Potential relevance of diet to breast cancer
Hui-Yang Lin,Xian Wang*
1Department of Medical Oncology,Sir Run Run Shaw Hospital,Zhejiang University School of Medicine,Hangzhou,Zhejiang,China.
Abstract Diet is thought to affect the occurrence and progression of breast cancer while the exact relationship between diet and breast cancer remains largely unclear.This review aims to elucidate the association of specific foods with breast cancer and potential underlying mechanisms.For example,sulforaphane is inversely related to the disease while the impacts of soy and meat on breast cancer are disputable.To some extent,soy is a protective factor while red and processed meat is an adverse one.Due to heterogeneity of breast cancer,menopausal and estrogen receptor statuses can influence the diet-cancer relation.In brief,it may be reasonable to recommend breast cancer patients to eat high soy foods and cruciferous vegetables and low red and processed meat.
Key words:Breast cancer,Soy and isoflavones,Red and processed meat,Sulforaphane
Introduction
Breast cancer is the most frequently diagnosed cancer and the leading cause of cancer-related death in women worldwide [1].The risk factors for breast cancer include age,overweight,physical inactivity and hormone replacement therapy [2,3].When concerning diet,the role related to the disease has been paid much more attention based on the plentiful studies assessing the relationship between breast cancer and specific foods,including red and processed meat [4],dietary carbohydrates and fiber[5],soy food and soy products [6]as well as sulforaphane[7].So far,there yet is not any agreement on the exact effect of diet on the occurrence and development of breast cancer except for the consumption of alcoholic drinks [8].Castello Aet al.[9]found that the Mediterranean pattern was associated with the reduction of 44% of breast cancer incidence,which was rich in fruits,vegetables,legumes,oil fish and vegetable oils while the Western dietary pattern induced a greater risk of breast cancer (OR=1.45,95%CI 1.06-2.01),which was characterized by high-fat dairy products,processed meat,refined grains,sweets,caloric drinks and other convenience food and sauces.Another systematic review of the impact of dietary patterns showed that vegetables was consistently a part of breast cancer protective patterns while red and processed meat consistently consisted in the cancer-causing patterns [10].The incidence of breast cancer in America is much higher than that in Eastern Asia (84.8 VS 39.2 per 100,000)[1].When comparing their diet choices,we found a much lower intake of soy products and cruciferous vegetables in America than that in Eastern Asia.The estimated consumption of soy products of Eastern Asia per day ranged from 6 to 8 g whereas that of America ranged from 1 to 2 g [11].The median intake of cruciferous vegetables of Eastern Asia was 83g/d whereas that of America was 0.2 serving daily [12,13].These studies implied the possible impact of soy,cruciferous vegetables and processed and red meat on breast cancer.So we attempt to summarize the role of these specific foods in the development of breast cancer.
Soy and isoflavones
In the last two decades,the relationship between soy foods and breast cancer has come into public notice because of the estrogenic effect of soy foods.As early as 1990,researchers have found there was a lower incidence of breast cancer in those countries with higher consumptions of soy products [14],which implied the potential antitumor effect of soy foods.The most recent case-control study conducted in Malaysia including 3,683 cases and 3,980 controls showed that consuming soy food once or per week can lower the breast cancer risk by 60% [15].The finding was consistent with Jing Wuet al.’s metaanalysis [16].Based on seven cohort studies,they found a linear relationship between soy foods consumption and reduction of breast cancer risk (p=0.908).However,not all the studies support the protective effect of soy products on breast cancer.When analyzing the data from 378 breast cancer cases and 1,070 control individuals in Shanghai,Shannon Jet al.[17]found that soy products intake was of no effect on breast cancer.Coincidently,Travis RCet al.[6]found no association between dietary intake of soy and risk of breast cancer regardless of the menopausal state after a median follow-up of 7.4 years of a prospective cohort including 37,643 British women aged 20 years and above.In a multiethnic cohort,researchers found that the protective effect was prone to occur in Asian countries rather than western countries.Based on the fact that the consumption of soy foods in Asians is much more than that in western populations,we can infer that the protective effect of soy against breast cancer may be dose-dependent[18].
