Rhombencephalitis caused by Listeria monocytogenes with hydrocephalus and intracranial hemorrhage:A case report and review of the literature
Jing-Jing Liang,Xiao-Yan He,Hong Ye
Abstract
Key words: Rhombencephalitis;Listeria monocytogenes;Central nervous system infections;Hydrocephalus;Intracranial hemorrhage;Case report
INTRODUCTION
Listeria monocytogenes(L.monocytogenes)is one of the very few bacteria that can infect neurons to produce a serious and often fatal disease,with a mortality of 20%-50%[1-4].L.monocytogenesinfection occurs predominantly in the following populations:elderly people,pregnant women,newborns,and immunodeficient patients;patients with chronic liver disease,malignant hemopathies,and diabetes;patients on chronic hemodialysis;and,less frequently,healthy individuals[5,6].The main routes of transmission are confirmed to be through the consumption of contaminated food andviavertical transmission from mother to child[7].Penetration of the intestinal,bloodbrain,blood-choroid,and fetoplacental barriers is one of the most important virulence factors ofL.monocytogenes[8].Therefore,the manifestations of listeriosis are varied,such as gastroenteritis,septicemia,meningitis,and other conditions.
Neurolisteriosis,a central nervous system(CNS)infection caused byL.monocytogenes,represents 5%-10% of listeriosis cases and is less common in the world,especially rhombencephalitis[9-11].Hydrocephalus and intracranial hemorrhage are rare complications of listeriosis,occurring in 10%-15% and 3% of neurolisteriosis cases,respectively[12,13].In this paper,we present a young patient withL.monocytogenesrhombencephalitis who presented with persistent alteration of consciousness,hydrocephalus,and intracranial hemorrhage.This case is rare due to the occurrence of hydrocephalus and intracranial hemorrhage.Cases published between 1985 and 2018 that are related toListeriahydrocephalus are reviewed in Tables 1 and 2.
CASE PRESENTATION
Chief complaints
A 29-year-old Chinese man was admitted to the hospital with a 2-d history of intermittent fevers of up to 39 °C,and forehead headache without nausea.
History of present illness
Two days prior to onset,he had consumed unpasteurized cooked beef that was stored in the refrigerator for a few days.
History of past illness
His medical history included type 2 diabetes mellitus,which was poorly controlled,fatty liver,smoking,and drinking.
Personal and family history
He denied a family history of hypertension and stroke.
Physical examination upon admission
The physical examination was unremarkable,except for nuchal rigidity.
Laboratory examinations
The blood laboratory findings showed that glucose,C-reactive protein,and erythrocyte sedimentation rate were high,while white blood cells(WBCs),red blood cells,hemoglobin,urea,creatinine,serum minerals,and autoimmune antibodies were normal.The first lumbar puncture on admission revealed a turbid cerebrospinal fluid(CSF)with 2090 leukocytes/mm3(30% neutrophils,70% monocytes),233.85 mg/dL protein,1.4 mmol/L glucose(serum glucose 9 mmol/L),and pressure > 33 cmH2O.CSF Gram stain showed Gram-positive rods and was negative for fungi and acid-fast bacilli(Table3).On the 8thday,the blood cultures yieldedL.monocytogenes,which was susceptible to ampicillin,erythrocin,meropenem,and penicillin but resistant to sulfamethoxazole.CSF and urine cultures were negative.Repeated CSF examination on the 14thand 28thday showed a greater decrease in WBCs and protein(Table3).
Imaging examinations
The initial brain CT was unremarkable,and chest CT showed bilateral bronchopneumonia.On the 4thday of admission,magnetic resonance imaging(MRI)of the brain showed an abnormally high T2 flow attenuated inversion recovery(FLAIR)signal in the right pons and prominent temporal horns with enlargement of the ventricles(Figure 1).On the 14thday,brain CT showed hemorrhage of the right pons and hydrocephalus(bilateral lateral ventricular and the third ventricle hydrocephalus)(Figure 2).The 3rdcerebral CT was performed on the day after extraventricular drainage,revealed significant dilatation of fourth ventricle,and no remission in lateral ventricles(Figure 3).The 4thbrain CT on the 29thday showed rehaemorrhagia of the lateral ventricle and a larger ventricular system(Figure 4).
FINAL DIAGNOSIS
The patient was finally diagnosed withListeriarhombencephalitis,hydrocephalus,and intracranial hemorrhage.
