Use of a combination strategy to improve neuroprotection and neuroregeneration in a rat model of acute spinal cord injury
Elisa García , Roxana Rodríguez-Barrera , Vinnitsa Buzoianu-Anguiano, Adrian Flores-Romero , Emanuel Malagón-AxotlaMarco Guerrero-Godinez, Estefanía De la Cruz-Castillo Laura Castillo-Carvajal Monserrat Rivas-Gonzalez Paola Santiago-TovarIvis Morales Cesar Borlongan, Antonio Ibarra ,
1 Centro de Investigación en Ciencias de la Salud (CICSA), Facultad de Ciencias de la Salud, Universidad Anáhuac México Campus Norte,Huixquilucan, Edo. de México, México
2 Centro de Investigación del Proyecto CAMINA A.C.; Ciudad de México, México
3 Unidad de Investigación Médica en Enfermedades Neurologicas, Hospital Especialidades CMN Siglo XXI, Ciudad de México, Mexico
4 Unidad de Rehabilitación Osteoarticular. Instituto Nacional de Rehabilitación. Luis Guillermo Ibarra Ibarra, Ciudad de México, Mexico
5 Center of Excellence for Aging and Brain Repair, Department of Neurosurgery and Brain Repair, University of South Florida Morsani College of Medicine, Tampa, FL, USA
Abstract Spinal cord injury is a very common pathological event that has devastating functional consequences in patients. In recent years, several research groups are trying to find an effective therapy that could be applied in clinical practice. In this study, we analyzed the combination of different strategies as a potential therapy for spinal cord injury. Immunization with neural derived peptides (INDP), inhibition of glial scar formation (dipyridyl: DPY), as well as the use of biocompatible matrix ( fibrin glue: FG) impregnated with bone marrow mesenchymal stem cells (MSCs) were combined and then its beneficial effects were evaluated in the induction of neuroprotection and neuroregeneration after acute SCI. Sprague-Dawley female rats were subjected to a moderate spinal cord injury and then randomly allocated into five groups: 1) phosphate buff-ered saline; 2) DPY; 3) INDP + DPY; 4) DPY+ FG; 5) INDP + DPY + FG + MSCs. In all rats, intervention was performed 72 hours after spinal cord injury. Locomotor and sensibility recovery was assessed in all rats. At 60 days after treatment, histological examinations of the spinal cord (hematoxylin-eosin and Bielschowsky staining) were performed. Our results showed that the combination therapy (DPY+ INDP + FG+ MSCs) was the best strategy to promote motor and sensibility recovery. In addition, significant increases in tissue preservation and axonal density were observed in the combination therapy group. Findings from this study suggest that the combination theapy (DPY+ INDP + FG + MSCs) exhibits potential effects on the protection and regeneration of neural tissue after acute spinal cord injury. All procedures were approved by the Animal Bioethics and Welfare Committee (approval No. 178544; CSNBTBIBAJ 090812960)on August 15, 2016.
Key Words: fibrin glue; mesenchymal stem cells; glial scar; protective autoimmunity; neural derived peptides;neural regeneration
Introduction
Spinal cord injury (SCI) triggers a cascade of events that increase tissue damage and lead to a continuous and exacerbated in flammatory response at the site of injury (Trivedi et al.,2006; Popovich, 2014). In central nervous system (CNS), the non-controled intensity of immune response provokes a negative effect, inducing more neural tissue loss and thus, a poor functional recovery (Dietrich et al., 2004). Therefore, the use of any therapy capable of modulating this reaction after SCI, is of utmost importance in limiting the damage (Liu et al., 1997).After studying neuroprotective strategies, the next challenge is to find the way of restoring neural tissue. To initiate this process, it is important to consider the existence of the scar formed after SCI. Both glial scar and the accumulation of a large number of molecules are considered an important barrier for neural regeneration in healing response (Silver and Miller, 2004; Fitch and Silver, 2008; Hu et al., 2010).
