. Misiones is the most affected province in the Argentine Republic, accounting for 25% of the reported cases in the period of study. The geographic spread of leishmaniasis transmission is limited by the distribution of the vector[15].
In the Argentine Republic, cutaneous and mucocutaneous leishmaniasis is endemic in the provinces of Salta, Jujuy, Tucumán,Catamarca, Santiago del Estero (Northwest region), Chaco,Formosa, Misiones and Corrientes (Northeast region). There is no report on geographical distribution of protozoa species belonging to Leishmania genus in Argentine Republic, which is a dynamic process because it is closely related to distribution of their vector,and it depends on deforestation, urbanization and other human activities[16].
In relation to the species that cause cutaneous and mucocutaneous leishmaniasis in Argentine Republic, L. braziliensis is the most frequent and with broad distribution in the country. It was isolated from patients with cutaneous and mucocutaneous clinical manifestation from Salta, Tucumán, Santiago del Estero, Corrientes,Misiones, Formosa and Jujuy provinces[5,10,17-21]. L. braziliensis was also isolated from vector [Lu. (Ev.) cortelezzii] in Chaco Province[22].There is no published data about Leishmania species that cause cutaneous or mucocutaneaous leishmaniasis in Catamarca, despite being considered as an endemic province, although Lu. (N.) neivai and Lu. (Ev.) cortelezzii, the main vectors of L. braziliensis, have been found in this area[23]. Additionally, Lu. (N.) neivai and Lu. (Mg.)migonei, species belonging to Phlebotominae family with vector capacity to L. braziliensis, have been found in Santa Fe and Entre Ríos provinces[24].
Moreover, L. amazonensis parasites have been isolated from patients with cutaneous and mucocutaneous leishmaniasis in Salta Province[5,9]. Finally, L. guyanensis has been identified as responsible agent of cutaneous leishmaniasis in patients from Salta and Corrientes provinces[25,26].
In the case of visceral leishmaniasis, it is spreading through autochthonous transmission outbreaks in the Argentine Republic.The transmission of human and canine visceral leishmaniasis has been reported in Misiones and Corrientes, while cases of human visceral leishmaniasis have been confirmed in Santiago del Estero and cases of visceral canine leishmaniasis have only been reported in Formosa. Nevertheless, the vector Lu. (Lu.) longipalpis is under active dispersion and it has been confirmed that it has already reached the south of Corrientes Province[27].
L. infantum, the etiological agent for visceral leishmaniasis,has been isolated from patients and vector [Lu. (Lu.) longipalpis]in Misiones Province[28] and from patients in Santiago del Estero[29] and Salta[30], where Lu. (Lu.) longipalpis has not been captured, so Lu. (Mg.) migonei is proposed as putative vector in these provinces[15]. Although the species responsible for visceral leishmaniasis in Corrientes have not been identified, the presence of Lu. (Lu.) longipalpis in this province could potentially be the cause of L. infantum infections[15]. Formosa, Chaco and Entre Ríos provinces could be vulnerable to leishmaniasis visceral infection due to the presence of the vector in this area[15,31,32].
Unfortunately, some of the leishmaniasis endemic provinces such as Santiago del Estero, Chaco, Corrientes and Formosa displayed the highest number of low income communities, which makes it more difficult to keep leishmaniasis controlled[33].
The number of cases of leishmaniasis in the Argentine Republic is suspected to be underreported. According to epidemiological studies carried out in the Northwest region of the country, during 1990 to 1993, the number of cases do not match with reports by National System of Health Surveillance, neither the results by capturerecapture method developed by the authors[34]. The underreported level of this disease could be due to the lack of awareness and health workers lack of interest in the epidemiological data collecting. This could explain the differences in confirmed cases of cutaneous and mucocutaneous leishmaniasis observed in 2015 in relation to other years.
The highest number of confirmed cases of leishmaniasis was found in the north regions of the Argentine Republic and this coincides with the endemic area of the country.
Deforestation for farming, the development of gated communities in the outskirts of the city, human migration coming from endemic areas and the tropicalization of continents, which is defined as a trend in the last few years toward increasing temperature and humidity in temperate areas[35]. They are factors that trigger changes in the dynamics of the vector’s dispersal, contributing to new establishments of the disease. For these reasons, provinces outside the endemic area of leishmaniasis have reported confirmed cases[36].This research assessed the epidemiological relevance of changes in leishmaniasis distribution in order to carry out targeted public health policies.
Conflict of interest statement
We declare that we have no conflict of interest.
Foundation project
This study was supported by grant from Fundación Alberto Roemmers (2017-2019).
 Asian Pacific Journal of Tropical Medicine2019年7期
Asian Pacific Journal of Tropical Medicine2019年7期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Disseminated cysticercosis presenting with bilateral proptosis: A case report
- Toxicological characterization and central nervous system effects of Calotropis procera Ait. aqueous extracts in mice
- Pouteria campechiana leaf extract and its bioactive compound myricitrin are mosquitocidal against Aedes aegypti and Culex quinquefasciatus
- Impact of seasonality on the prevalence and risk factors of Giardia lamblia infections among the aborigines
- Visceral leishmaniasis among children in an endemic area of northwestern Iran between 2016 and 2017: An epidemiological study
- Potential of herbal constituents as new natural leads against helminthiasis:A neglected tropical disease