TREATMENT
Although empiric antibiotic therapy for bacterial meningitis(Ceftriaxone 2 g,every 12 h for 2 d,followed by meropenem 1 g,every 8 h for 2 d)and all other supportive symptomatic treatments were administered after performing blood cultures,the patient developed new symptoms with fever,sinus tachycardia,tachypnea,confusion[Glasgow Coma Scale(GCS)score 12/15],bilateral horizontal nystagmus,bilateral abducens nerve palsy,dysarthria,and weakness of all four limbs.He was transferred to the intensive care unit(ICU)on the 5thday.On the 8thday,he went into coma(GCS score 5/15),and was intubated and ventilated without autonomous respiration.According to blood cultures,new antibiotic therapy with ampicillin,etimicin andmeropenem was administered.On the 12thday,etimicin was discontinued as he became afebrile.We performed an extraventricular drainage to relieve hydrocephalus on the 22ndday(Figure 3).On the 29thday,because of rehaemorrhagia of the lateral ventricle,his condition rapidly deteriorated(GCS score 3/15),with anisocoria(left pupil 4 mm and right pupil 2 mm).

Table2 Characteristics of 18 cases of non-perinatal listeriosis with hydrocephalus published between 1989 and 2018
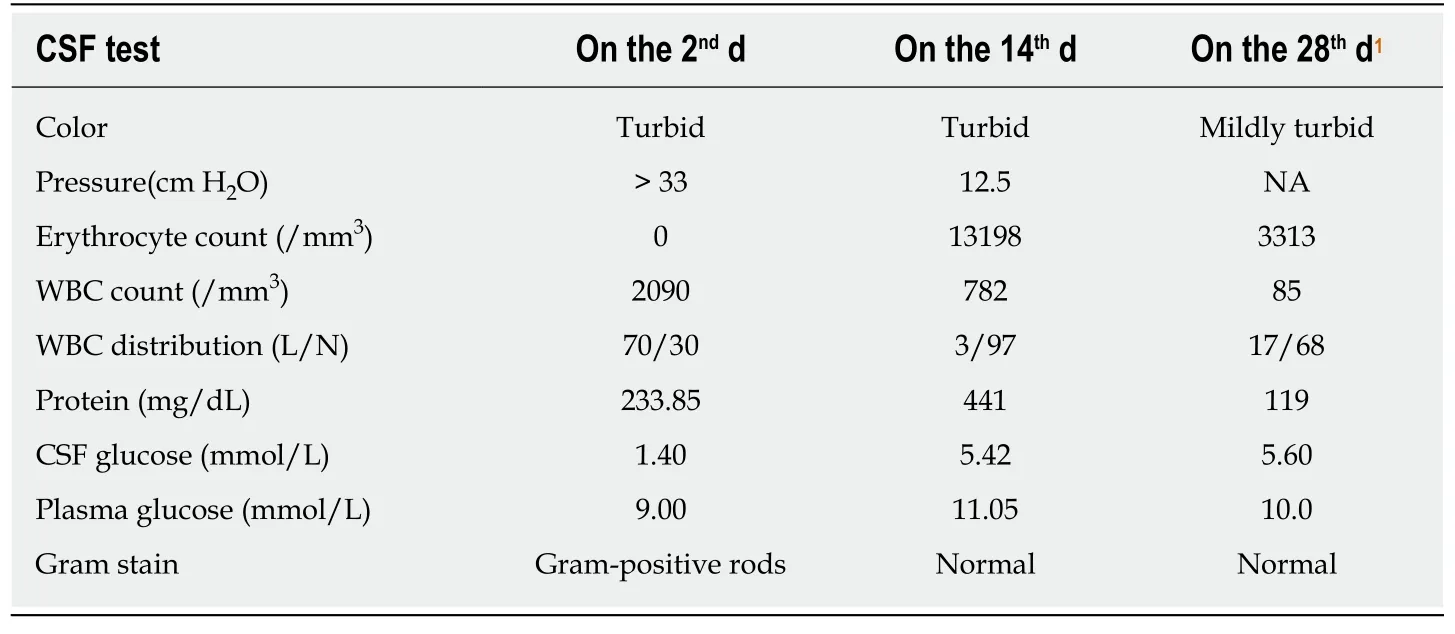
Table3 Cerebrospinal fluid analysis across disease duration
OUTCOME AND FOLLOW-UP
The patient died on the 31stday.Autopsy could not be performed.
