Nutritional support strategies for cancer cachexia
Jin Zhang,Hai-Tao Chen,Qing-Hua Yao
1Graduate School of Zhengjiang Chinese Medical University,Hangzhou 310053,China;
2Oncology Department of Integrated Traditional Chinese and Western Medicine,Zhejiang Tumor Hospital,Hangzhou 310022,China.
Abstract Tumor cachexia is widely seen in patients with various stages of cancer,manifested by inadequate intake or abnormal hypermetabolism resulting in negative nitrogen and energy balance.Early intervention of nutritional therapy and penetrate it into other anti-cancer treatment processes can significantly benefit cancer patients who receiving palliative treatment.Nutritional therapy for cancer is a process of planning,implementing,evaluating and nutritional intervention to treat cancer and its complications or physical condition,to improve the prognosis of cancer patients,including nutritional diagnosis (screening/evaluation),nutritional intervention,effi-cacy evaluation (including follow-up)three stages.In practice,we should choose appropriate nutritional risk assessment tools and intervention methods according to the actual situation of patients,avoid over-treatment,reduce complications,and maximize patients'interests as far as possible.Nutritional support therapy for cancer involves ethics,morality and the wishes of patients and their families,and needs further exploration and improvement.The best nutritional support strategy often requires the joint participation of many disciplines,including clinicians,nurses,nutritionists and psychosocial workers.Nutritional support group and multidisciplinary collaboration group on cancer are gradually becoming a trend.With the accumulation of experience in cancer nutrition therapy,the development and application of drugs and nutritional preparations,and the deepening of multi-disciplinary collaboration,more cancer patients will benefit in clinical work.
Key words:Cancer cachexia,Nutritional risk assessment,Nutritional support therapy
Background
Tumor cachexia is a complex syndrome in patients with various stages of cancer.It is characterized by chronic,progressive weight loss and skeletal muscle consumption.It is not sensitive to nutritional intervention or only partially sensitive.It is often accompanied by anorexia,satiety,fatigue and other manifestations,which lead to organ dysfunction.Its pathophysiological characteristics are negative nitrogen and energy balance caused by inadequate intake or abnormal hypermetabolism [1].The diagnostic criteria were as follows [1]:under the condition of no diet,body weight loss in 6 months was more than 5%,or BMI was less than 20 kg/m2 (Europeans and Americans),BMI< 18.5 kg/m2 (Chinese)and any degree of body weight loss was more than 2%,or the appendicular skeletal muscle index of limbs met the criteria of sarcopenia (males <7.26,females < 5.45)and to any extent.Weight loss was more than 2%.
Professor Fearon K[1]proposed three characteristics of cachexia in the International Consensus on Cancer Cachexia in 2011:persistent skeletal muscle loss (with or without loss of adipose tissue);inability to be completely alleviated by conventional nutritional support;progressive functional impairment.Tumor cachexia can be divided into primary cachexia,secondary cachexia and psychogenic cachexia according to its pathogenesis [2].According to the severity and duration of the disease,it can be divided into Marasmus type,Kwashiorkor type,Marasmus-Kwashiorkor mixed type [3].According to the degree of nutritional deficiency,it can be divided into hree degrees--mild type,moderate type and Heavy type.In the 2010 edition of European Clinical Guidelines for Cancer Cachexia,cancer cachexia is divided into three stages:pre-cachexia,cachexia and refractory cachexia [4].
At present,the pathogenesis of cancer cachexia is not completely clear,but the release of inflammatory factors and abnormal enhancement of tumor-related catabolism are considered to be closely related to the occurrence and development of cancer cachexia [5].Tumor cachexia as a common complication of advanced malignant tumors,seriously affects the quality of life of patients and reduces the sensitivity and tolerance of the body to treatment.According to statistics,60% to 80% of cancer patients may have the cachexia,which can occur in any process of cancer development.About 20% of cancer patients died of cancer cachexia [6].