In addition,there were several studies suggesting menopausal status might have an impact on the incidence of breast cancer when exposed to soy foods.Zhong Xet al.[19]suggested that,on the basis of a meta-analysis of 28 epidemiological studies,the inverse association between soy intake and breast cancer risk was only found in postmenopausal women.On the contrary,Trock BJet al.reported that the reduction of breast cancer risk caused by soy foods intake mainly happened to premenopausal women rather than postmenopausal women [20].Another meta-analysis conducted by Meinan Chenet al.[21]showed that soy foods consumption can decrease breast cancer risk,which did not vary by the menopausal status.Thus,the exact role of menopausal status involved in the development of breast cancer when exposed to soy products remains equivocal.Furthermore,Ji B-Tet al.[22],in the Shanghai Women’s Health Study,observed that both adolescent and adult soy food intake could significantly reduce the risk of premenopausal breast cancer.Similar finding was shown in a cohort study containing 70,578 Chinese women with a median followup of 13.2 years [23].The difference in the study was that the decrease of postmenopausal breast cancer was associated with low adolescent soy intake and high adult soy intake,which indicated that the soy exposure duration might modify the association between breast cancer risk and menopausal status.
When exploring the impact of soy on breast cancer patients,we also found encouraging signs.As early as 2009,through the Shanghai Breast Cancer Survival Study,Shu XOet al.[24]found there was an inversed association between soy consumption after cancer diagnosis with breast cancer and death or recurrence risk of breast cancer,which was independent of estrogen receptor status and tamoxifen use.The lower mortality exposed to postdiagnosis soy food intake was also seen in a meta-analysis of 5 cohort studies while the reduced risk of cancer relapse varied by ER and menopausal statuses [25].Further analysis including the above study and another two cohort studies from US showed that there was a significant decreased risk of recurrence and non-significant one of breast cancer-specific mortality when the consumption of isoflavones was more than 10mg/d [26].But they found such impact was tend to appear to the patients with estrogen receptor negative tumors and tomoxifen use.In a multiethnic cohort study,Fang Fang Zhangetal.[27]observed that all-cause mortality was reduced by 21%when comparing the highest isoflavones intake with the lowest,which was limited to the patients of negative hormone receptors and non-hormonal therapies.On the opposite,a very recent meta-analysis suggested that it was pre-diagnosis soy intake rather than post-diagnosis one that could cut down the mortality and recurrence of breast cancer,which was evident in post-menopausal patients[28].In general,soy and isoflavones exposure is safe for breast cancer patients and may improve their prognosis.Most results from epidemical and clinical studies are presented in Table 1,2,3,4,5.
Soy is abundant of isoflavones.The underlying mechanisms behind the interaction between isoflavones and breast cancer are not clear.Ju YHet al.[29]found that isoflavones promoted the proliferation of estrogensensitive human breast cancer cell,MCF-7,in vitro and when implanted in ovariectomized athymic mice,thus arousing concerns about the adverse effect of soy on breast cancer survivors.Besides,isoflavones increased the expression of BRF2 in MCF-7 cells [30]while the over-expression of BRF2 was related with oncogenesis and poor prognosis [31]and stimulated the bone and lung metastasis in vivo [32].However,the isolfavones metabolism in human differs with that in mice and little epidemical and clinical studies were in line with the above experimental data.Several potential mechanisms of anticancer effect of soy have also been presented.First,due to its similar structure with 17-β-estradiol,soy isoflavones can have an impact on cell growth,oxidative stress and apoptosis via estrogen-receptor signaling pathways [33].Second,Isoflavones have the ability to induce apoptosis through the mitochondrial pathway [34]and inhibit angiogenesis via regulation of multiple pathways [35].Third,Soybeans can inhibit cell growth by decreasing the level of histone demethylase JMJD5 [36].Fourthly,Soyproducts can reduce cancer cell invasion and migration and promote apoptosis by regulating PI3K/Akt/mTOR pathway involved in cell cycle regulation [37,38].Finally,High soy consumption can induce the overexpression of tumor suppressors and downregulation of oncogenes[39].Collectively,the mechanisms are not thoroughly understood and these aforesaid studies provide a new perspective for breast cancer prevention and therapy.