Several strategies are currently explored to promote neuroprotection or neuroregeneration after SCI. However, these strategies are endowed by different terapeutic mechanisms that separately neutralize only one or some of the degenerative phenomena induced after SCI. That is why, in order to implement the best strategy that achieves first, to neutralize the main degenerative phenomena observed after SCI and after, to contribute restoring neural tissue; we need to combine several strategies that display different beneficial effects.
In the present study, we explored the effects of combining:1) immunization with neural-derived peptides (INDP), 2) scar formation-inhibition using 2-2 dipyridyl (DPY), 3) fibrin glue(FG) as scaffold of 4) mesenchymal stem cells (MSCs). The rationale for using this combination was based on the beneficial effects that, individually, these strategies have shown.
INDP has conferred neuroprotective effects in SCI models(Ibarra et al., 2010; Garcia et al., 2012; Rodríguez-Barrera et al., 2013) and has also shown a significant effect in neural restoration since it is capable of inducing neurotrophic factors and neurogenesis (Cruz et al., 2015; Martiñón et al., 2016).
MSCs have been demonstrated to modulate the CNS environment promoting tissue protection and its repair (Krabbe et al., 2005; Quertainmont et al., 2012).
Scar inhibition has also been implemented as a therapeutic procedure after SCI. The use of DPY, an iron chelator, promotes extensive long-distance regeneration of injured axons(Klapka et al., 2005; Niclou et al., 2006). The use of FG after SCI promotes the growth and incorporation of afferent axons and intervenes in the support of the directionality of them (Cassell et al., 2001; Liu et al., 2013; Buzoianu-Anguiano et al., 2015). The action mechanism of these biomaterials is to provide a “support” for the placement of different stem cell types (Xiao et al., 2016).
The purpose of the present study was to investigate the effect of a combination therapy (DYP + INDP + FG + MSCs)in the treatment of acute SCI.
Materials and Methods
Ethical considerations
All procedures were carried out in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the Mexican Official Norm on Principles of Laboratory Animal Care (NOM 062-ZOO-1999). In addition, animal protocol and procedures were approved by the Animal Bioethics and Welfare Committee(approval No. 178544; CSNBTBIBAJ 090812960) on August 15, 2016. All experiments were designed and reported according to the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines.
Experimental design and groups
Forty-two female Sprague-Dawley rats, 12 to 15 weeks old,weighing 200 to 250 g, were supplied by the Animal Breeding Center of the Faculty of Health Sciences of the Anahuac University. Animals were grouped and housed in pairs in a room with 12-hour light/dark cycles and controlled temperature of 25°C. They had water and food ad libitum throughout the duration of the experiment.
The sample size was calculated using an alpha of 0.05 and beta of 0.20. Intervention was performed 72 hours after a moderate SCI contusion, with subsequent analysis carried out over the following 2 months.
After injury, rats were randomly allocated into five groups:1) PBS (n = 7); 2) DPY (scar inhibitor) (n = 7); 3) DPY +INDP (n = 7); 4) DPY + FG (n = 7); and 5) DPY + INDP+ FG + MSC (combination therapy; n = 7). We also used a group of sham operated rats (n = 7).
SCI model
Rats were anesthetized by intramuscular injection with a mixture of ketamine (50 mg/kg, Probiomed, Mexico City, Mexico) and xylazine (10 mg/kg; Fort Dodge Laboratories, Fort Dodge, IA, USA). Thirty minutes later, animals were subjected to laminectomy of the T9 vertebrae. Then, a moderate SCI was in flicted; a 10 g rod was dropped onto the exposed spinal cord at a force of 200 kd at a 2 mm height above the spinal cord using a spinal cord impactor (Precision Systems & Instrumentation, Lexington, KY, USA) (Franz et al., 2014).
At the end of the surgery, hemostasis was controlled, and internal planes were closed with 3-0 polyglycolic acid suture and 3-0 nylon cutaneous plane. After surgery, rats were hydrated with 2 mL of 0.9% saline solution via intraperitoneal injection. Antibiotic therapy of 0.1 mL enro floxacin (Baytril,Bayer®, Mexico City, México) diluted in sterile water (1:10)was administrated through subcutaneous injection, once a day, and analgesic therapy of 0.5 mL acetaminophen (Tempra 10 mg/mL, 10 mg/kg, Bristol Myers Squibb®, Mexico City, Mexico) was administered via intraperitoneal injection for 5 days. Rats were placed in polycarbonate boxes (two animals per box) and received manual bladder expression three times daily until recovery of the micturition reflex. Animals with signs of infection were excluded from the study.
