Stent placement followed by preoperative chemotherapy and elective surgery for acute malignant colorectal obstruction:Six cases of report
Jun-Jie Liu,Teng-Hui Ma,Qi-Yuan Qin,Lei Wang
Jun-Jie Liu,Teng-Hui Ma,Qi-Yuan Qin,Lei Wang,Department of Colorectal Surgery,the Sixth Affiliated Hospital of Sun Yat-sen University,Guangzhou 510655,Guangdong Province,China
Abstract
Key words: Stent;Colorectal cancer;Obstruction;Preoperative chemotherapy;Case report
INTRODUCTION
Acute malignant colorectal obstruction (AMCO) occurs in approximately 8.3% of colorectal cancers[1].Management of AMCO requires thorough assessment of patients,comprehensive understanding of the pathology and careful choice of treatment options.Since first introduced in 1994[2],stent placement has been widely used as a bridge to surgery for AMCO.Many randomized controlled trials and systematic reviews have demonstrated that stent placement followed by elective surgery is a safe and effective approach that has a lower stoma rate and reduced postoperative complications when compared with emergency surgery[3-9].
图书馆服务理念要突破传统图书馆在空间、时间、人员等方面的限制,为高校师生的教学科研服务、为师生的专业拓展服务。2015年7月,由美国新媒体联盟编写的,北京开放大学翻译的《新媒体联盟地平线报告(2015高等教育版)》指出:未来的几年内,正式学习和非正式学习融合,更多的移动学习和在线学习在高校广泛应用。现在已经有很多人通过互联网听到、看到、感受到在线教育的便捷。它因为具有名校名师效应、免费、高质量的优势,成为当下流行的课程选择。笔者认为,在线教育不仅仅是一种课程形式,它在本质上是互联网+知识的共享形态。图书馆在互联网+时代的服务应该与网络资源结合,更好地为师生利用网络提供高效、便捷的服务。
However,there are some concerns about the oncological safety of stent placement for AMCO.Recent studies have shown that stent use in AMCO resulted in higher local recurrence rate or inferior survival outcomes[10,11].In clinical practice,surgery of tumor resection was arranged about one week after stent placement.However,there are still some patients who cannot recovery well or obtain primary anastomosis without stoma creation in this short time.A recent meta-analysis indicated that the postoperative complication rate of using a stent as a bridge to surgery was up to 37.84%,and that the stoma rate was 28.8%[8].Adding preoperative chemotherapy into the prolonged interval between stent placement and elective surgery may reduce the risk of tumor dissemination and improve the general status of patients.In the current study,we presented six patients treated with two cycles of preoperative chemotherapy and elective surgery after stent placement and evaluated their outcomes.
CASES PRESENTATION
Chief complaints
From March 2016 to October 2017,six patients were hospitalized with the chief complaints of abdominal distention,abdominal pain and stop of flatus and defecation.
History of present illness
They had the chronic symptoms of colorectal cancers for at least two week,such as abdominal pain,change of the bowel habit and change of the stool character.The acute obstruction was occurred within 48 h before hospital admission.The signs of bowel perforation and strangulated obstruction were not found in these patients.
History of past illness
The six patients had Eastern Cooperative Oncology Group (ECOG) performance status ≥ 2 and adequate hematologic,liver and renal function.They had no other cancers or clinically significant cardiovascular diseases.
Physical examination
Abdominal distention and hyperactive bowel sounds were found.Peritoneal irritation signs were not found.
Laboratory testing
The blood routine index,biochemical function and tumor biomarker were tested after hospitalization.The initial testing results of hemoglobin,albumin and creatinine were shown in Table 1.
Imaging examination
Bowel distention with gas and effusion was shown in abdominal X-ray.Computed tomography (CT) showed that the obstructing tumor was located on left-sided colon or upper rectum (more than 10 cm from the anal verge).Obvious distention of proximal bowel was also found in CT scan.The tumor stage was examined through enhanced CT scanning.