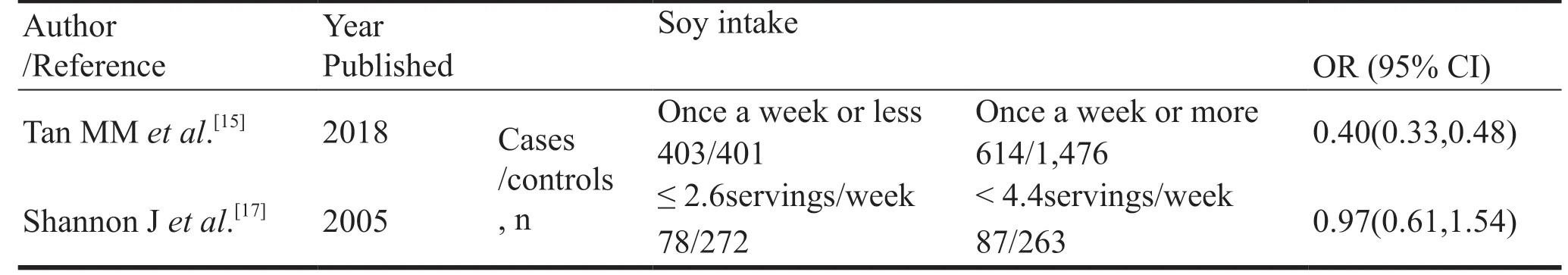
Table 1 Risk estimated from case-control studies of the associations between soy intake and breast cancer incidence
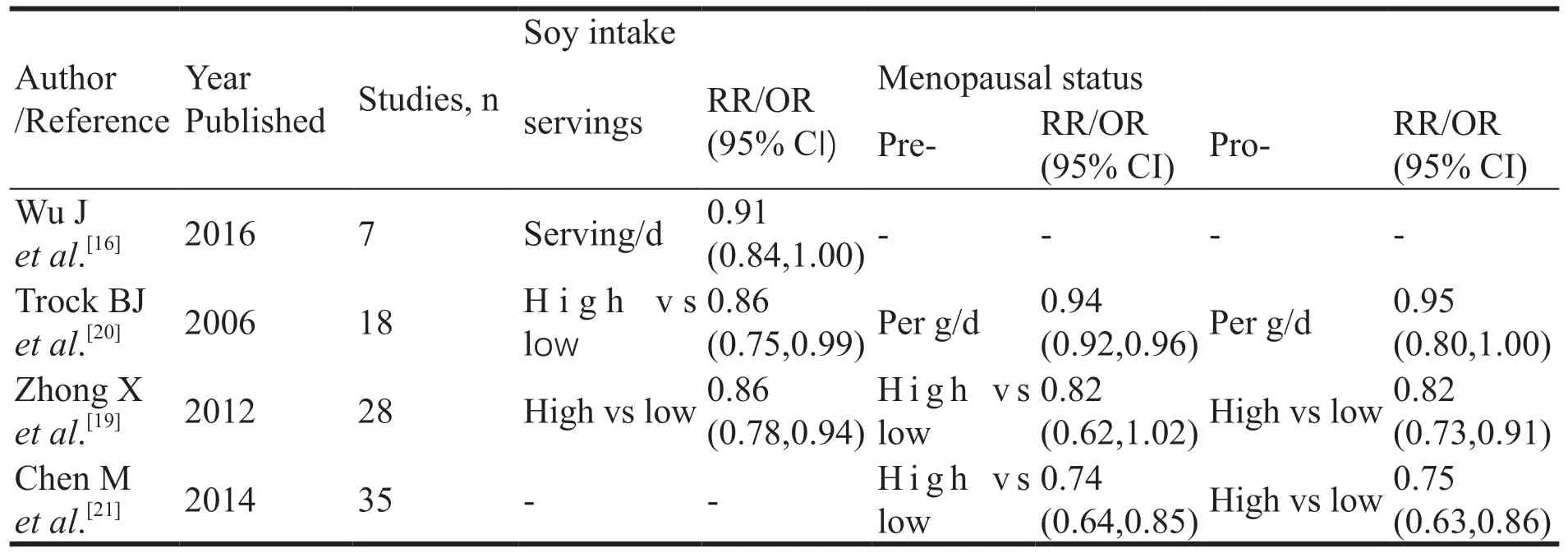
Table 2 Risk estimated from meta-analysis of the associations between soy intake and breast cancer incidence
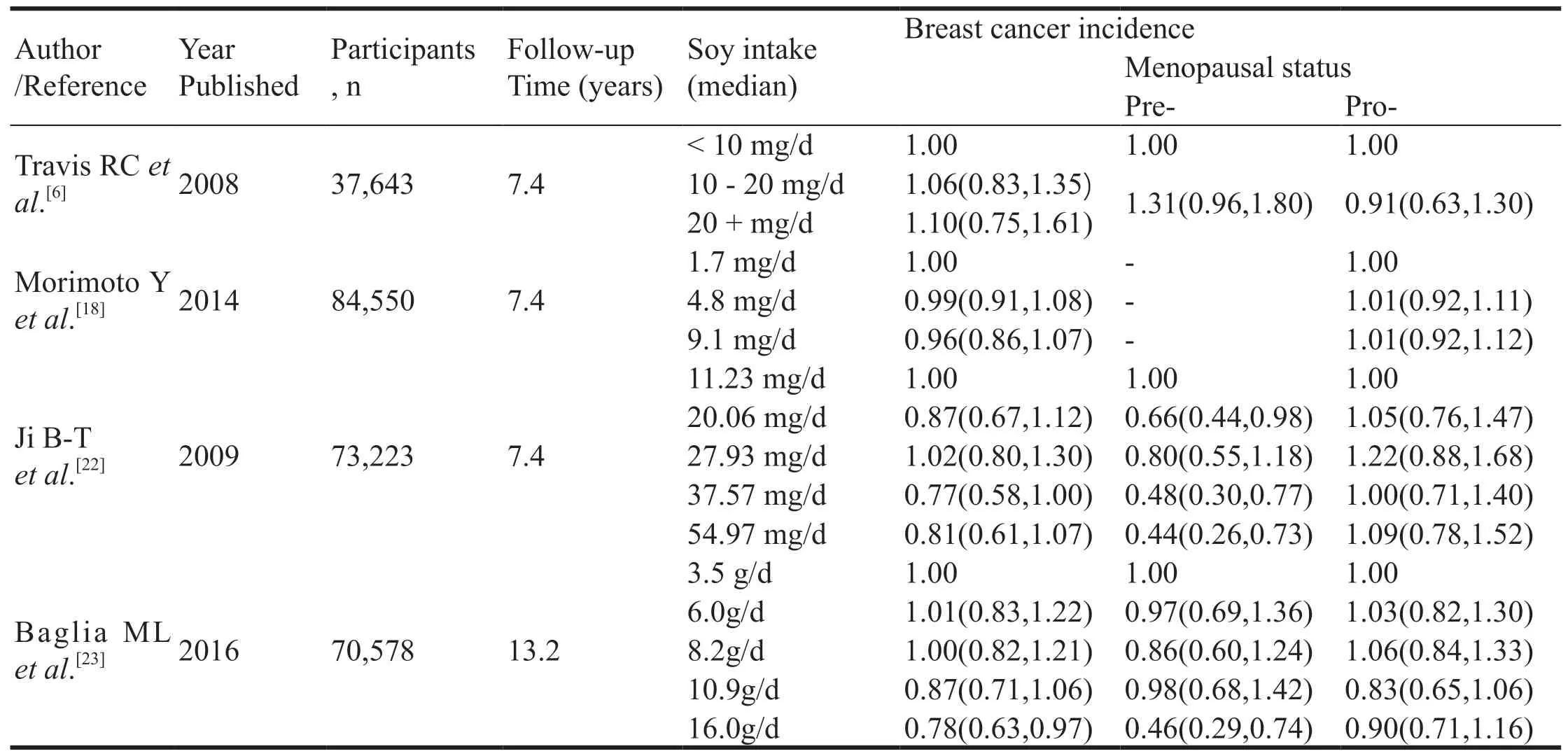
Table 3 Risk estimated from cohort studies of the associations between soy intake and breast cancer incidence
In conclusion,dietary isoflavones seems to be unlikely to have a negative impact on the occurrence and development of breast cancer.The positive effect can be modified by subtypes of breast cancer,menopausal status,therapies and the duration,quantities and frequencies of soy exposure.So it’s rational for health professionals to recommend young women consume soy products though the details of soy recommendation have not reach a consensus.The potential benefits on prognosis indicate that making a proper post-diagnosis dietary adjustment is an important part of cancer therapy.Some limitations must be considered when interpreting above-mentioned studies,such as the recall bias,the sample sizes,the measurement standard and so on.Besides,the lifestyle may also be a confounding factor while high consumption of soy is on behalf of healthy lifestyles in most cases.
