Perioperative rh-endostatin with chemotherapy improves the survival of conventional osteosarcoma patients: a prospective non-randomized controlled study
Hairong Xu, Zhen Huang, Yuan Li, Qing Zhang, Lin Hao, Xiaohui Niu
Department of Orthopedic Oncology Surgery, Beijing Ji Shui Tan Hospital, Peking University, Beijing 100035, China
ABSTRACT Objective:Anti-angiogenic drugs are an emerging treatment option against malignant tumors. The aim of this study was to determine whether the addition of perioperative rh-endostatin to chemotherapy could improve the probability of distant metastasis-free survival (DMFS) and overall survival (OS) in patients newly diagnosed with non-metastatic conventional osteosarcoma.Methods:This was a controlled non-randomized clinical study that included 388 patients without clinically detectable metastatic disease enrolled from January 2008 to April 2012. The control treatment group had 272 patients; 180 were male and 92, female,with a median age of 17 years. The treatment group had 58 patients; 36 were male and 22, female, with a median age of 16 years.The control group received preoperative chemotherapy followed by surgery and postoperative chemotherapy. The treatment group received 4 cycles of rh-endostatin perioperatively in addition to chemotherapy as per the control group. Patients were followed up from 6-101 months with a median follow-up period of 50.2 months.Results:The 5-year DMFS of the control group (61%) was significantly lower than that of the rh-endostatin group (79%)(P = 0.013). The 5-year OS of the control group (74%) was significantly lower than that of the rh-endostatin treatment group(87%) (P = 0.029). No difference in adverse drug reactions was found between these 2 groups.Conclusions:The addition of perioperative rh-endostatin to chemotherapy could significantly improve the DMFS and OS of patients with non-metastatic osteosarcoma.
KEYWORDS Osteosarcoma; rh-endostatin; perioperative; distant metastasis; overall survival
Introduction
Conventional osteosarcoma is the most common malignant bone tumor in children and adolescents. Long-term survival of localized osteosarcoma has increased substantially from 10%-20% in the 1970s, when surgery was the sole treatment,up to 50%-70% in the 1980s and onwards1,2. The most common survival predictors are the presence of metastases and the histological response to preoperative chemotherapy3,4. The value of chemotherapy for the treatment of osteosarcoma is well established. The most frequently used agents against osteosarcoma include doxorubicin, cisplatin, high-dose methotrexate (HDMTX)and ifosfamide5.
Recombinant human endostatin (rh-endostatin)(EndostarTM), expressed and purified in Escherichia coli with an additional 9-amino acid sequence forming another his-tag structure, was approved by the State Food and Drug Administration of China in 2005 for the treatment of nonsmall cell lung cancer6,7. Since anti-angiogenic drugs are directed against developing vasculature, not tumor cells, they may stabilize tumor load, rather than produce partial or complete remission. Moreover, the discontinuation of antiangiogenic therapy may allow a tumor to resume growth.Thus, anti-angiogenic treatment alone is not suitable for patients with malignant tumors. In preclinical studies,synergistic antitumor efficacy was observed in an osteosarcoma nude mouse model with the addition of rhendostatin to doxorubicin8.
From January 2008 to April 2012 our hospital carried out a single-institution study. This was a prospective, nonrandomized, controlled, doctor-initiated clinical study in patients newly diagnosed with non-metastatic conventional osteosarcoma. The primary endpoint of this study was to evaluate whether the addition of rh-endostatin to doxorubicin, cisplatin, HDMTX, and ifosfamide chemotherapy would improve overall survival (OS). The secondary endpoints included whether the addition of rhendostatin would improve distant metastasis-free survival(DMFS) and event-free survival (EFS).