DISCUSSION
AlthoughL.monocytogeneshas been reported to be the third most common cause of community-acquired bacterial meningitis,following pneumococcal and meningococcal meningitis in adults,its occurrence is relatively rare,accounting for only 5% of encephalitis cases in metropolitan France[14].Listeriahas an important impact on public health,with high hospitalization and mortality rates despite antibiotic treatment[15].As listeriosis is not incorporated into the national monitoring system for cases,epidemiological data onListeriaare scarce in China[7,16].In a study published in 2013,Fenget al[16]reviewed 147 cases of listeriosis in China from 1964 to 2010,with neurolisteriosis accounting for 31% of cases.The overall case-fatality rate was 26%,highest among neonatal cases(46%)and lowest among pregnant cases(4%)[16].In a study conducted by Wanget al[7],38 cases of listeriosis,including 5 neonatal,8 maternal,and 25 nonmaternal cases,were reviewed in China between 1999 and 2011,and the case-fatality rates for neonatal,maternal,and nonmaternal cases were 20%,0%,and 26%,respectively[7].
CSF and blood cultures are the most specific for diagnosis.Early diagnosis of neurolisteriosis is difficult not only because the presentation of CSF is similar to the manifestations of other bacterial encephalitis and meningitis(pleocytosis,hyperproteinorrachia,and hypoglycorrhachia)but also because approximately 50% of CSF Gram stains are negative[17].Jubeltet al[18]reported that approximately threequarters of patients have CSF pleocytosis,with approximately equal percentages of mononuclear and polymorphonuclear cells.In our case,there was an initial predominance of lymphocytic cells,which then turned to mononuclear cell predominance;this change might be related to pathological processes and the application of antibiotics.Listeriais usually revealed first on blood cultures,which are positive in 62% of encephalitis cases[19].Therefore,early before antibiotic administration,repeated blood and CSF cultures are necessary and helpful for early and differential diagnoses.
L.monocytogenesinfection most frequently presents as acute bacterial meningitis,less commonly as meningoencephalitis,and least commonly as rhombencephalitis,accounting for approximately 10% of neurolisteriosis cases[12,13].Although the exact mechanism of rhombencephalitis remains poorly understood,L.monocytogeneshas a well-known predilection for the brainstem.Karlssonet al[9]reviewed 120 patients withListeriarhombencephalitis and suggested thatL.monocytogenesenters the cerebellopontine angle through the trigeminal nerve in a subset of patients,invading the brainstemviathe sensory trigeminal nuclei.As MRI is superior to CT in detecting subtentorial abnormal lesions,it has become more helpful for diagnosing rhombencephalitis,which has a high signal on T2-FLAIR sequences.
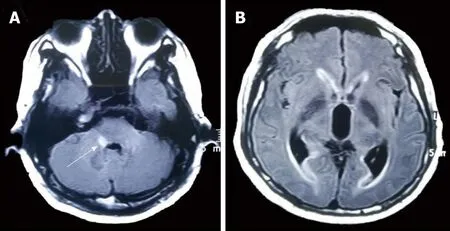
Figure1 Axial brian T2-FLAIR magnetic resonance imaging shows a hyperintense lesion of the right pons(A,white arrow),and prominent temporal horns with enlargement of ventricles(B)on the 4th d of administration.
L.monocytogenescomplications,such as acute hydrocephalus,hemorrhage,brain abscess,spine abscess,cerebritis,and ventriculitis,can develop,and the mortality associated with these complications is significantly high.Hydrocephalus is most common in tuberculous encephalitis but rare in listeriosis,with an approximate 3%incidence ofL.monocytogenesmeningoencephalitis in adults[13].The exact mechanism of hydrocephalus remains unclear.The development of meningitis-associated hydrocephalus may be due to several mechanisms,such as a high level of CSF protein,impaired CSF absorption due to the obliteration of the subarachnoid space by meningeal exudates,and/or blockade of the CSF pathway by leptomeningeal inflammation[20].
Retrospective analysis of hydrocephalus due to listeriosis is scarce at present,and most of the literature consists of case reports.The time to onset of hydrocephalus varies greatly,ranging from 1 d to 9 wk[20,21].Ventricular drainage may not be an effective way to relieve hydrocephalus and improve survival[12,14].A study from the Netherlands reviewed 26 hydrocephalus cases in 577 bacterial meningitis patients(4.5%),including four cases ofL.monocytogenes(15%),all of whom underwent placement of an external ventricular drain catheter[14].None of these patients improved clinically after catheter placement,and all had poor outcomes for hydrocephalus,with three deaths(75%)and one case of serious sequela(25%),thus indicating that patients with hydrocephalus were at a high risk for unfavorable outcomes and that hydrocephalus was an independent risk factor for death[14].In our case,the patient underwent ventricular drainage,but a continuous improvement in cognitive function was not obvious.