Red and processed meat
In recent years,the dietary pattern has been shifted to a high energy-dense diet,which is characterized by higher consumption of red and processed meat.Red and processed meat consumption has long been considered beneficial to health due to its nutritional composition,whereas the potential adverse health effects have attracted worldwide attention.In 2015,based on more than 800 epidemiological studies,The International Agency for Research on Cancer (IARC)classified consumption of processed meat as“carcinogenic to humans”(Group1)and red meat as“probably carcinogenic to humans”(Group 2A)[40].
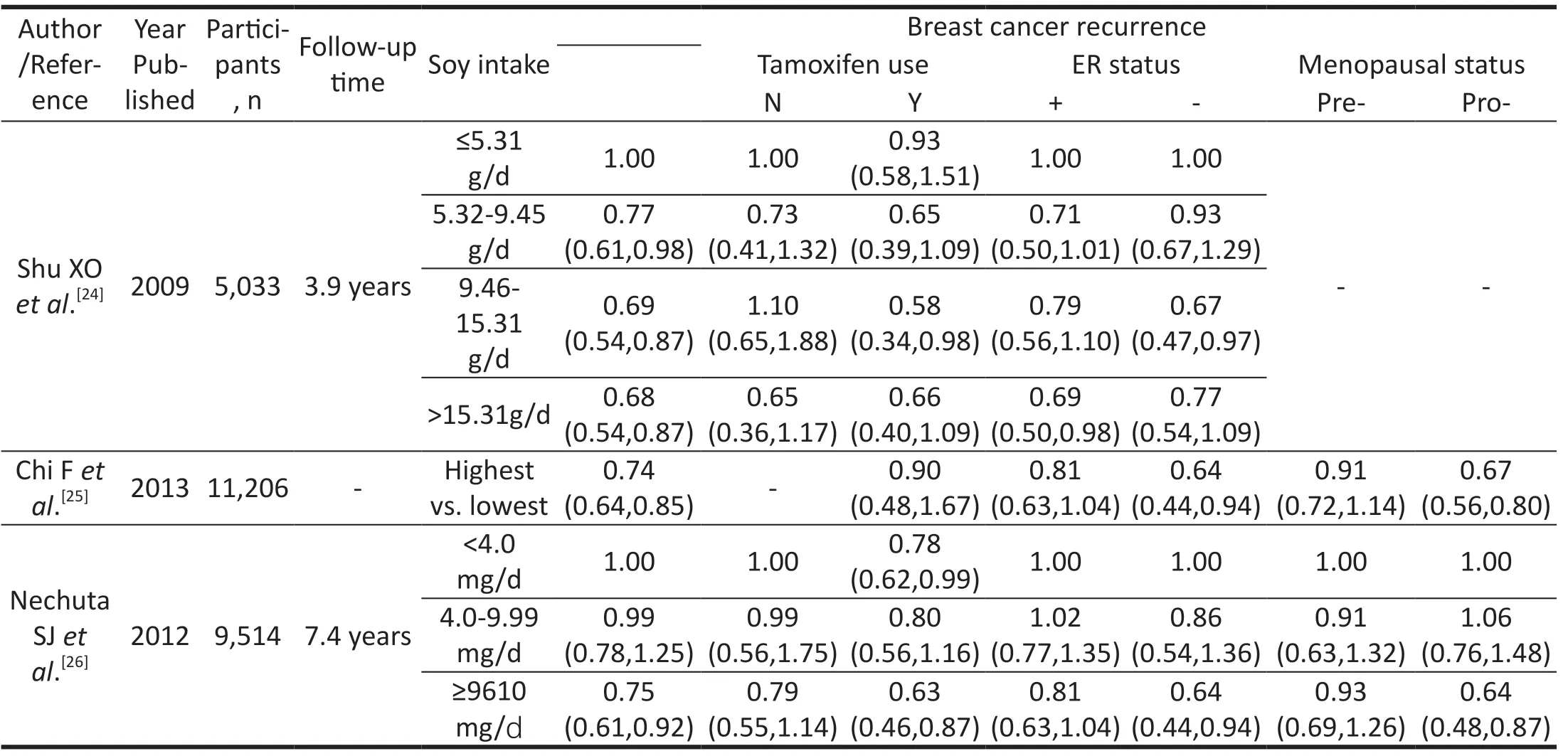
Table 4 Risk estimated from studies of the associations between soy intake and breast cancer recurrence

However,the exact relationship between red and processed meat and breast cancer remains controversial.Genkinger JMet al.[4]found no associations between meat-eating diet and the risk of breast cancer in the Black Women’s Health Study which was a large prospective cohort study.In contrast,Maryam S Farvidet al.[41]found that the greater intake of red meat during adolescence significantly increased the premenopausal breast cancer risk which might be decreased by replacing red meat with other protein sources such as poultry,fish and so on,based on the Nurse’s Health Study II cohort.When considering the adult diet,a similar result that a diet pat-tern rich in red meat could augment the incidence of the breast cancer was shown by a meta-analysis [16].Unlike the conclusions mentioned above,Camille Pouchieuet al.[42]found that it was processed meat rather than red meat that was involved in the occurrence of breast cancer.They also found that the association could be counteracted by dietary antioxidants supplements.The importance of processed meat-eating frequency was mentioned when taking the relevance between meat consumption and breast cancer risk into account.Niki Mouroutiet al.[43]emphasized that only daily processed meat intake added the odds of breast cancer.A recent meta-analysis conducted by Jana J.Andersonet al.