Materials and methods
Patients
All enrolled patients had histologically newly diagnosed conventional osteosarcoma (pathologically high-grade).Patients had no clinically detectable metastatic disease(Enneking stage IIB9) and received no prior treatment before enrollment. Patients had to be between 6 and 65 years of age without any contraindications to chemotherapy, including those associated with peripheral blood: white blood cells≥ 3.0 × 109/L, platelets ≥ 75 × 109/L, and hemoglobin level≥ 95 g/L; liver function: blood bilirubin level ≤ 2.5 × normal upper limit and transaminase level ≤ 2.5 × normal upper limit; and renal function: serum creatinine level ≤ 2.0 ×normal upper limit and blood urea nitrogen level ≤ 2.5 ×normal upper limit. Patients were required to have a normal electrocardiogram and no untreatable cardiovascular disease or cerebrovascular disorders and should not be pregnant.Approval for this study was obtained from the institutional review board before patient enrollment. Informed consent was obtained from all patients or their guardians.
Treatments
There were 2 treatment arms, the control group(doxorubicin, cisplatin, HDMTX, and ifosfamide) and the rh-endostatin group (doxorubicin, cisplatin, HDMTX,ifosfamide, and rh-endostatin). Both treatment regimens were explained in detail to patients or their guardians. It was the patient's/guardians' final decision to enroll in either the control group or the rh-endostatin group. The informed consent form was completed and signed by the patient or their legal representative before the commencement of the treatment.
Both regimens called for an initial period of chemotherapy, designated as induction therapy, that lasted about 2 months, followed by definitive resection of the primary tumor. Maintenance chemotherapy was scheduled to begin 2 weeks after the surgery but did not begin until the surgeons had determined that the surgical wound was healing adequately. However, if the initial surgical plan was amputation of the affected limb the patients received no induction therapy.
The sequence of 1 cycle of chemotherapy was HDMTX,followed by ifosfamide, doxorubicin, cisplatin, and a repeated dose of HDMTX. HDMTX (10 g/m2) was administered as a 4-hour infusion followed by leucovorin rescue. Serum methotrexate levels and renal function were monitored daily and every 3 days, respectively. Hydration and alkalinization with leucovorin were specified in the event of delayed methotrexate excretion. Ifosfamide (15 g/m2) was administered with mesna protection for 5 days. Doxorubicin was administered at a dose of 90 mg/m2for 3 consecutive days, and cisplatin was administered during the first day of doxorubicin delivery at a dose of 120 mg/m2. One cycle of induction chemotherapy lasted about 2 months, and 4 cycles of maintenance chemotherapy lasted about 8 months.
Rh-endostatin was administered at a dose of 15 mg for 14 consecutive days. Subsequently, the patients had a 7-day break followed by the repeated administration of rhendostatin. We specified that the administration of rhendostatin would be separated from the administration of methotrexate, ifosfamide, doxorubicin, and cisplatin by a minimum of 2 hours. Rh-endostatin was administered as a 4-6 hours infusion for a total of 4 cycles along with both induction and maintenance chemotherapy.
Definitive surgery was performed at week 9 for limbsalvage patients and at week 1 for amputation patients.Surgery was administered with curative intent and achieved a wide or marginal margin in all cases.
Endpoints and statistical analysis
The primary endpoint was OS, defined as the time from study entry until death or last patient contact. Patients without events were censored at the date of last contact. The secondary endpoints included DMFS, EFS, and toxicity.DMFS was defined as the time from study entry until distant metastasis or last patient contact, whichever came first. EFS was defined as the time from study entry until an adverse event or last patient contact, whichever came first. Adverse events included disease progression, the diagnosis of a second malignant neoplasm, or death before disease progression.Disease progression included local recurrence and distant metastasis. Patients without adverse events were censored at the date of last contact. Toxicity was monitored using World Health Organization common toxicity criteria10, with special attention to hepatotoxicity and nephrotoxicity. We compared the incidence of grades III and IV adverse events for the 2 groups. OS, DMFS, and EFS were estimated using the Kaplan-Meier method. The possible risks of each factor were summarized using hazard ratios (HRs) from multivariate Cox regression models. HRs were expressed relative to patients in the baseline category of the factor of interest. An HR < 1.0 and > 1.0 indicate a lower and higher risk, respectively, of the event for patients in that category compared with the baseline category. The survival curves were drawn using Prism 7 Software. The statistical significance of the comparisons of risk for adverse events was assessed by means of the log-rank test.
