Primary hepatic leiomyosarcoma successfully treated by transcatheter arterial chemoembolization:A case report
Ke-Lei Zhu,Xiu-Jun Cai
Abstract
Key words: Treatment;Prognosis;Transcatheter arterial chemoembolization;Primary hepatic leiomyosarcoma;Case report
INTRODUCTION
Primary hepatic leiomyosarcoma is rare and only reported sporadically[1],with less than 40 cases having been reported to date.It appears to be associated with acquired immune deficiency syndrome(commonly known as AIDS)[2],Epstein-Barr virus[3],Hodgkin's lymphoma[4],immunosuppression after organ transplantation[5],and hepatitis C virus(commonly known as HCV)-related liver cirrhosis[6],the precise mechanisms leading to leiomyosarcoma have yet been fully identified.Surgical resection is recommended for a curative treatment,while diagnosis of primary hepatic leiomyosarcoma is challenging and often delayed until it reaches a size that results in dismal prognosis.
We herein describe the first case of primary hepatic leiomyosarcoma successfully treated by transcatheter arterial chemoembolization(TACE).The patient has survived for 82 mo with no tumor enlargement and distant metastasis detected at postoperative follow-up.
CASE PRESENTATION
Chief complaints
A 68-year-old woman was referred to our hospital on December 2011,due to right upper quadrant pain and a 5-pound weight loss.
Personal and family history
Other symptoms were not presented and she did not drink alcohol,smoke or have a history of surgery.
Physical examination upon admission
Physical examination revealed a soft abdomen,no tenderness,no rebound tenderness,and no palpable lymph nodes or abdominal mass.
Laboratory examinations
The following laboratory data were recorded:hemoglobin of 125 g/L;white cell count of 5.5 × 109/L,with 72.5% neutrophils;platelet count of 234 × 109L;alanine aminotransferase of 25 U/L;serum total protein of 75 g/L;albumin of 37.2 g/L;total bilirubin of 11 μmol/L;direct bilirubin of 9.5 μmol/L;α-fetoprotein of 5.23 ng/mL;and carcinoembryonic antigen of 4.5 ng/L.Serological markers for hepatitis B virus and HCV were negative.The indocyanine green retention rate at 15 min was 2.2%.
Imaging examinations
Abdominal ultrasonography showed there was a mixed echoic mass measuring around 10 cm × 7 cm in the right hepatic lobe.Abdominal computed tomography(CT)showed a similar finding,that the tumor was inhomogeneous density,with mild delayed enhancement,and had central necrosis(Figure 1A).Gastrointestinal endoscopy and colonoscopy showed negative findings.Chest CT showed no mass over the lung.
Preoperative diagnosis was unconfirmed,exploratory laparotomy was performed 1 wk after admission,and no obvious effusion was found in the abdominal cavity.The entire liver VIII was occupied by a creamy white,firm mass measuring about 10 cm ×7 cm,which protruded into the abdominal cavity and appeared to invade the diaphragm and middle hepatic vein ,making the tumor unresectable(Figure 1);thus,a biopsy was performed.Rapid frozen-section biopsy analysis considered the diagnosis of leiomyosarcoma.Histopathological examination showed a hepatic mass that consisted of spindle-shaped cells with mitotic figures and nuclear atypia(Figure 2).Immunohistochemical staining showed that spindle-shaped cells were positive for anti-smooth muscle actin(Figure 3)and desmin(Figure 4)but negative for keratin,S-100,CD34 and CD117.No obvious lesions were observed in the bilateral adnexa and uterus,and no palpable mass was detected in the superficial body.
FINAL DIAGNOSIS
Taken together,a final diagnosis of primary hepatic leiomyosarcoma was established.
TREATMENT
TACE was performed 2 wk postoperatively.Superior mesenteric angiography showed no significant abnormality.Common hepatic angiography demonstrated a single mass with hypervascularity,tumor staining and dilated feeding arteries in the anterior segment of the right liver lobe(Figure 1B).A catheter was inserted into the feeding artery of the tumor,and the emulsion containing 50 mg epirubicin and Lipiodol(Lipiodol Ultra-Fluid;Guerbet Japan,Tokyo,Japan)was injected,followed by embolization with gelatin sponge particles(Gelpart;Nihonkayaku,Tokyo,Japan).The postoperative course was uneventful and the patient was discharged on day 7 after the operation.The patient underwent three courses of TACE,and the latest treatment was performed in October 2016.There were no newly emerging lesions observed in the liver(Figure 5B).
