The problems of nutritional support for head and neck malignant tumor patients undergoing radiotherapy
Ying-Na Bao
1Department of Radiotherapy,The Affiliated Hospital of Inner Mongolia Medical University,Hohhot 010050,China.
Abstract Nutritional support is a vital approach to improve symptoms of head and neck cancer,which are caused by radiotherapy.Although nutritional support has rapid progress,it could appear a variety of problems in nutritional treatment for head and neck cancer patients during radiotherapy.It is introduced that how to implement nutritional support for head and neck cancer patients during radiotherapy.It is more important to analyze the problems in nutrition assessment and nutrition support and intervention.It could be designed more convenient nutrition assessment system and try to find out more sufficient and effective nutrition markers.It also needs to enhance the nutrition education for patients and their family.In addition to,it could be more work to do in oral,nasal feeding and gastrostomy nutrition supplementation and parenteral nutrition support and intervention.Thus,it is a long way to make nutritional support be better in head and neck cancer patients during radiotherapy.
Key words:Problems of nutritional support,Head and neck cancer,Radiotherapy
Background
Head and neck cancer (HNC)(cancer of the oral cavity,oropharynx,hypopharynx and larynx)is a common cancer in worldwide and constitutes the eighth leading cause of cancer-related deaths worldwide[1].The current major treatment approach for HNC is radiotherapy,which combined with surgery and chemotherapy improved disease control and leaded to better overall survival for HNC[1-4].Despite the therapeutic improvement of HNC by radiotherapy,the side effects of radiation-induced result in malnutrition that is a common condition for HNC patients.The risk of malnutrition associated with radiotherapy threatens the quality of life for HNC patients,which could leads to the increased rate of infections,decreased immunity and obstructed wound healing[5].In spite of the improved survival,radiotherapy is also related to various nutrition-related toxicities for HNC[6].These radiation-induced damages could be classified as two groups:acute damages,which take place during and/or in a short time after radiotherapy and may remain up to 3 months;late damages,which arise months to years after the treatment[6].Radiotherapy is invariably associated with mucositis,altered sense of taste,xerostomia,acute skin reactions,dysphagia,odynophagia,sarcopenia,hematological toxicities and other acute side effects.It could lead to serious physical obstruction of water and food intake and weight loss,which may be life-threatening [7-10].Therefore,it is crucial to decrease risk of malnutrition and improve nutritional status in HNC patients.Although there are many strategies of nutrition interventions in clinical therapy for HNC,it is encountered all kinds of difficulties in actual.This review aimed to review the progress and the problems in the prevention and treatment of malnutrition in HNC patients undergoing radiotherapy as well as their impact on radiotherapy-related toxicity and survival.
Nutrition status assessment for patients with HNC
For improving nutrition of HNC patients,nutrition status assessment is recommended to apply in clinic and detect the nutrition of HNC patients.The purpose of nutrition status assessment is to recognize the patients that are suffered from malnutrition or those are in a risk of it as early as possible,to diagnose the type and grade of malnutrition,and then to observe the achievement of nutrition invention[11].Hence,it is very crucial to make a correct and appropriate nutrition evaluation of HNC patients,and to give an apposite and acceptable nutrition invention for HNC patients.
During radiotherapy,nutrition screening should be repeated weekly for HNC patients [12].ESPEN 2018 for nutrition screening,such as Nutrition Risk Screening 2002 (NRS-2002),Malnutrition Universal Screening Tool (MUST),Malnutrition Screening Tool (MST),Mini Nutritional Assessment Short Form Revised were recommended to be used for evalating nutritional disturbances at an early time [13].For patients with abnormal nutrition,nutrition status assessment,muscle mass,nutrition impact symptoms,physical performance and the degree of systemic inflammation should be evaluated objectively and quantitatively [11].These nutrition assessment tools are applied in actual,including Subjective Global Assessment(SGA),Patient Generated Subjective Global Assessment(PG-SGA)and Minimal Nutritional Assessment (MNA)combine qualitative and semi-quantitative data [11,14].It is shown that decrease of muscle mass can be detected by dual X-ray absorptimetry (DEXA),bio-impedance analysis (BIA),and computed tomography scans at lumbar level 3.Physical performance could be tested using by scales(ECOG,Karnofsky),gait speed,or dynamometry.Serum C-reactive protein (CRP)and albumin are very important inflammation factors that ought to be examined and monitored during radiotherapy for HNC patients [11,15].