The sample size was estimated as follows. Using a power of 80% and an alpha of 0.05, the 5-year survival for the control group was approximately 60%, and that of the test group was expected to be 80%. The ratio of the test group and control group was about 1:4. The total sample size was estimated to be 250 cases. However, due to the possibility that not all cases will meet the eligibility criteria and some would be lost to follow-up, the final number of cases was estimated to be 350-380.
Results
Patient characteristics
A total of 388 patients were enrolled. Among the 310 patients enrolled in the control group, 38 did not meet the eligibility criteria. Among the 78 patients enrolled in the rh-endostatin group, 20 did not meet the eligibility criteria. Finally, 330 patients were included in this study. Among them, 272 were in the control group, and 58 were in the rh-endostatin group at a ratio of 4.7:1. The control group contained 180 men and 92 women with a median age of 17 years. In the rhendostatin group, there were 36 men and 22 women with a median age of 16 years. Follow-up ranged from 6-111 months with a mean period of 56 months. There was no statistical difference in sex, age, location of the tumor, tumor volume11,surgical margin9, or surgery between the 2 groups (Table 1).
Local recurrence and distant metastasis
There were 26 local recurrences in the control group with a recurrence rate of 9.6% (26/272). In the rh-endostatin group,there were 3 local recurrences with a recurrence rate of 5.2%(3/58). The number of local recurrences was not significantly different between the 2 groups (P = 0.284).
In the control group, 94 patients developed distant metastasis, including 74 lung metastases alone, 10 bone metastases alone, 7 bone and lung metastases, 1 lung and brain metastases, and 2 lung and abdominal metastases. Thedistant metastasis rate for the control group was 34.6%(94/272). In the rh-endostatin group, 12 