Early detection and intervention of cancer cachexia is the most critical means to prevent its deterioration.In addition to the treatment of anorexia and metabolic disorders in cancer cachexia patients with drugs,current research also focuses on the application of cancer nutrition therapy to treat cachexia,including enteral nutrition and parenteral nutrition.Cancer Nutritional Therapy(CNT)for tumors includes planning,implementation,evaluation and nutritional intervention to treat tumors and their complications or physical condition,so as to improve the prognosis of patients with tumors,including nutritional diagnosis (screening/evaluation),nutritional intervention and curative effect evaluation (including follow-up)[7].In the pre-cachexia and cachexia period,nutrition therapy can not only increase the intake of energy and various nutrients,improve the nutritional status of patients,but also regulate the abnormal metabolism of cancer patients,which is beneficial to anti-cancer treatment,and ultimately improve the quality of life of patients,and even prolong the survival period,bring console to patients and their families [8].Of course,single-mode traditional nutritional therapy is not likely to increase patients'weight and reverse the symptoms of cancer cachexia.Early detection of disease and comprehensive treatment with multiple drugs and methods such as exercise and psychological intervention are more likely to delay its progress [9,10].This article reviews the current nutritional intervention strategies for cancer cachexia patients.
Part I Methods and Tools for Nutrition Risk Assessment
Before carrying out nutritional support treatment for cancer cachexia patients,objective nutritional status assessment must be carried out to guide the follow-up implementation of nutritional support.There are three aspects to evaluate the needs of cancer cachexia patients [11]:the rate of weight loss and protein consumption;energy reserve and intake;inflammation situation.
1.1.General nutritional assessment
It usually includes physical examination,anthropometry and blood biochemical examination,which is a widely used evaluation method.The observed indexes were height(Ht.)and weight (Wt.),BMI,triceps skinfold thickness(TSF),upper arm circumference (AMC),upper arm circumference (AC),serum albumin (ALB),prealbumin (PA)and transferrin (TRF).Some studies [12]show that about 5% of patients with advanced gastric cancer lost weight,decreased albumin and anthropometric index,decreased appetite and quality of life.The nutritional exhaustion status of cachexia can be understood by disease history,clinical manifestations,indicators or comprehensive evaluation indicators.However,single indicators only represent the function of one organ or tissue,and can not represent the function of the whole body.
1.2.Nutritional Risk Assessment Tools
At present,the mainstream nutritional risk assessment tools are:Subjectim Globe Assessment (SGA),patient-generated subjective global assessment (PG-SGA),Mini Nutritional Assessment (MNA),Malnutrition Universal Screening Tools (MUST),Nutritional Risk Index (NRI)and Nutritional Risk Screening Scale (NRS 2002),among them,PG-SGA and NRS 2002 are more commonly used[13-16].
PG-SGA is a widely used rough screening scale based on SGA.The results of the evaluation are divided into three levels:A-level good nutrition,B-level mild malnutrition or suspicious malnutrition,C-level severe malnutrition [17].CSONSC recommends that PG-SGA be used as a nutritional screening and evaluation method for cancer patients,especially cancer cachexia patients.It also suggests that every cancer patient in hospital should be screened and evaluated for malnutrition risk according to the clinical pathway of nutritional therapy established by CSONSC.The cachexia questionnaire was used as a functional evaluation of anorexia/cachexia treatment.
NRS 2002 was proposed and recommended by the European Society of Clinical Nutrition and Metabolism (ESPEN).It is mostly suitable for nutritional risk screening of inpatients with cancer [18].If NRS score≥3 indicates nutritional risk,individualized nutritional support program should be formulated.Although patients with NRS score <3 have no nutritional risk,it is recommended that they be screened once a week during hospitalization.In addition,patients can be classified into 0-4 grades by weight loss ratio and BMI level (grade 0 has the best prognosis and grade 4 has the worst prognosis)[11].