Intervention
Combination therapy was carried out 72 hours after injury as follows:
Glial scar inhibition
Rats were anesthetized with the same cocktail as previously described. The contused area was cleaned, and the muscles were separated. Then a 2 mm paramedial incision was made in the meninges, just above the site of injury (T9), and the necrotic tissue was removed. DPY was directly injected six times into each stump of the spinal cord with a Hamilton siringe, 6 μL rostral and 6 μL caudal to the injury. Each injection deposited 2 μL volume of DPY (16 nmol) diluted in PBS, at the end of the process the meninges were sutured with 9-0 mono filament nylon.
Isolation and phenotyping of MSCs
MSCs were obtained from healthy rats that were euthanized with an overdose of sodium pentobarbital. Bone marrow was acquired from both femurs and tibias (n = 7) using a 200 μL micropipette and deposited in a 15 mL conical tube with culture medium (Dulbecco's modified eagle's medium(DMEM); Thermo Fisher Scientific, Inc., Waltham, MA,USA). Afterwards, the sample was centrifuged at 35 × g for 7 minutes. The cells were then separated at 63 × g at 24°C for 30 minutes in Ficoll-Hypaque (Sigma-Aldrich, St. Louis,MO, USA) (3 mL). The total number of nucleated cells was quantified and 9 × 106cells were seeded into a 75 cm2cultureflask containing 5 mL DMEM with 20% fetal bovine serum(FBS; Thermo Fisher Scientific Inc., USA), 1 mL L-glutamine(Thermo Fisher Scientific Inc.), 5 mL hydroxyethyl-piperazineethane-sulfonic acid buffer (Sigma-Aldrich), and 1 mL penicillin-streptomycin (Gibco). They were then placed in a water-jacketed incubator at 37°C with 5% CO2until the cells formed a fibroblast monolayer. Finally, the MSCs were reseeded onto the fibroblast layer and maintained for 2 weeks until transplantation. Passage 4 MSCs expanded in culture were phenotypically characterized by flow cytometry. An approximate number of 2 × 106cells were centrifuged at 35× g for 5 minutes and they were incubated with antibodies(PE anti-rat CD90/mouse CD90.1 “Thy-1.1” (Biolegend,San Diego, CA, USA), PE/Cy7 anti-mouse CD105 antibody(Biolegend), anti rat-CD117 (Merck KGaA, Darmstadt,Alemania), anti rat-CD13 (Santa Cruz Biotechnology Inc.,Dallas, TX, USA), anti-CD34 “ICO-115” antibody (Alexa Fluor®488; Santa Cruz Biotechnology), all at a dilution of 1:100, in the dark for 20 minutes at 4°C. They were washed twice with a fluorescence-activated cell sorter (FACS) buffer before centrifugation again at 35 × g for 5 minutes. Finally,flow cytometry was performed and analyzed using the BD FACSCantoTMII System with a CellQuest Pro program (BD Biosciences, San Diego, CA, USA).
Cell phenotype proportion: 96.5% of the cells were mature MSCs, 80.45% of cells were positive for CD13 (a marker for MSC subpopulation), 51% of cells were positive for CD90 (a marker for MSC subpopulation), 35% of cells were positive for CD105 (a marker for MSC subpopulation), 11.49% of cells were positive for CD117 (a marker for MSC subpopulation),10.5% of cells were double positive for MSC subpopulations and 3.5% of cellular population was positive for CD34 (a specific control marker for hematopoietic stem cells). Therefore,the majority of transplanted cells were adult MSCs.
Administration of FG and MSCs
A mixture of MSCs (2.5 × 106cells in 5 μL) and FG (Baxter®;10 μL) was grafted at the site of injury using a Hamilton syringe. Finally, the meninges were sutured with a 9-0 suture and the aponeurotic plane and skin were separately sutured with nylon thread.