patients developed distant metastases, including 9 lung metastases alone, 1 bone metastasis alone, and 2 bone and lung metastases. The distant metastasis rate for the rh-endostatin group was 20.7%(12/58). There was a significant difference regarding the number of distant metastases between the 2 groups (P =0.04).
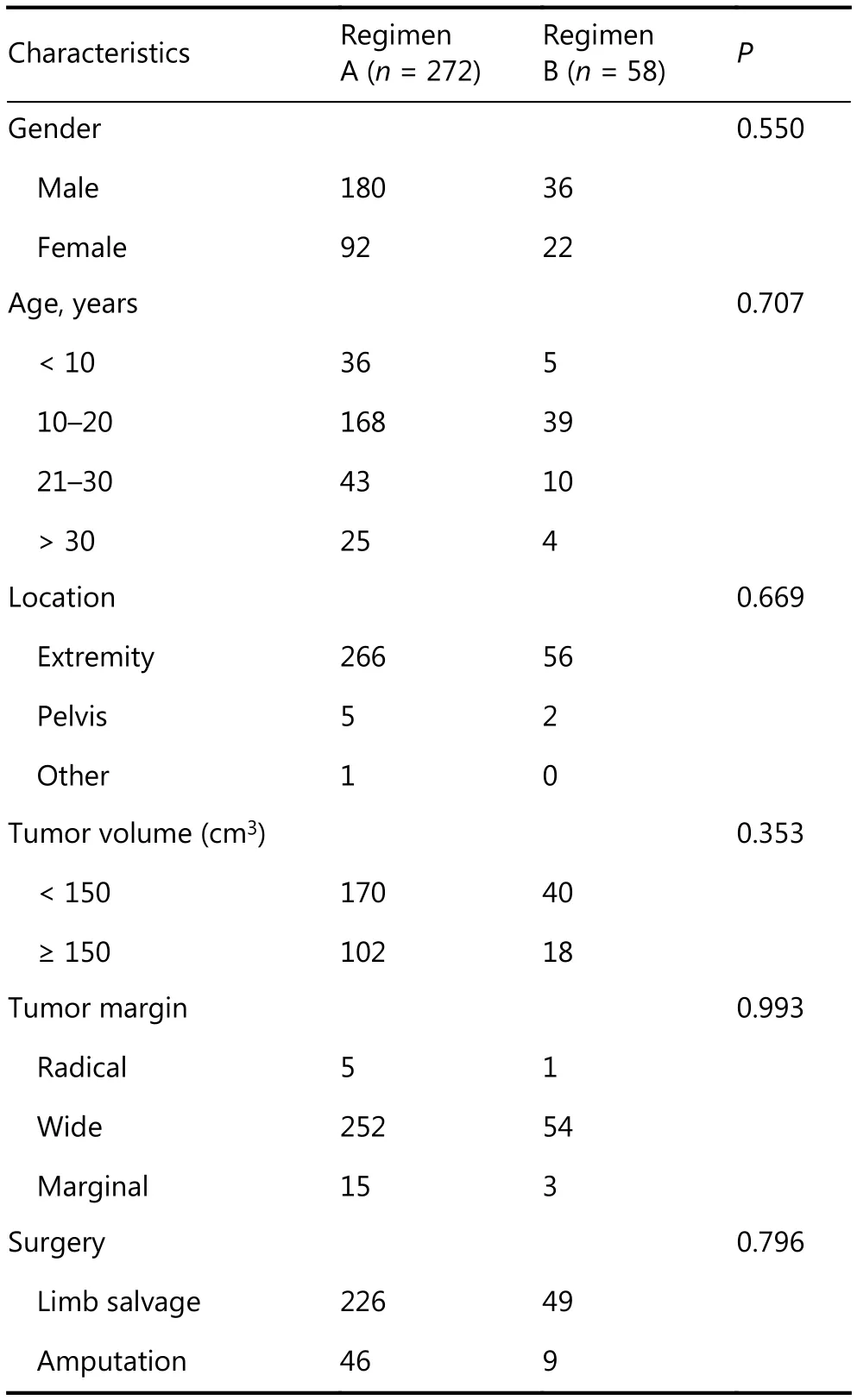
Table 1 The patient characteristics of the two groups
Distant metastasis-free survival
In the control group, the 2-year and 5-year DMFS rates were 71% and 61%, respectively. In the rh-endostatin group, the 2-year and 5-year DMFS rates were 82% and 79%,respectively. The 2 groups were significantly different regarding their DMFS rates (P = 0.013, log rank) (Figure 1).The relative risk of distant metastasis for patients who had received rh-endostatin was 0.478 [95% confidence interval(CI), 0.300-0.761, P = 0.014]
Event-free survival
In the control group, the 2-year and 5-year EFS rates were 67% and 57%, respectively. In the rh-endostatin group, the 2-year and 5-year EFS rates were 81% and 75%, respectively.There was a statistically significant difference between the 2 groups (P = 0.010, log rank) (Figure 2). The relative risk of events for patients who had received rh-endostatin was 0.490(95% CI, 0.364-0.873, P = 0.010).
Overall survival
In the control group, the 2-year and 5-year OS rates were 85% and 74%, respectively. In the rh-endostatin group, the 2-year and 5-year OS rates were 96% and 87%, respectively.There was a statistically significant difference between the 2 groups (P = 0.029, log rank) (Figure 3). Multivariate analyses for OS are shown in Table 2. Surgery methods (limb salvage vs. amputation) and treatment arms (with/without rh-endostatin) were both prognostic for OS. The relative risk of death for patients who underwent amputation was 2.24 (95% CI, 1.16-4.33, P = 0.006), and for patients who had received rh-endostatin, it was 0.37 (95% CI, 0.16-0.87,P = 0.016).