Quality of life assessment (QLQ)is also an important part of the nutritional support effect evaluation system.It mainly evaluates the quality of life and physical condition of cancer patients.At present,EORTC-QOL-C30 questionnaire,McGill Quality of Life Questionnaire (MQOL)and Palliative Treatment Quality of Life Assessment (PQLI)are the tools for assessing the quality of life of cancer patients receiving palliative treatment.In addition,the monitoring of body function in cancer patients receiving palliative treatment should be based on Karnofsky Functional State Score (KPS)or Functional Edmonton Symptom Assessment System (ESAS)[19].ESAS classifies malnutrition in advanced cancer patients as nine common symptoms:depression,anxiety,lethargy,shortness of breath,pain,fatigue,nausea,decreased happiness index and loss of appetite,which are especially suitable for palliative treatment of cancer patients.
Part II Nutritional support strategies for cancer cachexia
Nutritional support therapy for cancer cachexia is a part of comprehensive treatment for cancer patients,which has very important practical significance.Amano et al.[20]studies show that nutritional therapy is essential for cancer cachexia patients,and 76% of advanced cancer patients need nutritional support.Nutritional support therapy usually consists of three parts:physiological requirements,recent cumulative nutrient consumption,additional energy required for disease recovery and tissue synthesis,protein and other nutrients [21].Three principles should be taken into account in nutritional support for palliative cancer treatment:risk and benefit principle,voluntary principle and fair principle [22].
2.1.Nutrition Support Target
In the early stage of anti-cancer treatment,supplemented with nutritional support is mainly to enhance the benefits of anti-cancer treatment,stabilize organ function,slow or reverse weight loss,muscle loss,reduce complications and adverse reactions.But in the late stage of refractory cachexia,the main purpose of nutritional therapy is to control the symptoms related to cachexia,relieve discomfort and improve the quality of life of patients.The basic requirement of nutritional support is to provide more than 70% energy and 100% protein for cancer patients in both early and late stages [23].
2.2.Indicators of nutritional support
The guidelines of the American Society of Parenteral and Enteral Nutrition (ASPEN)point out that [24]:"Nutrition therapy should not be used as a routine adjuvant to surgery,chemotherapy and radiotherapy for cancer patients,but only when there is a risk of malnutrition or malnutrition,nutritional support should be given".If terminal patients with unstable vital signs and multiple organ failure need only a small amount of food and water to prevent mental disorder caused by dehydration,overnutrition treatment will increase the metabolic burden of patients and affect their quality of life.Therefore,nutritional status of patients undergoing palliative cancer treatment should be assessed before nutritional intervention,and nutritional support should be given according to the patient's own situation.The European Association for Palliative Care (EAPC)recommends [25]:If the patient is in good health and has a survival period of more than 3 months,he may die from anorexia/cachexia rather than cancer progression.People without impaired gastrointestinal function may consider using enteral nutrition,while those with gastrointestinal dysfunction may consider using parenteral nutrition.At the same time,active nutritional intervention may also provide opportunities for other anti-cancer therapies.
2.3.Nutritional support methods
Following the five-step malnutrition treatment principle[26]provided by the Cancer Nutrition and Support Therapy Professional Committee of the Chinese Anti-Cancer Association,when the next step can not meet the target needs of 60% of patients,the next step should be chosen to treat malnutrition.(Figure 1)
2.4.Types of Energy Demand
In the 2016 ESPEN Guidelines [11],it is proposed that the energy needs of cancer patients are between 25-30 kcal/(kg·d).Bed-ridden patients can estimate the total energy needs according to 20-25 kcal/(kg·d).
(1)Protein requirements
The rate of protein decomposition is faster than that of protein synthesis in cancer patients,so it is necessary to supplement protein in time,about 1-1.5g/(kg·d),to avoid aggravating negative nitrogen balance.Patients with acute and chronic renal insufficiency should be controlled at 1-1.2g/(kg·d).
