Factors associated with visit-to-visit variability of blood pressure in hypertensive patients at a Primary Health Care Service, Tabanan,Bali, Indonesia
Gusti Ayu Riska Pertiwi , Anak Agung Ngurah Aryawangsa , I Putu Yuda Prabawa , Ida Bagus Amertha Putra Manuaba ,Agha Bhargah , Ni Wayan Sri Ratni , I Putu Gede Budiana
1. Faculty of Medicine, Udayana University, P.B. Sudirman Street, Dangin Puri Klod, West Denpasar, Denpasar City, Bali 80232, Indonesia
2. Biomedicine Magister Program,Post Graduate Program, Faculty of Medicine, Udayana University,P.B. Sudirman Street, Dangin Puri Klod, West Denpasar, Denpasar City, Bali 80232, Indonesia
3. Medical and Health Education, Faculty of Medicine, Udayana University, P.B. Sudirman Street, Dangin Puri Klod, West Denpasar, Denpasar City, Bali 80232, Indonesia
4. International Program in Medicine, College of Medicine, Taipei Medical University, No. 250,Wuxing Street, Xinyi District,Taipei City 110, Taiwan, China
5. Tabanan III Primary Health Care Service, Bali, Indonesia
6. Department of Cardiovascular Medicine, Mangusada General Hospital, Badung, Bali, Indonesia
Abstract Background: An increasing number of valid and well-designed trials have demonstrated a positive correlation between visit-to-visit variability (VVV) in systolic blood pressure (SBP) and increased risk of stroke and coronary heart disease among hypertensive patients.Methods: A cross-sectional study was conducted that involved 74 patients who visited the outpatient clinic at the Tabanan III Primary Health Care Service during April to May 2017. Blood pressure was retrospectively obtained from medical records. VVV was classif ied as low or high on the basis of the standard deviation of SBP. Antihypertensive medication adherence was expressed as the percentage of days covered, and sodium intake was measured with 24-hour food recall. Bivariate analysis was performed, followed by multivariate analysis for signif icant variables.Results: Among the participants, 67.6% were female, with a mean (standard deviation [SD])age of 62.70 (10.00) years. Blood pressure was measured 4.82 ± 0.78 times during the period, and the mean (SD) SBP was 139.65 (10.57) mm Hg. Nonadherence and sodium intake were signif icantly higher in the high-VVV group than in the low-VVV group (nonadherence 13.5% vs. 37.8%,P = 0.033; sodium intake 1278.44 ± 43.02 mg vs. 1495.85 ± 45.26 mg, P = 0.038). After adjustment for other covariates, the differences remained signif icant only for nonadherence (model I exp β = 3.89 [95.0% conf idence interval 1.23— 12.34, P < 0.05], model II exp β = 3.9 [95.0% conf idence interval 1.12— 14.15, P < 0.05]). The area under the curve was 0.636 ( P < 0.05), with sensitivity of 67.6% and specif icity of 51.4%.Conclusion: Nonadherence to antihypertensive medication was signif icantly associated with higher VVV of SBP. Further study is needed to assess whether improving adherence could reduce VVV and improve cardiovascular outcomes.
Keywords: Blood pressure; visit-to-visit-variability; nonadherence; sodium intake; hypertension
Introduction
Hypertension is generally accepted as one of the key modif iable risk factors for the development of cardiovascular diseases and cerebrovascular events [ 1— 3]. Over the past 25 years,the growing aging population and some behavioral risk factors(e.g., unhealthy diet, physical inactivity, excess body weight,persistent stress) have inevitably contributed to a signif icant increase in the rate of elevated systolic blood pressure (SBP)and disability and deaths related to it. Thus hypertension is becoming a very important global health issue [ 2, 3].
Blood pressure (BP) inherently exhibits an array of spontaneous oscillations that can be seen as a neurohormonal adaptive response to internal and external stimuli. This f luctuation, known as BP variability (BPV), can happen in a short period (beat to beat, within 24 hours) or a long period (months,between visits) [ 4, 5]. Several clinical studies have recently suggested that higher short-term BPV, as measured by 24-hour ambulatory BP monitoring (ABPM), or long-term BPV, as measured by visit-to-visit variability (VVV), predicts poor prognosis not only for major cardiovascular events but also for other medical events [ 6, 7]. These include stroke [ 8], cognitive impairment [ 9], worsening renal function in a patient with or without chronic kidney disease [ 10— 12], and development of microvascular complication in diabetes mellitus patients [ 13],independent of the average BP. Equally signif icant, apparently only studies on VVV have been done on the large scale of clinical trials, thus providing a stronger level of evidence than for ABPM [ 4, 14]. Moreover, head-to-head comparison between VVV and ABPM variability demonstrated that VVV might be a stronger prognostic predictor than ambulatory BPV in hypertensive patient. VVV could also provide more comprehensive information regarding long-term and ultra-long-term outcome in hypertensive patients [ 5, 15].