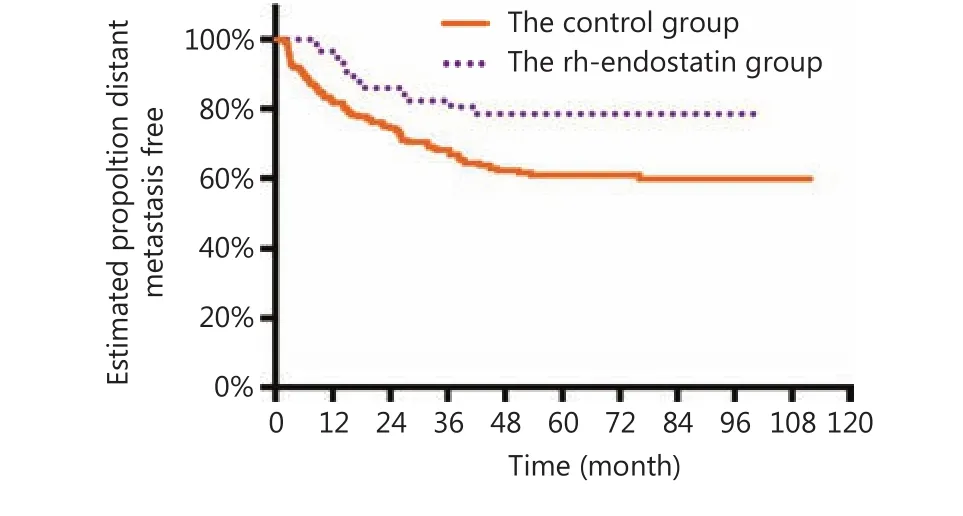
Figure 1 Distant metastasis-free survival for patients according to the treatment arms.
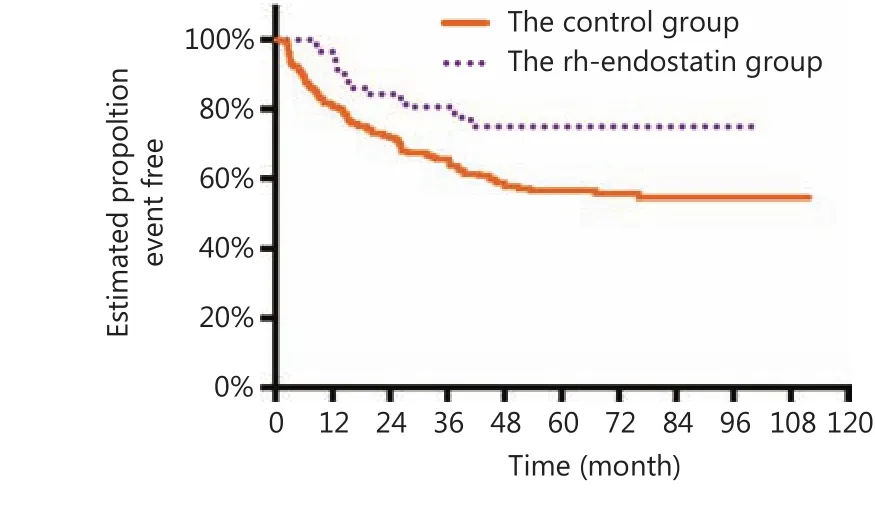
Figure 2 Event-free survival for patients according to the treatment arms.