OUTCOME AND FOLLOW-UP
Routine follow-up was continued in the hepatobiliary clinic.Contrast-enhanced CT in 2018 showed that the tumor had shrunk significantly and was associated with satisfactory lipiodol deposition(Figure 5A).The patient was followed up for 82 mo until now,and no progressive enlargement of the tumor or distal metastasis was observed.
DISCUSSION
Primary hepatic leiomyosarcoma is extremely rare,and less than 40 such cases have been reported in the English-language literature.Primary hepatic sarcoma comprises only 1%-2% of all malignant hepatic tumors[7],and leiomyosarcoma is particularly rare.Hepatic leiomyosarcoma may arise from intrahepatic vascular structures[8],bile ducts[9]or ligamentum teres[10],and is reported to be associated with AIDS[2],Epstein-Barr virus[3],Hodgkin's lymphoma[3],immunosuppression after organ transplantation[4],and HCV-related liver cirrhosis[5].However,the precise steps leading to leiomyosarcoma have not been fully identified.
Leiomyosarcoma has no specific clinical manifestations.It is often asymptomatic until it becomes large and produces nonspecific symptoms,or is unexpectedly found during physical examination.Some patients may have a wide spectrum of symptoms,including abdominal pain,abdominal mass,weight loss,nausea,vomiting,anorexia,abdominal distension,jaundice,and,rarely,acute intra-abdominal bleeding secondary to tumor rupture.
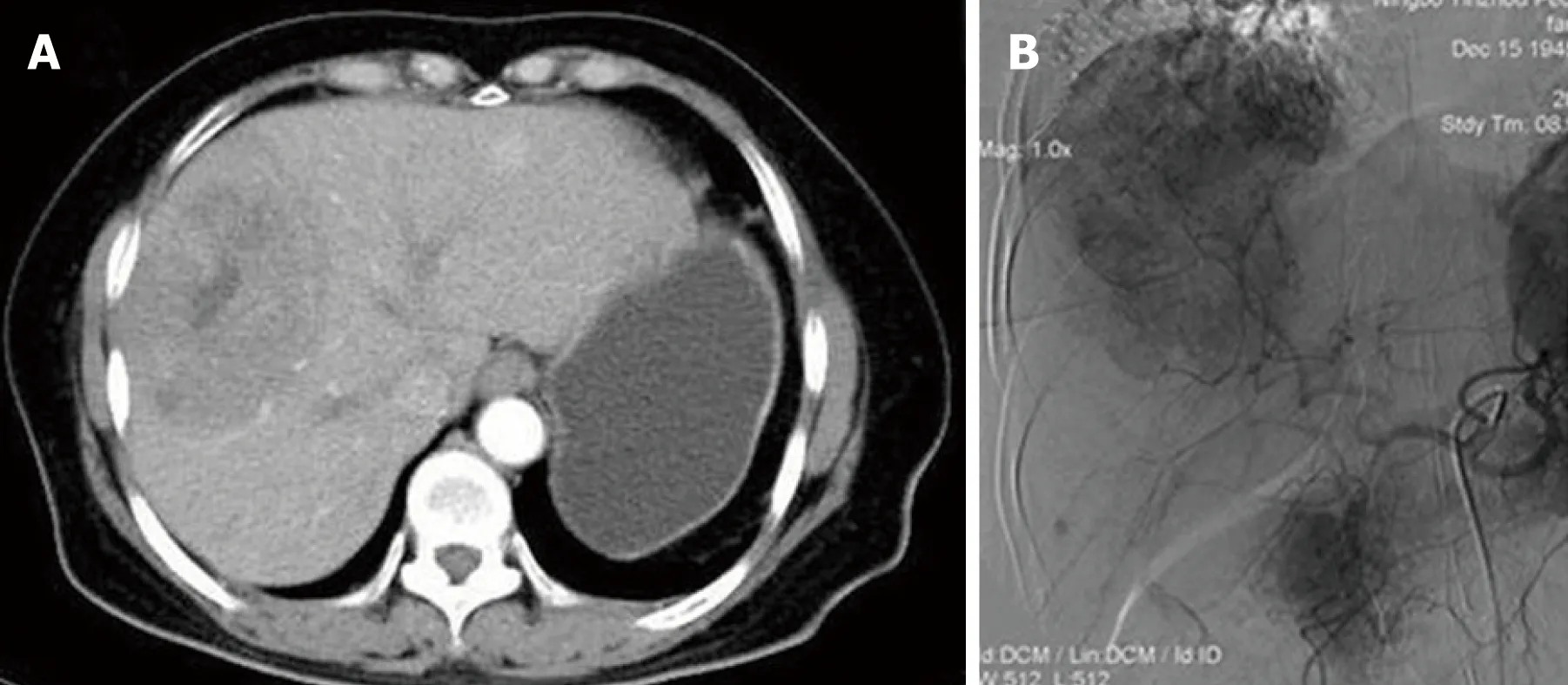
Figure1 Imagining features before treatment.