Nutrition support and intervention for patients with HNC
HNC patients are frequently malnourished for the cancer expenditure as well as oncological therapy [12],which revealed almost all the HNC patients have similar nutritional demands to the healthy population,generally range between 25-30 kcal/kg/day,with a balance between expenditure and calorie intake.The protein intakes of patients with radiotherapy are estimated to at a least between 1.2 and 1.5 g/kg/day.Nutrition support and invention should be applied to patients with malnutrition or risk of malnutrition,as the intake is less than 60% of their requirements for more than 1-2 weeks,or not able to eat food for 1 week or more were considered as malnutrition [15].Therefore,nutrition counselling has a profound impact on achieving the aim of making nutrition status of patients better and maintaining stable nutrition status.Nutrition counselling involves nutrition history,diagnosis,and nutrition therapy,which should be executed by trained nutrition professionals.It is required doctors must have an effective and adequate communication skills to build trust with patients who are suffered from malnutrition.
Next to nutrition counselling,artificial nutrition support is important for those who could not take food,which includes oral,enteral and parenteral nutrition support [12,15].For most of HNC patients receiving radiation therapy could occur radiation induced damages that may impair the patients’ ability of intake solid foods,therefore,oral nutrition supplements could be first choice to make sure adequate intake of nutrition and may stabilize nutrition status.All kinds of commercially produced shakes are used to provide adequate nutrition or can be used as meal replacements [12].It is very convenient and easy to adoption for patients.If HNC patients are unable to eat,digest or absorb food among radiotherapy,enteral nutrition support should be applied to ensure sufficient nutrition.The types of feeding tubes available are nasogastric,nasojejunal,orogastric,tracheoesophageal fistula tubues,gastrostomy,gastrojejunostomy and jejunostomy.It is demanded that nasogastric,nasojejunal,orogastric,tracheoesophageal fistula tubues are using for short time,less than four weeks.If enteral feeding is prospective to be exercised for longer than four weeks,gastrostomy is recommended [12,16].Meanwhile,several clinical considerations could be decided to choose feeding route,such as:site of tumor,treatment plan,treatment intent,predicted duration of feeding tubes and patient’s wishes.Parenteral nutrition could be performed by an interdisciplinary nutrition support team that contains physicians,pharmacists,registered dietitian,and nurses to decrease complication and ensure safety and efficacy [17].Parenteral nutrition is scarcely used in HNC patients,unless patients who can’t tolerate enteral nutrition or with extensive neck surgery [11,17].During whole nutrition support and invention,nutrition monitoring is very vital and essential,which could observe patient’s nutrition status and complication.Nutrition monitoring is also need multidisplinary team to involve and assess [17].
Problems in nutrition support and intervention for HNC
Nutrition support and invention plays a considerable role for HNC patients during radiotherapy,which may keep nutrition status stabilization of patients and increase treatment efficacy.Although there are many advantages for nutrition application in HNC patients,it still presents some complicated problems when it is in practical performance.
The problems in nutrition assessment
Nutrition assessment is the most important process for patients with HNC during radiotherapy.Only if the patients get correct and true nutrition assessment,symptoms can be effectively alleviated.Nowadays,the nutrition assessment system has a lot of questions during clinical application(Figure 1).
The limitation of application for nutrition evaluation scale
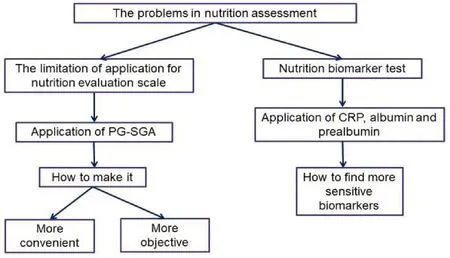
Figure 1 A variety of problems in nutrition assessment for HNC.
Because the characteristic of nutrition support and invention during radiotherapy,it is required to implement and monitor nutrition assessment at least once a week.Though nutrition assessment methods are very convenient to patients and physician,it still contains many contents to examine and needs lots of time.For example,PG-SGA,which is clinically used,contains patient self-assessment and medical staff assessment.The details of PG-SGA include body mass,food intake,symptoms,activities and physical functions,the relationship between disease and nutritional needs,metabolic needs and physical examination.So only patients accurately understand the nutrition assessment contents,it will spend less time to achieve assessment.Some patients with physical,cognitive or emotional problems could not do the subjective assessment[18].For those hospitals without registered dietitian,it will cost a lot of time to complete nutrition assessment by physician.In addition,it also found that PG-SGA scores are correlated with demographic characteristics in common malignant tumors patients.In the study,PG-SGA was used to assess the nutrition status of twenty-three thousand nine hundred and four patients with malignant tumors.Correlation analysis showed that the PG-SGA scores of some tumors were significantly difference in various types of medical insurances,education levels,occupations,regions,and nationalities [19].It is indicated that PG-SGA is more subjective for patients.Due to the volume of patients and contents of nutrition assessment,there is often insufficient time to spend with those who had complex nutritional issues.Nutrition assistant are allied health assistants who specifically work with dietitians,which are trained to work in Australia.The study found that nutrition assistant role resulted in improved patient satisfaction and maintenance of nutritional outcomes demonstrating the effectiveness of this role in supporting the management of head and neck cancer patients within a multidisciplinary treatment clinic [20].Thus,how to design more convenient,relatively objective and easy to understand nutrition assessment is future work.