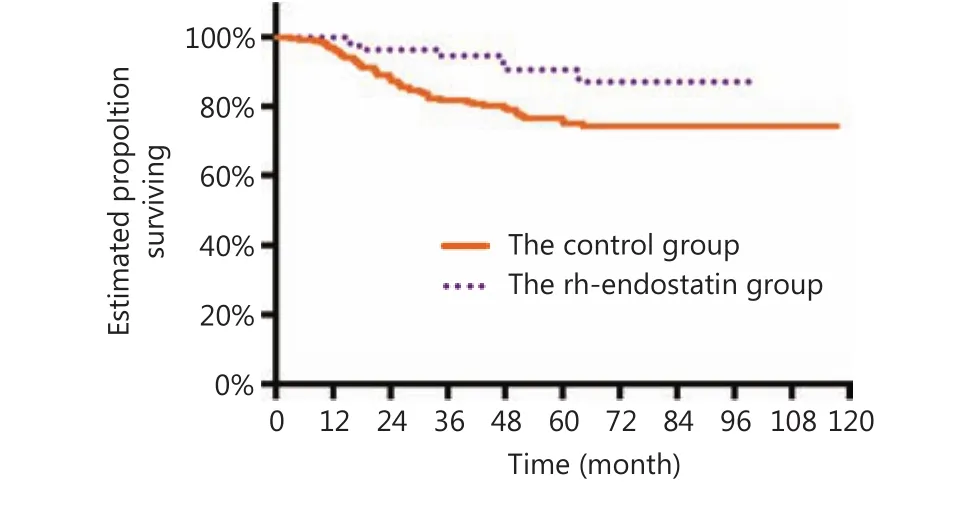
Figure 3 Overall survival for patients according to the treatment arms.
Toxicity of therapy
Toxicity was reported for all the patients in this study. There was no treatment-related death in either group. The most common grade III and IV adverse reactions in the control and rh-endostatin groups were leukopenia, lowered hemoglobin level, hepatic impairment, nausea, and vomiting(Table 3). No adverse cardiac toxicity was observed, and no delayed wound healing was observed in either group. There was no significant difference in adverse effects between the 2 groups. No cases of discontinuation of treatment due to adverse drug reactions were observed.
Discussion
Although osteosarcoma is the most common primary malignant bone tumor, its treatment is still one of the most challenging issues in bone tumor therapy and even the entire field of oncology12,13. High-dose chemotherapy using methotrexate and doxorubicin has greatly increased the OS rate of osteosarcoma since the 1970s14,15. Over the past 30 years, oncologists have tested numerous approaches to improve the OS of osteosarcoma patients, including increasing the intensity of chemotherapy, using various combinations of chemotherapeutic agents, and even incorporating immunotherapy. However, to date, no new treatments have significantly reduced the development of lung metastases, which currently occur in up to 30%-50% of osteosarcoma patients16,17. Therefore, the key to improve the survival rate of osteosarcoma is reducing the incidence of lung metastases.
In 1971, Dr. Folkman proposed the theory of tumor angiogenesis18. He pointed out that both local tumor growth and distant metastases are dependent on tumor angiogenesis.Subsequently, anti-angiogenesis became a new field of cancertreatment. Anti-angiogenesis therapy-related research has shown that there exists a balance in the body's proangiogenic factors and angiogenesis. However, when the primary tumor is excised, the pro-angiogenic factors dominate, thus, contributing to the formation of distant metastases19. In osteosarcoma patients, a study found that the balance of systemic angiogenic factor activity and angiogenesis inhibitory factor activity was disrupted, which was associated with the occurrence of postoperative lung metastasis20. Dutour's research demonstrated that therapy using Endo cDNA/CLP is associated with a pronounced delay in tumor growth in a human-like rat orthotopic tumor model21. Endo cDNA/CLP could effectively prevent the occurrence of lung metastases in osteosarcoma. We have previously undertaken promising anti-angiogenesis research on osteosarcoma in both in vitro and in vivo models22. The combination of rh-endostatin and doxorubicin produced marked synergistic antitumor activity in a mouse osteosarcoma model8.