CT findings of primary hepatic leiomyosarcoma have been described as an enlarged,heterogeneous,hypodense mass with peripheral enhancement and evidence of central necrosis,whereas magnetic resonance imaging usually displays the homogeneous or heterogeneous hypointensity tumor on T1-weighted images and hyperintensity on T2-weighted images.Diagnosis of primary hepatic leiomyosarcoma is challenging due to the nonspecific nature of symptoms and lack of serological markers.The clinical manifestations and laboratory and imaging examinations have limited value for diagnosis and differential diagnosis.The definitive diagnosis of leiomyosarcoma mainly depends on pathological and immunohistochemical examinations.The pathological features of leiomyosarcoma include spindle-shaped cells,abundant cytoplasm,nuclear atypia,and presence of mitotic figures.Immunohistochemical staining of tumors is positive for vimentin,desmin and actin,and negative for α-fetoprotein,CD34,CD117,cytokeratin,and hepatocytes.
Surgical resection is considered to be the only potentially curative treatment.Patients with primary hepatic leiomyosarcoma mostly have no history of hepatitis B and cirrhosis.Therefore,complete resection of the tumor,such as regular hepatic lobectomy,hemihepatectomy and trisegmentectomy,may achieve a satisfactory therapeutic outcome.Matthaeiet al[11]reported three cases with > 10 yr survival after hepatectomy.Liver transplantation for primary hepatic leiomyosarcoma has remained controversial until now.The outcome for liver transplantation has varied among cases.Lianget al[12]described a patient with primary hepatic leiomyosarcoma who survived for 34 mo after undergoing liver transplantation.In contrast,Saintpaulet al[13]reported a case with only 15 d survival after surgery.The efficacy of chemotherapy and radiotherapy for primary hepatic leiomyosarcoma has not been confirmed.Adjuvant chemotherapy using doxorubicin and ifosfamide seems to slow progression and help to prolong survival after complete resection[14].
Currently,no effective treatments for unresectable primary hepatic leiomyosarcoma have been reported.Fujitaet al[5]reported a patient with metastatic leiomyosarcoma who just received palliative and conservative therapy and only survived for 3 mo after diagnosis.For our case,the patient underwent three courses of TACE with emulsion of epirubicin and Lipiodol,followed by embolization with gelatin sponge particles.Postoperative contrast-enhanced CT showed significant tumor shrinkage associated with satisfactory lipiodol deposition.Routine follow-up was continued in the hepatobiliary clinic and there were no newly emerging lesions observed in the liver.The case has been followed up for 82 mo until now,and no progressive enlargement of the tumor or distal metastasis has been observed.Primary hepatic leiomyosarcoma is a tumor with rich blood supply,and tumor cells are intolerant to ischemia.The embolic agents injected into the hepatic artery induced ischemic tumor necrosis.This may be the main mechanism underlying the effectiveness of drug-eluting bead TACE(commonly known as DEB-TACE).Otherwise,the epirubicin was used to suppress tumor progression[15].
CONCLUSION
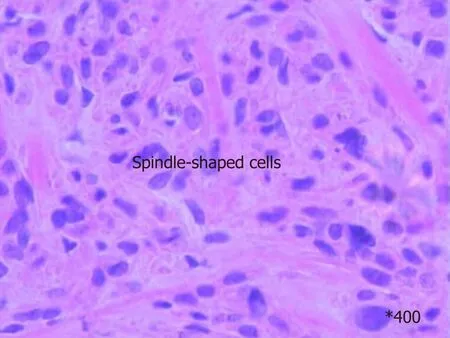
Figure2 Histological examination showed a hepatic mass that consisted of spindle-shaped cells with mitotic figures and nuclear atypia.