Although there are few discordant subsets of data regarding the prognostic relevance of each BPV measurement, it can be proposed that minimizing BPV may help to provide better cardiovascular protection in hypertensive patients. To achieve this goal, a more comprehensive measure should be used to overcome contributing factors. Unfortunately,data on factors responsible for the BPV observed between visits are very scarce and limited in the literature. A large observational randomized trial, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial(ALLHAT), assessed the relationship between antihypertensive medication nonadherence and VVV and found a positive correlation [ 16]. Unfortunately, several risk factors that are assumed to correlate with hypertension, such as obesity,sodium intake, and levels of physical activity, remain unexplored. Only a paucity of evidence is available to explain the relationship between the factors mentioned above and BPV[ 17— 19]. Considering sodium intake as an independent risk factor for VVV is unsatisfactory because of inconsistent f indings [ 18, 19]. In one study that monitored ambulatory BP and physical activity in 431 patients, there was a signif icant association between physical activity and BPV, although this relationship is weak [ 20].
In the current study, we tried to explore factors affecting VVV in the real-world hypertensive population in a primary health care service setting. The primary health care service as the f irst gatekeeper in handling patients has a pivotal role in identifying modif iable risk factors for VVV of BP in hypertensive patients at the primary health care level. Hence concern for risk factor identif ication will provide an important benef it regarding the setting of health policy and prevention measures.For the reasons mentioned above, this study aimed to determine the factors associated with the VVV in BP at a primary health care service.
Methods
Study participants
Seventy-four hypertensive patients admitted to the outpatient clinic of the Tabanan III Primary Health Care Center,Tabanan, Bali, Indonesia, for evaluation and management of hypertension were enrolled in this study during April to May 2017. Hypertension was diagnosed on the basis of clinical measurements of SBP of 140 mm Hg or greater and/or diastolic BP (DBP) of 90 mm Hg or greater at a minimum of two different visits or if the patient was currently taking medication to control hypertension [ 21]. The patients’ BP records over a 4-month period (January to April 2017) were retrieved, and those having fewer than three BP measurements from three different visits before data collection were excluded.
This study was evaluated and approved by the Ethics Committee, Faculty of Medicine, Udayana University, Bali,Indonesia. Informed consent was obtained from all eligible participants who could provide informed consent.
Data collection
BP measurement, VVV of BP, and BP control:Data regarding BP were retrospectively retrieved from medical records. BP was measured in off ice-based settings with an interval of 1— 4 weeks by professional nurses with the conventional cuff method using a mercury sphygmomanometer(Nova-Presameter, Riester, Germany). In this study we used the standard deviation (SD) of BP from three to six visits as the main metric for VVV of SBP regardless of there being many other metrics available (coeff icient of correlation, average real variability, SD independent of the mean [SDIM]) as studies found them to be equally signif icant. The SD of SBP was then classif ied into two groups by means of a cutoff point at the 50th percentile: values below the 50th percentile are def ined as low variability of SBP and values equal to or greater than the 50 percentile are def ined as high variability of SBP.
Covariates:Adherence to antihypertensive medication therapy was assessed through the percentage of days covered(PDC) at each visit. In this formula, the number of days the patient took the medication during a prescribed period (numbers of days in period “ covered”) is divided by the number of days in the prescribed period, and then multiplied by 100.0%.Besides checking the pharmacy administrative database, we also asked directly whether participants had already taken their antihypertensive medications or not, to ensure the total number of days covered with medication was correct. Participants with PDC of less than 80.0% on at least one visit during the observation period were categorized as nonadherent ( < 96 days taking medication during 120 days of the prescribed period)[ 16]. Amlodipine and captopril were the medications used by the patients in this study.