Table 2 Multivariate Cox analysis for overall survival
Prior to commencing the current research, many details of the study design were discussed by the authors. First, when is the appropriate time to administer anti-angiogenesis therapy? The metastatic patterns of osteosarcoma show that most lung metastases occurred 6-12 months after surgical treatment23. Further research revealed that the balance of pro-angiogenic factors and inhibitors was disrupted soon after the primary osteosarcoma was removed24. For this study, it was decided to administer anti-angiogenesis therapy perioperatively to prevent the imbalance of pro-angiogenic factors and inhibitors. Second, should anti-angiogenesis therapy be administered alone or in conjunction with chemotherapy? As anti-angiogenesis treatment only prevents new vascular formation, in theory, it is insufficient to destroy the tumor cells25,26. The goal of anti-angiogenesis treatment is to normalize blood vessels to ensure that more cytotoxic drugs reach the tumor cells, as it is these drugs that will eventually eliminate the tumor cells27. This may explain whyanti-angiogenesis therapy alone usually results in limited good outcomes. Third, should the target patients be newly diagnosed non-metastatic or advanced? Once osteosarcoma patients have developed metastasis, it is extremely difficult to cure the patients or to improve long-time survival28-31. The primary goal of improving OS for osteosarcoma patients is to lower the occurrence of distant metastasis at an early stage.

Table 3 The toxicity profile of the two groups
Although it was not possible to perform a randomized study, we attempted to minimize the differences between the groups. Previous studies have shown that age, tumor size,tumor location, and other factors are possible prognostic factors1,32. In the current study, there was no significant difference between the 2 groups in terms of age, sex, tumor location, tumor volume, and tumor margin.
We found that the 2-year and 5-year DMFS rates were significantly improved by 11% and 18%, respectively, with the addition of anti-angiogenesis therapy. For 5-year DMFS,this represents a reduction of 46% for the 39% of patients we would normally expect to develop metastatic disease. The addition of rh-endostatin to chemotherapy resulted in an improvement in the 5-year OS rate from 74% to 87% (P =0.016; relative risk = 0.37). We considered that the improved survival can be ascribed to the decreased occurrence of distant metastasis due to the use of rh-endostatin in addition to standard multi-drug chemotherapy. The higher risk of death in the amputation group than in the limb salvage group may reflect the fact that poor responders were more likely to undergo amputation in real clinical practice.
Regarding the safety profile, there were no more serious adverse effects in the rh-endostatin group than in the control group, consistent with previous findings for the use of other anti-angiogenic agents combined with chemotherapy in the treatment of other malignancies6,33-36.
In summary, the addition of rh-endostatin in patients with newly diagnosed conventional osteosarcoma resulted in a significantly lower occurrence of distant metastases and an improved OS. The addition of rh-endostatin did not increase the rate of adverse effects. However, we do not know whether the addition of rh-endostatin could improve the OS of osteosarcoma patients with advanced disease. The limitations of this research include the non-randomized design and an imbalance in the number of patients between the 2 groups.The current research requires further laboratory and multicenter clinical investigations to evaluate the potential mechanisms and confirm the clinical value of antiangiogenesis therapy in the treatment of osteosarcoma.
Acknowledgements
Ministry of Human Resources and Social Security of the People's Republic of China (MOHRSS) (Grant No. 2017-199). We thank Dr. Conan Hall for his kind revising of this manuscript.
Conflicts of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2019年1期
Cancer Biology & Medicine2019年1期
- Cancer Biology & Medicine的其它文章
- Application of next-generation sequencing technology to precision medicine in cancer: joint consensus of the Tumor Biomarker Committee of the Chinese Society of Clinical Oncology
- The breakthrough in primary human hepatocytes in vitro expansion
- Circular RNAs and human glioma
- Qidong: a crucible for studies on liver cancer etiology and prevention
- The PI3K/Akt/GSK-3β/ROS/eIF2B pathway promotes breast cancer growth and metastasis via suppression of NK cell cytotoxicity and tumor cell susceptibility
- Estrogen and insulin synergistically promote endometrial cancer progression via crosstalk between their receptor signaling pathways