(2)Fat demand
Adipose mobilization and fatty acid synthesis increased,lipid synthesis and lipoprotein lipase activity decreased in cancer cachexia patients.Adequate amount of medium and long chain fat emulsion should be given.
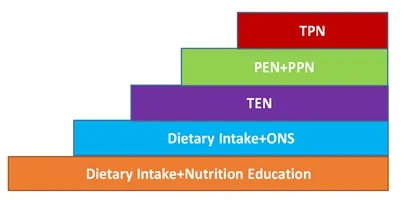
Figure 1 Nutritional Support Therapy "Five Steps"
(3)Glucose-lipid ratio
The optimal energy supply ratio of carbohydrates and fats has not yet been determined.Patients with insulin resistance (IR)and weight loss can increase the energy supply ratio of fat,which can increase the energy density of nutrients and reduce the blood sugar load.
(4)Vitamins and Trace Elements
Statistics from the American Cancer Society (ACS)in 2012 suggest that the demand for vitamins and trace elements in cancer cachexia patients is close to that of normal people [27].Studies have also confirmed that patients who use antioxidants such as vitamin A and vitamin C have an advantage in reducing mortality [28].Therefore,it is recommended that patients with cachexia be supplemented with routine doses of vitamins and trace elements.
(5)Immuno-nutritional preparations
The Studies [29]have shown that ONS rich in ω-3 fatty acids and proteins can improve the quality of life of cancer patients with cachexia,increase body weight and lean tissue,but also has the role of anti-inflammatory factors.Branched chain amino acids (BCAA)can inhibit protein catabolism,promote protein synthesis and increase appetite of patients;L-carnitine can alleviate fatigue,improve appetite and increase lean tissue [30].Eicosapentaenoic acid (EPA)can slow down weight loss,inhibit tumor growth and reduce the production of inflammatory-related cytokines [31].Glutamine:Enhance immune function of cachexia patients,consolidate intestinal immune barrier and reduce protein consumption [32].
2.5. Nutritional support
(1)Nutrition consultation
Cancer cachexia patients often have some dietary problems,such as poor appetite,or can not eat.The inadequate dietary intake can be significantly improved after doctors give specific advice and guidance to cancer cachexia patients.Studies such as Bachmann [33]have shown that dietary recommendations can help improve oral diet in patients with cachexia and control adverse symptoms associated with inadequate dietary intake.Other studies [34]reported that simple dietary recommendations could significantly increase protein-energy intake by mouth,predict malnutrition and cachexia in cancer palliative treatment patients.Common methods include paying attention to diversification of diet,avoiding reasonable dietary restrictions,choosing energy-rich foods,changing the texture of food appropriately and improving its use way.Dining environment,reasonable arrangement of medication time,etc.[35].
(2)Oral Nutritional Supplements (ONS)
In the case that protein intake can not meet the body and disease consumption after dietary nutrition consultation,ONS can be given to patients to improve their nutritional status.There are many oral nutritional supplements,such as those rich in ω-3 unsaturated fatty acids (ω-3 PUFA)or nutrients rich in arginine [36-37].Different nutrients vary according to protein type,osmotic pressure concentration,energy density,lactose,fiber content and dosage form.ONS can reduce weight loss,enhance physical activity,improve quality of life or improve overall survival rate,disease-specific survival rate and local recurrence-free survival rate [38],but it can not improve the mortality rate [39].