Data on sodium intake were obtained through 24-hour food recall questions, the answers to which were analyzed with NutriSurvey 2007. These questions help in obtaining detailed information on all food, beverages, and dietary supplements taken by participants during the previous 24 hours, and questioning was done on two nonconsecutive days to estimate the participant’ s mean usual dietary sodium intake.
Other potential variables that might affect VVV, including demographic, socioeconomic, and behavioral-related variables (smoking status, physical activity), comorbidity,and anthropometric data (height, weight, waist circumference, body mass index) were also analyzed. Smoking status was determined on the basis of smoking behavior currently and within the past year. The level of physical activity was categorized as sedentary, mild, or moderate according to the Centers for Disease Control and Prevention and American College of Sports Medicine 1999 guideline. Body mass index was calculated as weight (kg) divided by height squared (m2) [ 22].
Statistical analysis
All statistical analyses were performed with IBM SPSS Statistics version 19. Participants’ characteristics, adherence to antihypertensive medication, sodium intake, and covariates were compared among the group with low VVV of SBP and the group with high VVV of SBP. Data were expressed as a percentage, mean ± SD, or median (and range). Bivariate analysis using the chi-square test for dichotomous variables and the t test (parametric) and Mann-Whitney U test (nonparametric) was used to determine statistically signif icant differences between variables. All signif icant variables in the bivariate regression test were included in the multivariate regression test. Multivariable analysis was performed to calculate the β coeff icient (standard error) and adjusted exp β (odds ratio [OR], 95.0% conf idence interval [CI]). Ultimately, the accuracy of the f inal signif icant variable was tested by receiver operating curve (ROC) analysis. We set P < 0.05 as statistically signif icant.
Results
Baseline characteristics
Most of the participants were female (67.6%), and the mean (SD) age was 61.57 (9.82) years (range 45— 81 years).The SBP and DBP were 139.65 ± 10.57 mm Hg and 84.52 ± 6.10 mm Hg, respectively, and were obtained from 4.82 ± 0.78 measurements (range 3— 7). The SD range of SBP was 5.77— 23.09 mm Hg, and a median value of 10 mm Hg was used as a cutoff point to further classify participants into two groups; the group with low VVV of SBP and the group with high VVV of SBP. The sodium intake per day, waist circumference, PDC, and body mass index were as follows:1387.14 ± 451.98 mg/day, 84.81 ± 8.41 cm, 99.82 ± 15.81 days,and 25.49 ± 4.07 kg/m2, respectively. Only 16.2% patients had concurrent comorbidities ( Table 1). Most of the participants were uneducated (58.1%), had mild activity level (67.6%),adhered to medication (74.3%), were married (89.2%), and had no smoking history (85.1%) ( Table 1).
The characteristics of the patients in each study group are summarized in Table 2. The demographics, socioeconomic status, comorbidities, level of physical activity, smoking status,types of antihypertensive being used, and body mass index did not differ signif icantly between the low-VVV group and the high-VVV group. Poor adherence to the prescribed antihypertensive medications was more common in the high-VVV group than in the low-VVV group ( P = 0.030). Participants in the high-VVV group also tended to have higher mean dietary sodium intake than those in the low-VVV group ( P = 0.038)( Table 2).
Multivariable analysis
The associations between study variables and VVV of SBP were further analyzed in a multivariate regression logistic test, and signif icance was found only for nonadherence to antihypertensive medications ( P = 0.023). In multivariate model I, after adjustment for nonmodif iable covariates such as age and sex, nonadherence was signif icantly associated with high VVV of SBP (OR 3.89, 95.0% CI 1.23— 12.34,P = 0.021) ( Table 3). This result remained signif icant in full multivariable analysis (model II), which found that nonadherent patients had four times higher risk of having SD of SBP variability greater than 10 mm Hg (OR 4.22, 95.0% CI 1.22—14.64, P = 0.023) ( Table 4). However, the area under the curve(AUC) in ROC analysis was 0.636 (95.0% CI 0.508— 0.763,P = 0.044) ( Fig. 1), which indicated that it had signif icantly weak discriminatory power to predict high BPV accurately.The sensitivity and specif icity of this measurement were 67.6% and 51.4%, respectively.