[44]reported similar findings to the above studies.They found that red meat was independent of breast cancer while the pooled RR for processed meat and post-menopausal breast cancer was 1.09 (95% CI:1.03-1.15).In another cohort study,it was shown that both red meat and processed meat might promote the development of postmenopausal breast cancer.Besides,they found that red meat consumption was prone to induce regional or distant cancer and processed meat was related to localized cancer [45].Interestingly,the methods and degrees of cooking also have an impact on breast cancer risk.Elena Boldoet al.[46]reported that well-done and stewed red meat enhanced the breast cancer risk,especially for HR+tumors and so did pan-fried/bread-coated fried white meat,especially for pre-menopausal breast cancer.It’s plausible to conclude that high consumption of red and processed meat has a negative impact on breast cancer risk.
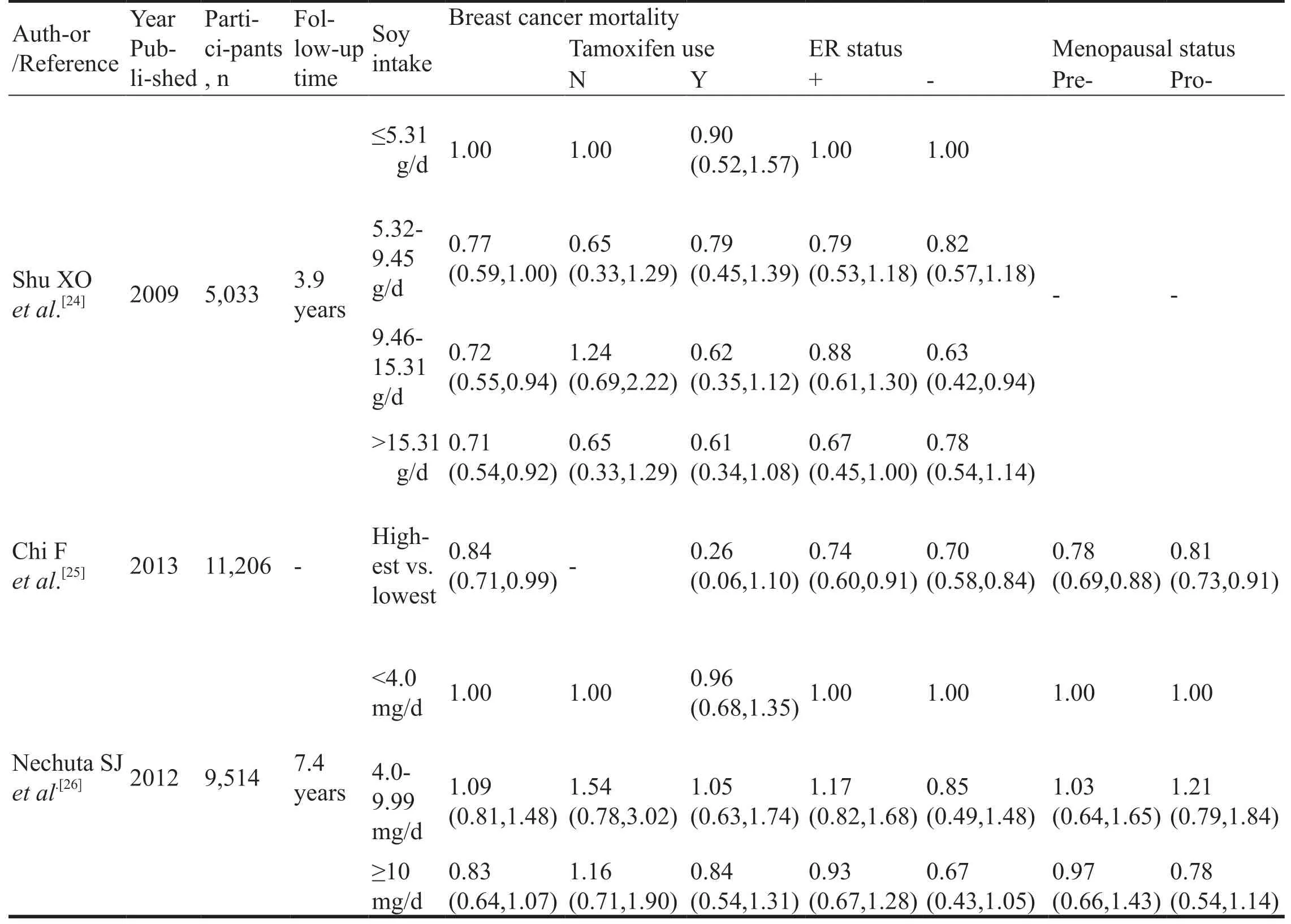
Table 5 Risk estimated from studies of the associations between soy intake and breast cancer mortality
The possible mechanisms of the above associations are listed as follows.Firstly,red meat is rich in amines,nitrate and nitrite,which can convert to N-nitroso-compounds.Hebels DGet al.[47]have shown that exposure to NOCs can induce apoptosis,cell cycle blockage,DNA repair and oxidative stress,which are involved in the tumor progression.Secondly,heme iron,another component of red meat,can promote hyper-proliferation and hyperplasia of colon cells by down-regulating proliferation inhibitors[48],though there is no significantly association between heme iron and breast cancer.Thirdly,non-human sialic acid N-glycolylneuraminic acid (Neu5Gc),which specifically consists in red meat,could cause systemic inflammatory response related to carcinogenesis when interacting with its specific antibody [49].Fourthly,when cooking at high temperatures or for long time,red meat can produce heterocyclic amines (HCAs)[50],which has been shown its carcinogenicity in animal models [51]and its positive association with breast cancer in an epidemiological study[52].Besides,HCAs is abundant in 2-amino-1-methyl-6-phenylimidazo [4,5-b]pyridine (PhIP),which is demonstrated that PhIP can