Another rare complication ofListeriameningitis is intracranial hemorrhage,which is also one of the determinants of unfavorable outcomes[2].Most reported cases of intracranial hemorrhage occur in infants and young children,while the condition is quite rare in adults.Svareaet al[22]reported a case of maternal listeriosis resulting in preterm delivery and intraventricular hemorrhage,which was diagnosed by an ultrasound scan.In a prospective study of 860 episodes with bacterial meningitis in the Netherlands,24(2.79%)were diagnosed with intracranial hemorrhage,withS.pneumoniaeaccounting for 67% andL.monocytogenesaccounting for 4%[2].The underlying pathophysiology of intraventricular hemorrhage inL.monocytogenesinfection is still unknown and may be related to dysregulation of both the coagulation and fibrinolytic pathways and to vascular endothelial cell swelling and activation[2].
An empirical therapy for bacterial meningitis,generally third-generation cephalosporins,is always applied at an early stage when bacterial meningitis is suspected.However,this treatment option does not coverL.monocytogenes.Former publications have demonstrated that inappropriate empirical antibiotic therapy leads to unfavorable outcomes[23].Therefore,it is very important to adjust the appropriate antibiotic therapy as soon as possible onceListeriais highly suspected or confirmed.
Listeriais known to be difficult to treat,not only becauseL.monocytogeneshas an intracellular life cycle but also because only a few antibiotics demonstrate activity againstListeria[24].Due to the lack of multicenter clinical controlled studies,the optimal antibiotic regimen and duration for neurolisteriosis have not been definitively defined.However,amoxicillin,ampicillin,and penicillin G are generally considered effective regimens in the treatment of listeriosis[24].The addition of aminoglycosides(such as gentamicin)could be considered a treatment regimen forL.monocytogenesmeningitis,but its use remains controversial due to the occurrence of kidney damage[24].The drugs should be applied at high doses,and the duration of this treatment should be extended to 21 d or longer,until complete eradication,to prevent relapse[24].Furthermore,cotrimoxazole,rifampin,meropenem,linezolid,tetracyclines,and moxifloxacin should also be considered active againstListeria[23].In our patient,the combination of ampicillin,etimicin,and meropenem was used forListeria,and it was proven effective by repeated CSF examinations(Table3).
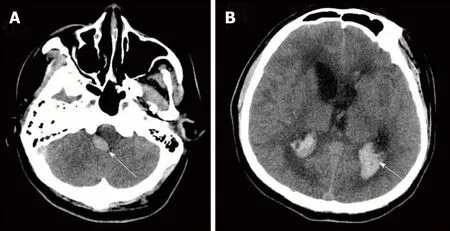
Figure2 Axial brain computed tomography shows hemorrhage of the right pons(A,white arrow),and gross hydrocephalus and hemorrhage(B,white arrow)on the 14th d of administration.
CONCLUSION
We report a case of acute hydrocephalus and intracranial hemorrhage due to complications fromL.monocytogenesrhombencephalitis.The pathogenesis of complications has been reviewed.L.monocytogenesmay be prone to entering the brainstem through the trigeminal nerve;hydrocephalus may be close with a high level of CSF protein and impaired CSF absorption and circulation;the occurrence of intracranial hemorrhage may be related to dysregulation of both the coagulation and fibrinolytic pathways and to vascular endothelial cell swelling and activation.Hydrocephalus,intracranial hemorrhage,and inappropriate antimicrobial treatment are the determinations of unfavorable outcomes.

Figure3 Axial brain computed tomography shows no improvement of hydrocephalus in the lateral ventricle on the 22nd d of administration(A and B).

Figure4 Axial brain computed tomography shows rehaemorrhagia of the lateral ventricle and a larger ventricular system(A and B)on the 29th d of administration.
 World Journal of Clinical Cases2019年4期
World Journal of Clinical Cases2019年4期
- World Journal of Clinical Cases的其它文章
- Anterior cervical corpectomy decompression and fusion for cervical kyphosis in a girl with Ehlers-Danlos syndrome:A case report
- Primary hepatic leiomyosarcoma successfully treated by transcatheter arterial chemoembolization:A case report
- Long-term follow-up of a patient with venlafaxine-induced diurnal bruxism treated with an occlusal splint:A case report
- Hydrochloric acid enhanced radiofrequency ablation for treatment of large hepatocellular carcinoma in the caudate lobe:Report of three cases
- Therapeutic plasma exchange and continuous renal replacement therapy for severe hyperthyroidism and multi-organ failure:A case report
- Recurrent acute liver failure associated with novel SCYL1 mutation:A case report