INDP
INDP was performed using the peptide A91, a non-encephalitogeic peptide derived from the sequence 87-99 of the myelin basic protein. Non-encephalitogenicity was obtained by replacing the lysine residue at position 91 with alanine.Immunization was performed subcutaneously at the base of the tail with 150 μg peptide A91. The peptide was diluted in phosphate buffer solution (PBS; 0.5 M, pH 7.4) and emulsified in an equal volume of complete Freund's adjuvant (ACF,Sigma-Aldrich) containing 0.5 mg/mL Mycobacterium tuberculosis (Sigma-Aldrich).
Evaluation of motor recovery
Locomotor function recovery was evaluated in an open field weekly during a 60 day study period using the Basso, Beattie& Bresnahan (BBB) Locomotor Rating Scale (Basso et al.,1995). The scale score ranges from 1 (no movement) to 21(normal movement). Rats were allowed to move freely in an open field. Three blinded examiners implemented the test.Rat motor behaviors were observed for 5 minutes for the evaluation of locomotor function recovery. The first evaluation was performed 48 hours after injury (24 hours before treatment administration).
Sensibility evaluation (Von Frey test)
Mechanical hypersensitivity was assessed by measuring the hind paw withdrawal response after pressure stimuli with Von Frey filaments (Sundberg et al., 2010). This evaluation was performed before and 60 days after SCI. The rats were placed in an acrylic glass chamber and the response was recorded using an Electronic von Frey Anesthesiometer (IITC Life Science, Inc., Woodland Hills, CA, USA). Hind plantar surfaces were stimulated with Von Frey plastic semi- flexible filaments.To determine if the animals were experiencing allodynia at a given time point, the average of three pressure values recorded for each paw was compared to the baseline score that was recorded prior to injury. The data were expressed as g/cm2.
Histopathological examination
Rats were euthanized (n = 7 per group) with sodium pentobarbital (80 mg/kg, Probiomed, Mexico City, Mexico) via intraperitoneal injection 60 days after SCI and perfused with intra-aortic heparin (1%), 100 mL PBS (pH 7.4) at 4°C and 400 mL 4% paraformaldehyde (pH 7.4) at 4°C.The SCs were then removed (1.0 cm caudal/rostral from the injury site) and cryosectioned (12 sequential 20 μmthick sections) at 0, 1, 2 and 4 mm caudal and rostral from the epicenter. Modified Harris hematoxylin solution(Sigma-Aldrich) and Eosin Y (Sigma-Aldrich) were used in the histopathological examination. Hematoxylin and eosin-stained sections were cut to evaluate the spared tissue that was defined as tissue areas (mm2) in which normal spinal cord architectiure was preserved (tissue with no cysts or unorganized tissue) (Garman, 2011). To quantify axonal density, Bielschowsky silver impregnation was performed with 20 μm-thick paraffin sections. The rehydrated sections were covered with 20% AgNO3and incubated at 37°C in the dark for 30-40 minutes. The solution was washed off with distilled water and replaced by ammonia silver solution for 10 minutes in the dark. After incubation, two washes with distilled water were performed. The slides were immersed in ammonia-water to develop the silver stain for 5—10 minutes. After two washes with distilled water, the reaction was stopped using 5% sodium thiosulfate for 3 minutes. Then sections were rinsed, dehydrated, cleared, and mounted (Litch field and Nagy, 2001).Bielschowsky silver-stained (Sigma-Aldrich) sections were used to evaluate axonal density, which was defined as the stained area with a dark tone; unorganized tissue and cysts were excluded from the analysis. Hematoxylin-eosin staining and Bielschowsky silver staining images were digitized under a 20× objective (Olympus BX-41, Tokyo, Japan) and assesed with the image analysis system ImageJ software(v.1.46, National Institutes of Health, Bethesda, MD, USA).The areas positive for hematoxylin-eosin staining and Bielschowsky silver staining were quantified. The data were expressed as the tissue preserved/mm2for hematoxylin-eosin staining. In the case of axonal density, the data was expressed as the percentage obtained from the spinal cord of a sham group underwent only laminectomy.