FINAL DIAGNOSIS
The basic characteristics of the six patients are shown in Table 1.Six patients were diagnosed with AMCO.There was one patient with descending cancer,four with sigmoid cancers and one with rectal cancer.Two patients had synchronous hepatic metastasis.One patient had two metastastic sites in the left lobe of liver (maximum diameter:1.6 cm and 5.8 cm),and the other patient had one metastatic site in S8(maximum diameter:2.2 cm).
TREATMENT
Stent placement
Before stent placement,an endoscopic biopsy was carried out to confirm the malignancy diagnosis.An endoscope was used to cross the stricture caused by the tumor.When the stricture could not be crossed,a guide wire in a catheter was used.Contrast agent was injected through the catheter to estimate the length and width of the stricture.An appropriately sized of self-expandable metal stent (SEMS) was chosen according to the estimation of the stricture.The stent delivery system was pushed into the area of the stricture with radio-endoscopic guidance.The stent was deployed to crossover the distal and proximal end of the stricture.The passing of fecal material through the stent indicated successful placement.If complications from the stent occurred,including re-obstruction,migration of the stent or bowel perforation,patients were sent to emergency surgery.
Preoperative chemotherapy
After stent placement,the six patients were scheduled for preoperative chemotherapy,which consisted of two cycles of modified infusional fluorouracil,leucovorin and oxaliplatin [modified FOLFOX6 (mFOLFOX6)],instead of direct surgery.The timing of preoperative chemotherapy after stent placement was determined by the time when the obstructive symptoms disappeared.Each cycle consisted of oxaliplatin 85 mg/m2,leucovorin 400 mg/m2and fluorouracil 400 mg/m2given intravenously on day 1 and fluorouracil 2400 mg/m2given over 48-h of continuously intravenous infusion on days 1-2.Acute adverse events associated with chemotherapy were graded according to the Common Terminology Criteria Adverse Events Version 4.03.
Elective surgery
Surgery of primary tumor resection was performed two to three weeks after the end of chemotherapy.Mechanical bowel preparation was used preoperatively.Laparoscopic or open surgery was performed by senior surgeons.Complete mesocolic or mesorectal excision with central vascular ligation was adopted as the standard technique.Stoma creation or colonic lavage was selectively performed in the cases with obvious bowel edema or distention,or doubtful anastomosis.
Postoperative treatment
The patient with one metastatic site in S8 underwent microwave ablation.The patient with two hepatic metastatic tumors in left liver lobe underwent partial hepatectomy,but he refused postoperative chemotherapy.The other five patients received postoperative chemotherapy for three to six months.
OUTCOME AND FOLLOW UP
The obstructive symptoms of these six patients were disappeared within 3 d afterstent placement.No patients had complications caused by stents.The median time between stent placement and preoperative chemotherapy was 9 d (range,3-34).None of the grade 3/4 toxicities were found.The median time between stent placement and elective surgery was 38 d (range,33-43).All of the six patients underwent primary tumor resections with primary anastomosis.No patient had stoma creation,colonic lavage or postoperative complication.Five patients (83.3%) received laparoscopic surgery.The median operation time was 162.5 min (range,112-270).The median blood loss was 50 mL (range,30-100).The median lymph node harvest was 26 (range,13-45).The median time to first flatus was 2 d (range,2-4).The median postoperative stay was 11.5 d (range,9-17).The perioperative outcomes are shown in Table 2.