Nutrition biomarker test
There is no uniform standard for nutrition support and invention in patients with HNC.The American Society of Parenteral and Enteral Nutrition (ASPEN)clinical guidelines recommend initiating nutrition support and invention in patients receiving anticancer therapy who are malnourished and anticipated to be unable to ingest and/or absorb adequate nutrients for seven to fourteen days [21].The European Society of Parenteral and Enteral Nutrition(ESPEN)recommend nutritional support should be initiated when patients are not yet severely malnourished and when the goals of care include maintaining or improving nutritional status [11].Unfortunately,there is no data to confirm the optimal time for initiating nutritional support and invention.Therefore,it is more important to find some nutrition biomarker to point the appropriate time to initiate nutrition support and invention.Systemic inflammation plays a key role in catabolic processes and catabolism of muscle protein.The extent of systemic inflammation may be estimated by measuring serum C-reactive protein(CRP)and albumin [11].Prealbumin is a more sensitive marker than albumin to assess the nutritional status in patients with HNC during radiotherapy.Mean prealbumin level was significantly lower in patients with malnutrition than in those without malnutrition (17±5g/dl vs.22±5g/dl,respectively,p=0.004).Besides,the prealbumin level negatively correlated with the percentage of weight loss(p=0.002)[22].Though C-reactive protein and prealbumin could prognosis nutrition status of HNC patients,it is still not enough for make sure the correct time to nutrition invention.Inflammation-nutrition score,controlling nutritional status score,prognostic nutritional index may be predicting the nutrition status of HNC patients during radiotherapy.We should perform more bench researches to find more sensitive biomarker to change nutrition status of patients.
The problems in nutrition treatment process
Nutritional education

Figure 2 A variety of problems in nutrition treatment process for HNC.
Nutritional education is the first step of nutrition support and intervention.It is included that explaining the pathophysiology of the tumor,imparting nutritional knowledge,proposing nutrition recommendations,completing quality of life questionnaires and nutritional screening and assessment,viewing patient blood and biochemical test results,answering questions from patients and their families,discussing individualized nutrition invention goals.Depending on the difference of region and culture,patients often have complex dietary habit.It is more difficult for them to change their own dietary habit for adapting the new nutrition advice.Besides,patients with cancer are easy to believe one kind of food that can have a magic power to anticancer or have a harmful ingredient for health.So patients often are anxious to discuss dietary options and insist on choosing those foods that are perceived as“protective”(Figure 2).In this case,oncologist and dietitian should be more patient and initiate a counselling about the importance of how to achieve nutrition balance and the risk associated with an inadequate of dietary habit [11].
Oral,nasal feeding and gastrostomy nutrition supplementation
As we all know,the most important parts in nutrition support and invention are oral nutrition supplement and enteral nutrition support,which could maintain patient’s nutrition balance.It is demanded to match patient’s eating habits.In terms of oral nutrition supplement,patients of HNC should use commercial production to keep nutrition status during radiotherapy.However,it is difficult to tolerate some flavors of commercial nutrition supplement for HNC patients among radiotherapy,when they suffered radiotherapy acute side effects.So far,it is an urgent problem that how to supplement nutrition for patients with HNC and make oral nutrition supplement easy to taste to be solved.Many researches are on-going.It is reported that chitosan oligosaccharides had certain anticancer effects and potential application as a synergic functional food ingredient to be oral nutritional supplements of cancer [23].A nutritional supplement with a high blend ratio of w-3 fatty acids is confirmed good for oral mucositis and body weight loss in patients with HNC during chemoraidotherapy [24].
Moreover,it is worth to pay attention to psychological problems of HNC patients,when they require applying all kinds of feeding tubes and ostomy [17].Some HNC patients couldn’t accept their new appearance with a tube in nostril and they feel very embarrassed and shy to meet friends and relatives.It is uncomfortable for HNC patients with radiation-induced malnutrition and radiation side effects placing a nasogastric feeding tube,which could injure the mucosa.In addition,long term enteral nutrition support can be associated with complications,such as constipation,diarrhea,tube site infection,leakage from the tube site,tube dislodgement,and tube clogging.It will bring about a risk of aspiration and pneumonia for patients[17].Besides,the situ of nasogastric feeding tube in patients could have an influence on accuracy of radiotherapy.