Statisticals analysis
Data are expressed as the mean ± SD and were analyzed using Graph Pad Prism 6.0 software (GraphPad Software Inc., San Diego, CA, USA). One-way analysis of variance followed by Tukey's test was used to analyze sensibility recovery. Preserved tissue, axonal density, and locomotor function recovery were analyzed using the one-way repeated measures analysis of variance. A P-vaue < 0.05 was considered statistically significant.
Results
Locomotor function of rats
Although all treated rats exhibited a better motor improvement compared with control rats, the animals treated with DPY + INDP + FG + MSC presented significantly greater locomotor function recovery. From the 2ndweek, locomotor function recovered to a larger extent in the combination group than in the PBS, DPY, DPY + INDP, and DPY + FG groups. This improvement was maintained and even increased until the end of the experiment (P < 0.05) (Figure 1).
Mechanical hypersensitivity of rats

Figure 1 The combination therapy induced better locomotor recovery after spinal cord injury.
As SCI and the consequent inflammatory reaction trigger nociceptive hypersensitivity (Colburn and Rickman, 1999),we evaluated the development of mechanical hypersensitivity. In this case, the lower is the damage, the less is the mechanical hypersensitivity, and thereby the withdrawal threshold is greater (the animal needs higher level of pressure to stimulate withdrawal response). Therefore, hind paw mechanical hypersensitivity was assessed by measuring withdrawal threshold of mechanical stimulation with von Frey filaments.
This test was performed before and 60 days after SCI.Before injury, the results of the test were similar among the studied groups. There were no significant differences in test results between studied groups (P > 0.05).
Sixty days after SCI, the DPY + INDP + FG + MSC and DPY + INDP groups showed a significant increase in the mechanical withdrawal threshold compared with PBS, sham-operated and the other spinal cord injured groups (P <0.0001; Figure 2). The mechanical withdrawal threshold was also increased in sham-operated rats compared with those in the PBS, DPY, and DPY + FG (P < 0.001; Figure 2).
Histopathological features
To assess the neuroprotective effects of the combination therapy, we quantified the spared tissue 60 days after SCI.Figure 3 shows that animals in the DPY + INDP + FG +MSC or DPY + INDP group exhibited a significant increase in the amount of spared tissue in the rostral and caudal portions from the epicenter. The amount of spared tissue in the DPY + INDP + FG + MSC or DPY + INDP group was significantly higher than that in the PBS group. The combination therapy (DPY + INDP + FG + MSC) induced a higher amount of spared tissue than the theapy DPY + INDP (P <0.05; Figure 4).
Axonal density was to quantify the percentage of stainedarea 60 days after SCI. The Bielschowsky silver staining joins AgNO3 to the axon microtubules, giving them a dark tone;in this way, it is possible to identify the axonal density in each cross-section of the spinal cord. Figures 5 and 6 show a higher density of axonal fibers in rats treated with DPY +INDP + FG + MSC or DPY + INDP. Similarly, the quanti fication of axonal density showed a significant increase in rats treated with the combination therapy (DPY + INDP + FG +MSC; P < 0.001, vs. PBS; P < 0.05, vs. DPY and DPY + FG; P= 0.05, vs. DPY + INDP) and those subjected only to DPY +INDP (Figure 7).