(3)Enteral Nutrition (EN)
EN is a special medical food provided by gastrointestinal tract to provide nutrients and other nutrients for metabolism.EN should be preferred when the weight loss caused by inadequate intake is obvious,the intake is not expected to be able to eat for 7 days,the intake is less than 60% of the daily consumption for more than 10 days,and the gastrointestinal function is perfect [40].Implementing methods include oral administration and tube feeding(nasogastric tube,nasointestinal tube,PEG,PEJ,etc.).The advantage of EN is that it can maintain the integrity of gastrointestinal mucosa,regulate the normal intestinal flora,prevent intestinal bacterial translocation,and more in line with the physiological needs of patients.In addition,it has the advantages of convenient application,less complications and low cost.However,the French Federation of International Cancer Centers (FNCICC)recommended[33]:in palliative treatment,attention should be paid to the complications of EN.All nutritional measures should be adjusted to respect the wishes of patients and their families and communicate in a timely manner.When the risk of gastrointestinal complications is included,EN should be banned.In addition,when there is systemic inflammation,it is difficult to restore somatic cell population through EN alone,and it can not bring survival benefits.However,when combined anti-infective therapy and treatment for metabolic abnormalities,there may be positive results.
(4)Parenteral Nutrition (PN)
PN can be used when EN can not meet the nutritional needs of patients or has gastrointestinal dysfunction and can not implement EN.PN is a nutrient (carbohydrate,fat emulsion,amino acid,vitamin,electrolyte and trace elements)needed by patients by intravenous infusion.As an important means of nutrition intervention,it has certain risk and high cost.At present,the most widely used total nutrition admixture in clinical application,parenteral nutrition support for patients with advanced tumors should be carefully carried out.A study [41]reported that the patients with cachexia and malnutrition who had taken EN orally in the late stage were supplemented with PN.It was found that the patients lost weight,improved appetite and improved quality of life.However,when KPS was less than 40 and the average survival time was less than 3 months,only 9% of the patients received PN had improved quality of life [42].
(5)Home Nutritional Support (HNS)
Under the guidance of professional nutritional support team (NST),patients with cachexia who are relatively stable and need nutritional support can receive nutritional support at home,which is called Home Nutritional Support(HNS).Family nutrition support includes home parenteral nutrition (HPN)and home enteral nutrition (HEN)/home enteral feeding (HETF).When choosing HNS for patients with cachexia,especially those with terminal illness,the wishes of patients and their families should be taken into account.Nutrition schemes need to be discussed with patients and their families.Successful HNS requires reliable,safe and comfortable input,and nutrient solution should be selected according to the patient's characteristics.Regular follow-up is an important guarantee for HNS to proceed smoothly.Through follow-up,patients are assessed periodically to determine the continuation,change or discontinuation of nutritional support in the next stage.
(6)parenteral hydration (PH)
Patients with advanced malignant cachexia are often accompanied by dehydration and dietary intake is significantly reduced.At this time,PN can no longer benefit them.Overnutrition treatment will increase the metabolic burden of patients and affect their quality of life.Extra-intestinal hydration (PH)can be considered to prevent the symptoms of mental disorder caused by dehydration.A study [34]showed that PH reduced dehydration symptoms in patients with advanced cachexia who consumed less liquid and could tolerate hydration.At present,the use of artificial nutrition and hydration (ANH)in late palliative treatment is still lack of evidence-based medicine,and ethics is controversial,so we should avoid abusing risk [22].
2.6.Nutritional support-related diseases
According to the way and content of nutritional support,nutritional support complications can be divided into parenteral nutrition and enteral nutrition-related complications.The complications of parenteral nutrition can be divided into venous catheter-related complications,metabolic complications,organ dysfunction and metabolic osteopathy.The common complications of enteral nutrition include mechanical,gastrointestinal,metabolic and infectious factors.Therefore,the need for standardized operation,strict regular monitoring and careful nursing during nutritional support is particularly important for the prevention,detection and timely treatment of complications (such as feeding syndrome,water and electrolyte disorders).
Part III Evaluation and Follow-up of Nutritional Support Therapeutic Effect
3.1.Evaluation of curative effect
Nutrition therapy for cancer cachexia patients is recommended as early as possible.It is generally recommended that 4 weeks be a treatment cycle[23].There are three kinds of evaluation indicators for its efficacy [43]:Rapid changes in indicators such as blood routine,electrolyte,liver and kidney function,inflammatory parameters (IL-1,IL-6,TNF,CRP),albumin,prealbumin,transferrin and retinol binding protein.Free fatty acids,blood lactic acid,etc.were detected 1-2 times a week;Medium-speed change indicators:anthropometric parameters,human component analysis,quality of life assessment,physical fitness assessment,tumor lesion assessment (dual-path method),PET-CT metabolic activity,evaluate every 4-12 weeks;Slow change indicators:survival time,once a year.