suppress the miRNA expression via activating oestrogen receptor alpha in MCF-7 cell lines [53],while the deregulation of miRNA can promote breast cancer development and metastasis [54].Last but not the least,it’s thought that the high content salt and fat and residual harmful feed composition may make an contribution to the tumorigenesis although the exact mechanism needs to be further explored [49].
Sulforaphane
Cruciferous vegetables,like broccoli,brussels sprouts,cabbage,cauliflower,collard and so on,are abundant in sulforaphane and have been brought to the forefront since their anti-breast cancer potentials were reported in Deborah A.Boggset al.[55]‘s cohort study.They found an inverse association between cruciferous vegetables intake and breast cancer incidence (Ptrend=0.06)and it was stronger in premenopausal women after a median follow-up of 12years among 51,928 women enrolled in the Black women’s health study.Consistently,Ambrosone CBet al.[56]reported a marginally significant reduced risk of post-menopausal breast cancer for broccoli intake.Conversely,based on eleven case-control and two cohort studies,Liu,Xet al.[7]found that higher cruciferous consumption could reduce the breast cancer risk by 15% and such an significant risk reduction was only observed in postmenopausal women.Farvid MSet al.[57]reported higher consumption of cruciferous vegetables,particularly broccoli,cabbage and cauliflower,was related to lower breast cancer incidence though the impact of menopausal status was not further studied.
It’s accepted that sulforaphane (SF)makes a great contribution to the tumor-protective effect.Ming Yanget al.[58]found that in triple negative breast cancer cell(TNBC)lines treated with SF such as MDA-MB-453 cells and MDA-MB-436 cells,cell proliferation was inhibited which was attributed to the incremental number of G2/M-arrested and apoptotic cells.At the same time,the expression of cyclinB1,Cdc2 and Cdc25 was reduced and that of Egr-1 was significantly increased in those changed cells.They also found that up-regulated level of Egr-1 induced down-regulation of cyclinB1,Cdc2 and Cdc25 followed by the accelerated cell proliferation.