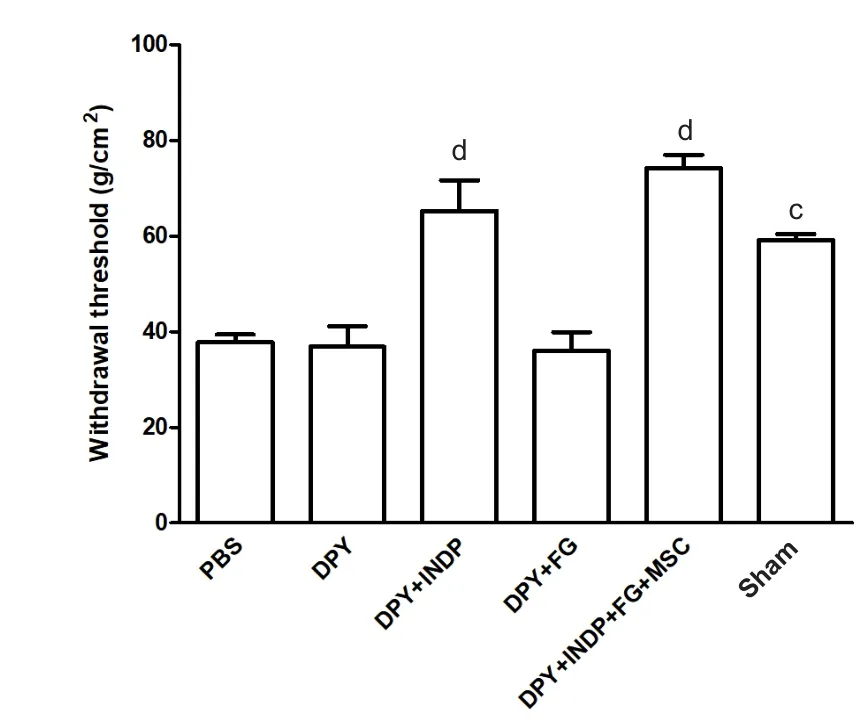
Figure 2 The combination strategy improves the nociceptive hypersensitivity after spinal cord injury.
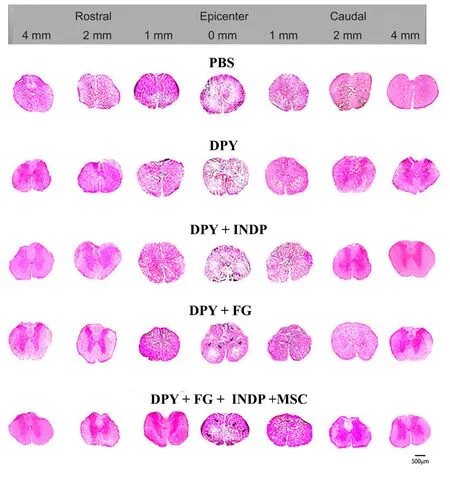
Figure 3 Representative hematoxylin and eosin stained cross-sections of the injured spinal cord at different distance sites (both rostral and caudal) from the epicenter at 60 days after spinal cord injury.
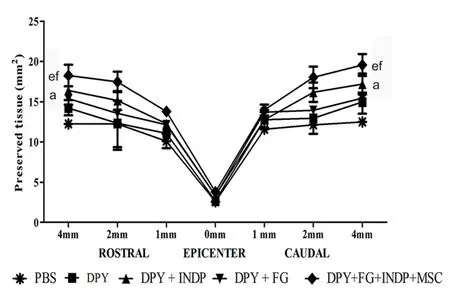
Figure 4 The combination therapy increases the amount of spared tissue.

Figure 5 Bielschowsky's silver stain shows cross-sections of the injured spinal cord at different distance sites (both rostral and caudal) from the epicenter at 60 days after spinal cord injury.

Figure 6 Bielschowsky silver staining of nearby areas to central canal at 60 days after spinal cord injury.
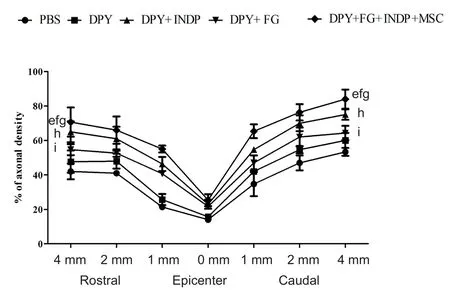
Figure 7 Spinal cord injury rats treated with the combination therapy show a higher axonal density.
Discussion
After SCI, self-destructive mechanisms produce neuronal loss and avoid regenerative processes (Kasahara et al.,2006; Donnelly and Popovich, 2008). Nowadays, there is no effective therapy that, at the same time, neutralizes the degenerative phenomena and promotes an effective neural restoration. Recent studies have shown important advances in this issue; however, up to day, none of the strategies has demonstrated completely satisfactory results. For this reason, ongoing investigations are aiming to find innovative treatments that achieve this goal. In line with this, some investigations have shown a better morphological and functional recovery when treatment includes more than one strategy (Chiba et al., 2009; Gu et al., 2010; Martiñón et al.,2012; del Rayo Garrido et al., 2013; Rodríguez-Barrera et al.,2017).