3.2 Follow-up
Regular follow-up after discharge,at least once every three months to qualified hospital nutrition clinic or receive telephone nutrition follow-up.
3.3.Nutrition evaluation,curative effect evaluation and follow-up
Implementation by clinicians,nurses and nutritionists qualified for oncology nutrition training;nutritional intervention;and curative effect evaluation by nutritionists and clinicians qualified for oncology nutrition training.
3.4.Home Rehabilitation Guidance [23]
(1)To maintain the ideal body weight,it should not be lower than the lower limit of normal body weight,weigh every two weeks regularly (in the morning after defecation and empty stomach)and record,and return to the hospital in time when the weight loss of unknown cause (non-autonomous)is more than 2%.
(2)Every meal can reach 70%-80% satiety.Non-obese patients should maintain their weight and avoid hunger.
(3)Increase the intake of protein,the combination of buckwheat (1:2).Control the intake of red meat and processed meat.
(4)Increase intake of fruits and vegetables,whole grains and legumes.
(5)Change living habits,quit smoking and limit alcohol,and keep adequate sleep.Nutrients cannot be replaced by health products.Avoid sugary drinks.Avoid salty foods and processed foods with salt.Develop the habit of oral nutrition supplementation.
(6)Exercise not less than five times a week,30-50 minutes per day,with moderate intensity.Bed-ridden patients perform appropriate exercises (including hand,leg,head and neck and trunk movements).Resistance exercise is advocated in elderly patients with muscle loss.
(7)Encourage patients to actively participate in social and social activities.
(8)Pay attention to any abnormal changes of physical symptoms and signs,return to the hospital in time for consultation,and actively seek psychological support,including the use of anti-anxiety drugs.Control pain.
Summary
In summary,nutritional support therapy for cancer cachexia has been paid more and more attention.It has become the most basic and necessary basic treatment for cancer patients.It has become a treatment method which pays equal attention to surgery,chemoradiotherapy,targeted therapy and immunotherapy.Nutrition therapy is essentially a form of palliative treatment.The main purpose of nutrition therapy intervention for advanced cancer patients is to improve their quality of life.Nutritional support should run through other anti-cancer treatment processes,and be detected as soon as possible,and receive nutritional treatment as soon as possible.Before making individual nutritional interventions for patients,doctors should fully evaluate the nutritional status of patients,select appropriate nutritional intervention methods and degrees,avoid over-treatment,reduce complications,and maximize patients'benefits as far as possible.In recent years,research on nutritional support for palliative treatment of cancer patients at home and abroad has gradually risen,but the problem has also begun to highlight.Some relevant treatment experience lacks evidence-based medicine basis,and there is considerable controversy.In addition,it also involves ethics,morality and the willingness of patients and their families,which needs further exploration and improvement.
The best nutrition support strategy requires the joint participation of many disciplines,including clinicians,nurses,nutritionists and psychosocial workers.Multidisciplinary team (MDT),including nutrition support team (NST)and oncology experts,is a growing trend.It is believed that with the accumulation of experience in cancer nutrition therapy,the development and application of drugs and nutritional preparations,and the deepening of multidisciplinary collaboration,more cancer patients will benefit in clinical work.
- Food and Health的其它文章
- The therapeutic mechanism of black soybean in atherosclerosis based on network pharmacology
- The problems of nutritional support for head and neck malignant tumor patients undergoing radiotherapy
- Potential relevance of diet to breast cancer
- Study on the mechanism of Coix seed in the treatment of colon cancer Based on network pharmacology