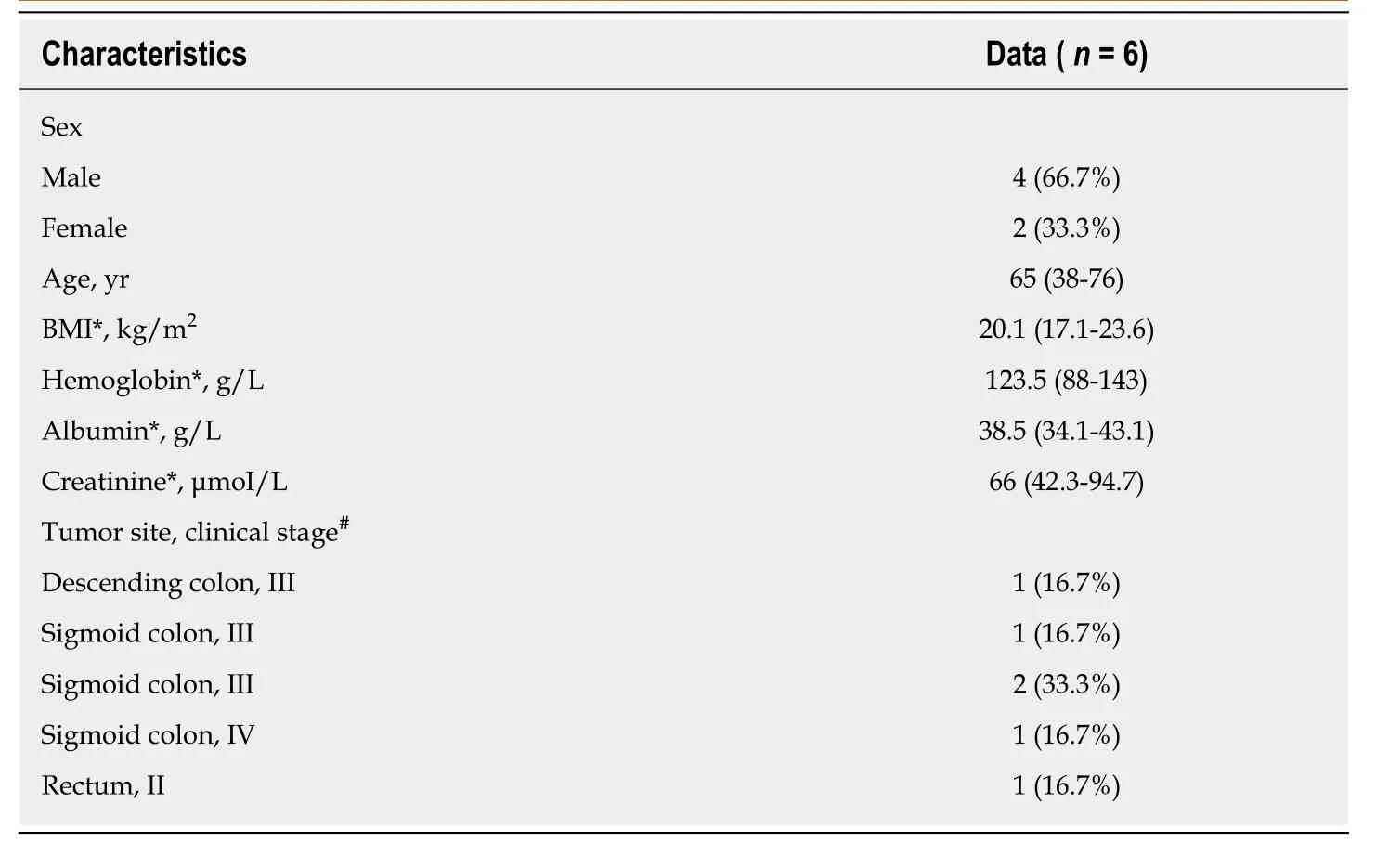
Table1 Patient characteristics
Eighteen months after surgery of primary tumor resection was set for the follow-up period.Two patients were found with peritoneal metastasis at the end of follow-up period (both of them received postoperative chemotherapy).
DISCUSSION
The use of SEMS as a bridge to surgery for AMCO has been an increasingly common practice in qualified medical centers.In the present study,we introduced the clinical use of preoperative chemotherapy and elective resection after stent placement for AMCO.The case series showed that this new approach provided no stoma creation and no morbidity.