In the present work, we investigated the effect of combining four different strategies on the behavioural and morphological recovery of rats with acute SCI. Our results demonstrated that, animals treated with DPY + INDP +FG + MSC presented the best motor and sensory recovery as compared with animals in the other studied groups. The improved locomotor recovery was observed from the first week of therapy, suggesting a neuroprotective effect induced by this combination strategy. This favorable effect could be the result of the sum of the protective mechanisms provided by INDP and MSC. The neuroprotective effect exerted by INDP has already been reported by numerous studies. For instance, it has been shown that INDP is capable of reducing lipid peroxidation (Ibarra et al., 2010), apoptosis (Rodríguez-Barrera et al., 2013), nitric oxide production (García et al., 2012) and proinflammatory cytokines (García et al.,2018). In addition, INDP induces a significant increase in brain-derived neurotrophic factor (BDNF), a neurotrophic factor, involved in neuroprotective mechanisms and anti-inflammatory cytokines (Martiñón et al., 2012, 2016;García et al., 2018). All of these actions contribute greatly to tissue protection and thus improve functional recovery.MSCs also contribute to neuroprotection (Neuhuber et al.,2005). These cells have been reported to be capable of reducing SCI-cavities and improving behavioral function in rats after spinal cord contusion (Ohta et al., 2004). To achieve this neuroprotective effect, transplanted MSCs could exert an immunomodulatory effect that contributes to notable changes in SCI environment. There are significant increases in interleukin-4 and interleukin-13 levels, but reductions of tumour necrosis factor-α and interleukin-6 levels. These changes were associated simultaneously with high numbers of alternatively activated macrophages (M2 phenotype), and decreased numbers of classically activated macrophages (M1 phenotype). This inmunomodulation has been associated with locomotor function recovery in MSCs-transplanted rats, which correlated with preserved axons, less scar tissue formation and increased myelin sparing (Nakajima et al.,2012). Finally, MSCs are also capable of producing BDNF,which can enhance tissue protection (Lu et al., 2005).
In the present study, the combination strategy also induced neuroregeneration. The increased axonal density observed in this group of animals could support this motion.In previous studies, we demonstrated that BDNF and neurotrophic factor-3 production increased at the site of injury after active immunization with INDP. Moreover, our results showed that the rats receiving INDP presented an improved motor performance that was maintained over time as compared to those treated with PBS only (Martiñón et al., 2016).These observations shed light onto beneficial neuroregeneration effects, even at the chronic stages of injury. Previous studies performed in models of ischemic stroke have also shown that INDP is capable of inducing important changes at the choroidal plexus which correlated with a significant increase in the expression of genes encoding for BDNF, neurotrophic factor-3, interleukin-10 and transforming growth factor-β and a significant increase in neurogenesis (Cruz et al., 2015, 2018). INDP has been reported to induce a better neurological performance and increase hippocampal and cortical neurogenesis (Ziv et al., 2007).
The implantation of MSCs helps to provide an optimal microenvironment for axonal regeneration (Buzoianu-Anguiano et al., 2015). Several studies have reported that MSCs might provide a better environment for damaged tissue and save remaining neurons by neurotrophic factors or cytokines that induce the tissue preservation, axonal growth and neurogenesis after SCI (Barnabé-Heider and Frisén, 2008;Vaquero and Zurita, 2009; Kan et al., 2010). The use of MSC in this study promoted and enhanced the motor recovery,tissue preservation and a better axonal density in the group treated with the combination therapy (DPY + INDP + FG +MSC).
The implantation of MSCs into a fibrin matrix (FG) reinforces in some way its favorable effects. FG forms a sealant that can maintain tissue approximation. Aside from this,nutrients, cytokines, and trophic factors can pass through the fibrin glue networks (Cheng et al., 1995). The use of FG in cell transplantation therapies, besides providing a biodegradable scaffold for axonal growing, has promoted the increase of BDNF, glial-derived neurotrophic factor,neurotrophic factor-3, antinflammatory cytokines and has been shown to induce motoneuron survival and locomotor function recovery (Menovsky and Beek, 2001; Barbizan et al., 2013, 2014).