We have described the first case of primary hepatic leiomyosarcoma successfully treated by TACE,and demonstrated that TACE is safe and effective.Further studies are required to assess the therapeutic effect of TACE in combination with surgical resection in primary hepatic leiomyosarcoma.

Figure3 Immunohistochemical staining was positive for anti-smooth muscle actin.
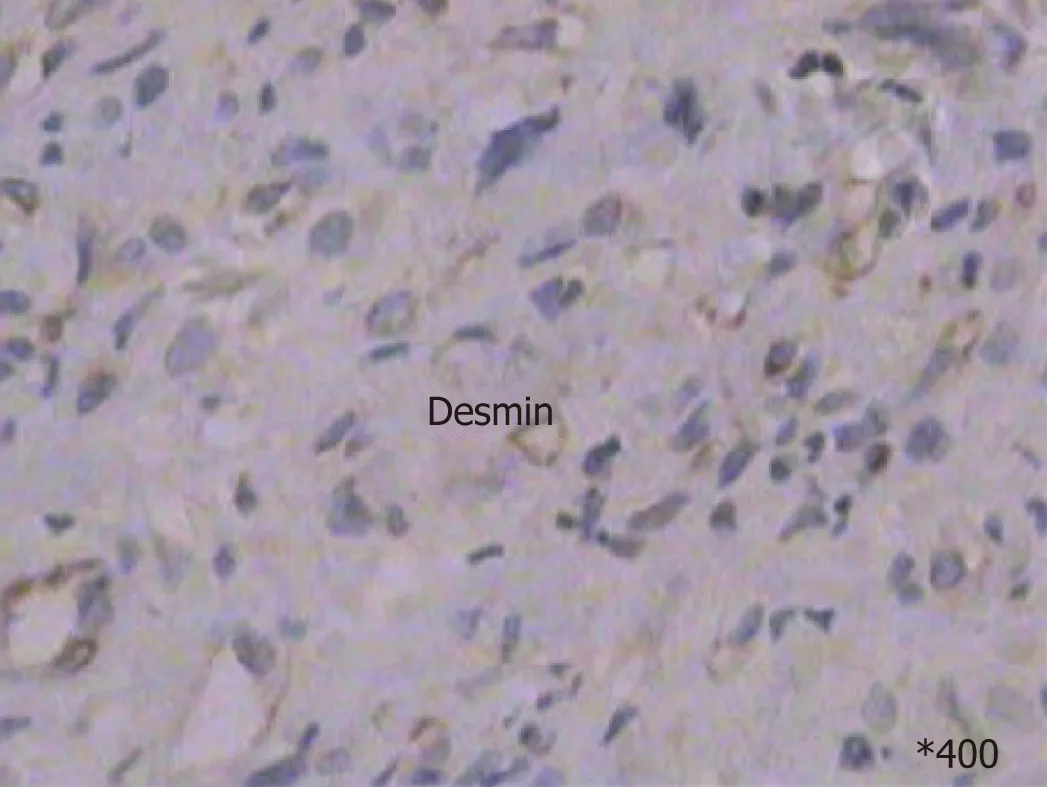
Figure4 Immunohistochemical staining was positive for desmin.
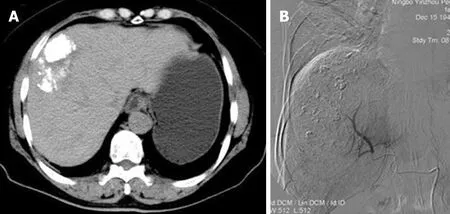
Figure5 Imagining changes after treatment.
 World Journal of Clinical Cases2019年4期
World Journal of Clinical Cases2019年4期
- World Journal of Clinical Cases的其它文章
- Immune checkpoint inhibitor-induced colitis:A comprehensive review
- Formalin fixation on HER-2 and PD-L1 expression in gastric cancer:A pilot analysis using the same surgical specimens with different fixation times
- Nested case-control study of multiple serological indexes and Brighton pediatric early warming score in predicting death of children with sepsis
- Intestinal endometriosis:Diagnostic ambiguities and surgical outcomes
- Efficacy of 1.2 L polyethylene glycol plus ascorbic acid for bowel preparations
- Congenital analbuminemia in a patient affected by hypercholesterolemia:A case report