Thus,SF can restrain cell growth through the Egr 1-cyclinB 1-cdc2 pathway.Similarly,Anna Lewinskaet al.[59]found that the effects of SF on human breast cancer cell lines including MCF-7,MDA-MB-231 and SK-BR-3 were dose-dependent.Low concentration of SF caused cell cycle arrest and senescence while high dose induced cell apoptosis.The cytostatic effect of SF involved multiple mechanisms,including the generation of nitric oxide,the inactivation of AKT signaling which played a pivotal role in cell growth,survival and metastasis,the epigenetic changes such as microRNAs profile,and the global DNA demethylation as well as the suppression of m6A RNA methylation.In MDA-MB-231,BT-549 and MDA-MB-468 cells,SF enhanced the formation of autophagosome which could be prohibited by the autophagy inhibitor 3-Methyladenine.It was connected with the decreased level of histone deacetyalse 6 and the activation of phosphatase and tensin homolog(PTEN)[60].SF can also promote paclitaxel-treated breast cancer cells to apoptosis via reducing the activity of NF-κB signaling pathway and the expression of Bcl-2 which is an anti-apoptotic protein,and inhibiting the phosphorylation of AKT [61].Cancer stem cells (CSCs)are suggested to be crucial to tumor dormancy and relapse because conventional tumor therapies have little impacts on those cells.It is encouraging to find that SF may have a potential role of targeting CSCs.SF declined the number and size of mammospheres and aldehyde dehydrogenase(ALDH)positive cells in MCF7 and SUM159 human breast cancer cell lines.Cancer cells abundant in mammospheres and high ALDH activities were considered to be self-renewal.These effects were followed by the diminished level of β-catenin and cyclin D1,which implicated that SF eliminated CSCs via inhibiting Wnt/β-catenin pathway [62].Analogically,the rise of ALDH+cells and mammospheres caused by taxane was reversed by SF in an attempt against TNBC via the combination taxane with SF.There was also a suppression in the activation of NF-κB signaling which was essential for CSCs regulation and in the secretion of IL-6 and IL-8 which can directly promote CSCs expansion in SF treated cell lines [63].Nadia P.Castroet al.[64]reported similar SF-mediated effects on CSCs.After SF treatment,there was a reduced expression of CR1 and CR3 which were embryonic genes to encode proteins,Cripto-1 and Cripto-3,respectively.CR1 and CR3 can act with growth differentiation factor-1/3 (GDF1/3),G-protein coupled receptor 78 (GRP78),activin receptor type-1B (ACVR1B)and other molecules of TGF-β family related to mediate Smad-dependent signaling.SF also inhibited the interaction of CR1,GPR78 and ACVR1B,which might be responsible for SF-induced reduction of CSCs.SF inhibited Hh (Hedgehog)/Gli1(glioma-associated oncogene homologue)signaling by decreasing the Gli level and suppressed the expression of matrix metalloproteinases 2 and 9 (MMP-2 and MMP-9)in SUM159 human breast cancer cells,in which Hh/Gli signaling regulated the MMP-2 and MMP-9 expression and both of them were involved in tumor cell invasion and migration.This finding implicated that SF suppressed tumor metastasis by regulating Hh/Gli signaling [65].In addition,Qinglin Liet al.[66]found SF disrupted the communication between tumor cells and the microenvironment by inhibiting the production of adipocyte differentiated from mesenchymal stem cells,thus reducing breast cancer cell invasion and migration.
Conclusion
In summary,the association between dietary factors and breast cancer haven’t come to a unanimous conclusion.Soy at least was harmless and most of time was protective.Red and processed meat was at least profitless.Sulforaphane seemed to be promising in the prevention and treatment of breast cancer.Due to the heterogeneity of breast cancer,the menopausal and estrogen receptor statuses may be modified factors in diet-cancer association.In brief,it may be reasonable to recommend breast cancer patients to eat high soy foods and cruciferous vegetables and low red and processed meat.
- Food and Health的其它文章
- Nutritional support strategies for cancer cachexia
- The therapeutic mechanism of black soybean in atherosclerosis based on network pharmacology
- The problems of nutritional support for head and neck malignant tumor patients undergoing radiotherapy
- Study on the mechanism of Coix seed in the treatment of colon cancer Based on network pharmacology