Finally, scar acts as a physical and chemical barrier, and it is an obstacle to axonal growing and thus, to allow the action of interventions (Beck et al., 2010). That is why several investigations have been directed to inhibit scar formation, thus improving axonal regeneration (Ikeda et al., 1992; Schiwy et al., 2009). In the present work, we inhibited scar formation using DPY, which is a chelating molecule that inhibits the formation of type III collagen fibers (Gallo and Deneen,2014). This strategy could also induce a better neurological and morphological outcome in combination-treated animals. Regarding this, previous studies in our laboratory have demonstrated that the combination of DPY-scar inhibition and INDP improves locomotor recovery after SCI, even at the chronic stages of injury (Rodríguez-Barrera et al., 2017).Our results suggest that in the acute phase, scar inhibition with DPY contributes to a better locomotor recovery than the one observed in the other groups. The morphological analysis demonstrated a statistically significant difference in the axonal density presented by DPY + INDP + FG + MSC and DPY + INDP groups, which could be an evidence of the regenerative process induced by the combination therapy.This observation could be clinically evidenced by the results obtained in the sensibility evaluation. Von Frey test showed a significant increase in the mechanical withdrawal threshold of aforementioned groups. This finding indicates that DPY + INDP + FG + MSCs and DPY + INDP were efficient to diminish the mechanical hypersensitivity observed after SCI. According to our results, this beneficial effect could be the consequence of diminished tissue damage (neuroprotection) but also the result of an increased tissue restoration(neuroregeneration). Reduction of hypersensibility is a relevant finding as it develops neuropathic pain like allodynia (non-noxious stimuli become noxious) or hyperalgesia(noxious stimuli become more noxious) (Berrocal et al.,2014). These painful sensations can disturb behavioral function and reduce the quality of life (Vogel et al., 2017). Since no cure is currently available for this type of chronic pain,the sensitive outcome observed in these groups of rats is a promissory benefit for individuals with SCI.
Altogether, results of this study envision a promissory therapy for SCI; however, to provide more satisfactory evidence, it is necessary to plan more investigations. In this preliminary study, we demonstrated that the combination therapies could be a viable strategy with better results than using individual therapies for SCI treatment.
The combination therapy proposed in this study displayed an increased locomotor function recovery, which was associated with improved neuroprotection and possibly better neuroregeneration. Future studies are guaranted to elucidate the exact mechanisms responsible for the observed bene ficial effects.
Author contributions:Study design and paper writing: EG and AI;surgery implementation and care of animals: AFR and EMA; data analysis: RRB and AI; purification of mesenchymal stem cells: VBA;providing histological technique: MGG, EDCC, and LCC; analysis of histological images: MRG and PST; experimental studites: IM; experiment analysis and supervision: CB; fundraising, study supervision and analysis: AI. All authors approved the final version of this paper.
Conflicts of interest:The authors declare that they have no competing interests.
Financial support:This work was supported by the National Council of Science and Technology of Mexico (CONACYT), No. 178544. The funder had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Institutional review board statement:All procedures were approved by the Animal Bioethics and Welfare Committee (approval No. 178544;CSNBTBIBAJ 090812960) on August 15, 2016 and carried out in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the Mexican Official Norm on Principles of Laboratory Animal Care (NOM 062-ZOO-1999). All experiments were designed and reported according to the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- Busting the myth: more good than harm in transgenic cells
- Comparative study of microarray and experimental data on Schwann cells in peripheral nerve degeneration and regeneration: big data analysis
- Lessons from glaucoma: rethinking the fluid-brain barriers in common neurodegenerative disorders
- Characteristics and advantages of adenoassociated virus vector-mediated gene therapy for neurodegenerative diseases
- Gene expression changes in dorsal root ganglia following peripheral nerve injury: roles in in flammation, cell death and nociception
- Nicotinamide adenine dinucleotide phosphate oxidase activation and neuronal death after ischemic stroke