The original intention of adding preoperative chemotherapy after stent placement was to lighten the potential adverse effect of stent placement.Maruthachalamet al[12]found that insertion of a stent resulted in increased levels of CK20 mRNA in the peripheral blood of patients with colorectal cancer,which was considered to promote the distribution of occult tumor cells.Fryeret al[13]analyzed the histopathological changes induced by stent placement in 72 patients and concluded that the changes of the tumor included tumor necrosis (100%) and flat ulceration (77.8%).Colonic perforation caused by the stent may potentially result in the peritoneal seeding[14].In a retrospective study of Korea,a higher rate of perineural invasion was observed in patients of the stent group compared to surgery group (76%vs51.4%,respectively)[15].Sabbaghet al[11]first reported significantly lower overall survival for the patients with stent placement after conducting a propensity score analysis.Although receiving preoperative and postoperative chemotherapy,two patients in our study were found with peritoneal metastasis at the end of follow-up period.It demonstrates that the evidence about the inferior oncological outcomes of stent placement may be underestimated in our clinical practice.
Most obstructing colorectal cancers are in the advanced stage.For the metastatic colorectal cancers that are suitable for curative resection,it is appropriate to carry out preoperative chemotherapy in order to reduce the tumor load.In terms of tumorswithout macroscopic metastasis,preoperative chemotherapy was considered to eradicate micrometastasis and to reduce the risk of incomplete excision.Preoperative chemotherapy in locally advanced rectal cancer has been recommended by clinical guidelines.For locally advanced and operable colon cancers,preoperative chemotherapy is feasible with encouraging pathological responses,although longterm outcomes are unknown[16].
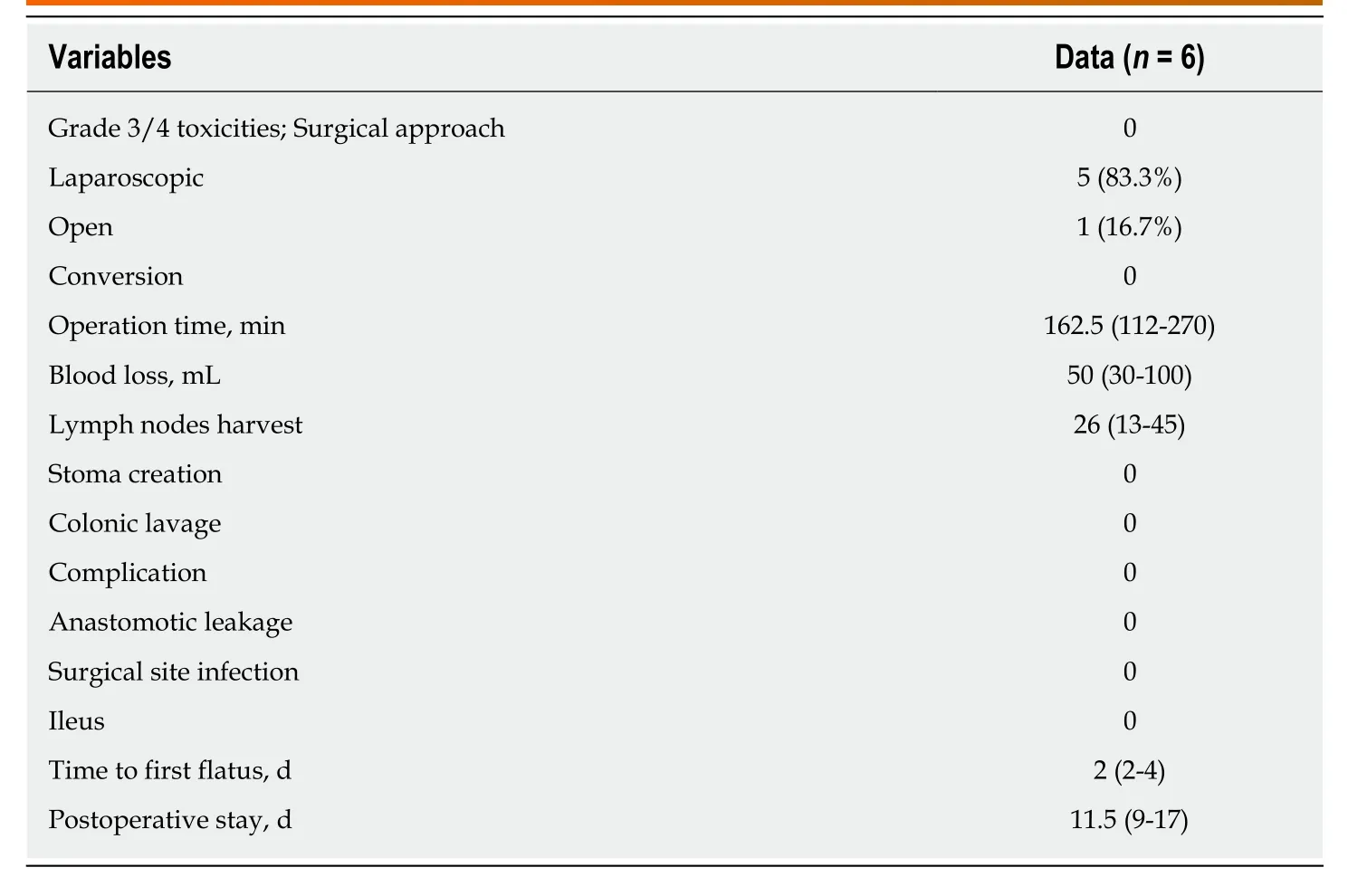
Table2 Perioperative outcomes