Although it has been reported that the complication rates were lower with nasogastric feeding tubes compared to feeding via gastrostomy in cancer patients,compare to feeding tubes,some HNC patients are more willing to receive gastrostomy [11].The reason perhaps is that gastrostomy is hard to be perceived by others and easy to be adapting in psychology of patients.Especially,when patients with HNC during radiotherapy have radiation-induced malnutrition and radiation side effects,gastrostomy is more comfortable than nasal feeding tube and less injure to mucosa.Moreover,it is convenient for food passing intestine by gastrostomy.Despite gastrostomy could bring benefits for HNC patients,it still has other problems urgently to be solved.Parts of patients feel scared to surgery and get a gastrostomy,which are needed to receive adequate and strong nutrition counselling.Others think that it will generate even more cost and lead to heavier family economic burden.The complications of gastrostomy are included local infection of tube site,dislodgment,haemorrahage,bowel perforation,peritonitis,aspiration pneumonia,and mortality [25].The South West Cancer Intelligence Serivce Head and Neck Cancer Gastrostomy Audit found that swallowing ability and continued need for gastrostomy feeding are the major complication of gastrostomy inserted in patients with HNC [25].It is found that the post-insertion mortality rate for percutaneous endoscopic gastrostomy is 4%,with complications reported in 46% of patients,and with 23%-26% being severe or fatal. The study is to investigate gastrostomy versus nasogastric tube feeding for chemoradiation patients with HNC and found that pre-treatment gastrostomy tube feeding is not a cost-effective option [26].
Hence,it is much difficult to make HNC patients with radiotherapy to apply nasogastric feeding tubes and gastrostomy,unless their psychological problems could be deal with and they recognized the importance of nutrition support and invention.In Australia,Eating As Treatment(EAT)program is to improve nutritional status of patients with HNC during radiotherapy using a novel method of training dietitians to deliver psychological techniques to make nutritional behaviors of patients more better.Patients who received the EAT intervention had significantly better scores on the primary outcome of nutritional status and have fewer treatment interruptions.The trial firstly demonstrated the effectiveness of a psychological intervention to increase nutrition in patients with HNC during radiotherapy [27].It is the direction of future work that how to increase patient nutrition treatment compliance through psychological education.Otherwise,the findings revealed that enteral nutrition support could lead to disuse of the swallowing mechanism and long-term tube dependence which has been related with complications including prolonged dysphagia and esophageal constriction [28].How to alleviate the symptoms of swallowing and long-term tube dependence by enteral nutrition also should be studied in the future.
Parenteral nutrition support and intervention
The patients with severe intestinal insufficiency can be improved nutritional status by parenteral nutrition.However,parenteral nutrition has some complications.Bloodstream infections can be serious,which may lead to the interruption of the nutrition,using antibiotics,and exchange of lines.In some patients,parenteral nutrition may cause mild to severe liver dysfunction and allergy.Some complications associated with catheter such as catheter rupture,obstruction,thrombosis,etc.which may result in the limitation for parenteral nutrition [29].Besides,patients need frequent blood tests to make sure that their nutrition is safe. Thus,parenteral nutrition should be complemented by a nutrition support team to reduce complications and improve efficacy and safety.
Refeeding syndrome is defined as the potentially fatal shifts in fluids and electrolytes that may occur in severely malnourished patients receiving artificial refeeding,which include enteral and parenteral nutrition supplement.It is found that the risk factors most strongly involved in the refeeding symptoms were pain,eating difficulties,low handgrip strength,high alcohol intake,and previous radiotherapy in patients with HNC surgery [30].How to decrease refeeding symptoms should be pay more attention in patients with HNC during radiotherapy with enteral nutrition or parenteral nutrition invention.
Conclusion
HNC patients frequently suffer multiple nutritional problems or malnutrition during radiotherapy.It is necessary to use nutrition assessment to evaluate the nutrition status of HNC patients during radiotherapy.When HNC patients accept nutrition support and invention,nutrition monitoring with a focus on symptom management is recommended during radiotherapy.However,there are all kinds of problems associated with nutrition support and invention implement,which should be noted and settled.In summary,all of HNC patients with radiotherapy should get appropriate and timely nutrition assessment,adequate nutrition counselling,and suitable nutrition support and invention.
- Food and Health的其它文章
- Study on the mechanism of Coix seed in the treatment of colon cancer Based on network pharmacology
- Potential relevance of diet to breast cancer
- The therapeutic mechanism of black soybean in atherosclerosis based on network pharmacology
- Nutritional support strategies for cancer cachexia