The optimal time interval between stent placement and subsequent surgery has not been clearly mentioned by previous studies.Five to ten days was recommended by the guidelines of the European Society of Digestive Endoscopy[17].A meta-analysis showed a median interval of ten days from stent placement to surgery[9].A retrospective study from Turkey concluded that time intervals of seven to nine days after stent placement is sufficient for safe surgery[18].However,extending the time interval will lead to better recovery of bowel and nutritional status.The six cases showed that primary anastomosis without stoma creation was obtained after the interval of four weeks.In our experiences,a time interval of ten days is not enough for the bowel to restore.We considered that the better bowel environment could be obtained at least four weeks after stent placement.However,a prolonged interval may increase the technical difficulty of surgery because of more local tumor infiltration and fibrosis in patients with stents.In addition,more cycles of chemotherapy during stent placement might induce more complications such as bowel reobstruction,stent migration and bowel perforation.In our study,the two cycles of preoperative chemotherapy have excellent clinical outcomes and patient compliance.However,it needs further studies to confirm.
CONCLUSION
The study demonstrates that the placement of SEMS followed by two-cycle preoperative chemotherapy and elective surgery is a safe and feasible strategy for the treatment of AMCO.This new strategy brings no stoma creation and low postoperative morbidity.Surgeons can apply this method to selected patients after thorough evaluations and multidisciplinary collaborations.However,the oncological improvement of this strategy and the optimal cycles of preoperative chemotherapy need confirmation in further studies,in particular clinical trials.
 World Journal of Gastrointestinal Oncology2019年3期
World Journal of Gastrointestinal Oncology2019年3期
- World Journal of Gastrointestinal Oncology的其它文章
- Near-infrared fluorescence guided esophageal reconstructive surgery:A systematic review
- Hepatic resection vs percutaneous radiofrequency ablation of hepatocellular carcinoma abutting right diaphragm
- Post-operative computed tomography scan-reliable tool for quality assessment of complete mesocolic excision
- Human colorectal cancer cells frequently express IgG and display unique Ig repertoire
- Glycerophospholipids pathways and chromosomal instability in gastric cancer:Global lipidomics analysis