Discussion
VVV of BP was identif ied as an important independent risk factor for cardiovascular events and death in several studies.However, recent studies still have a paucity of data regarding factors associated with VVV of BP. This study considered factors related to BPV between visits as measured by off ice BP inhypertensive patients in a primary health care setting. The participants were essential hypertensive patients without apparent cardiovascular-related adverse complications, which makes this study suitable for analyzing the interaction between variables of interest and BPV at an earlier state of hypertension progression. The relatively low levels of concurrent noncardiac comorbidities in the participants (only 16.2% had at least one comorbidity) mean that the results could be specif ically attributed to hypertension itself.
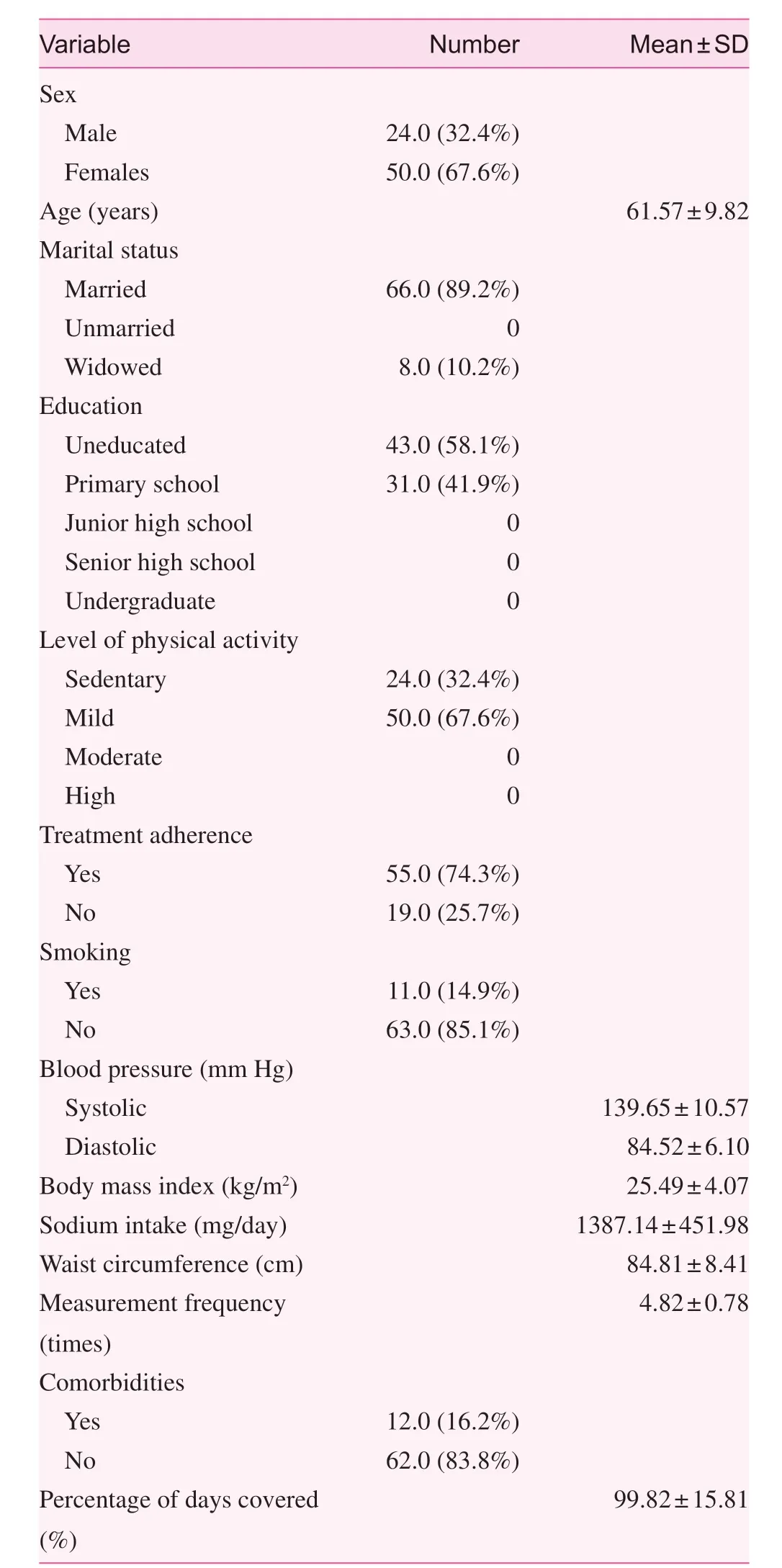
Table 1. Demographic characteristics of participants at the Tabanan III Primary Health Care Service
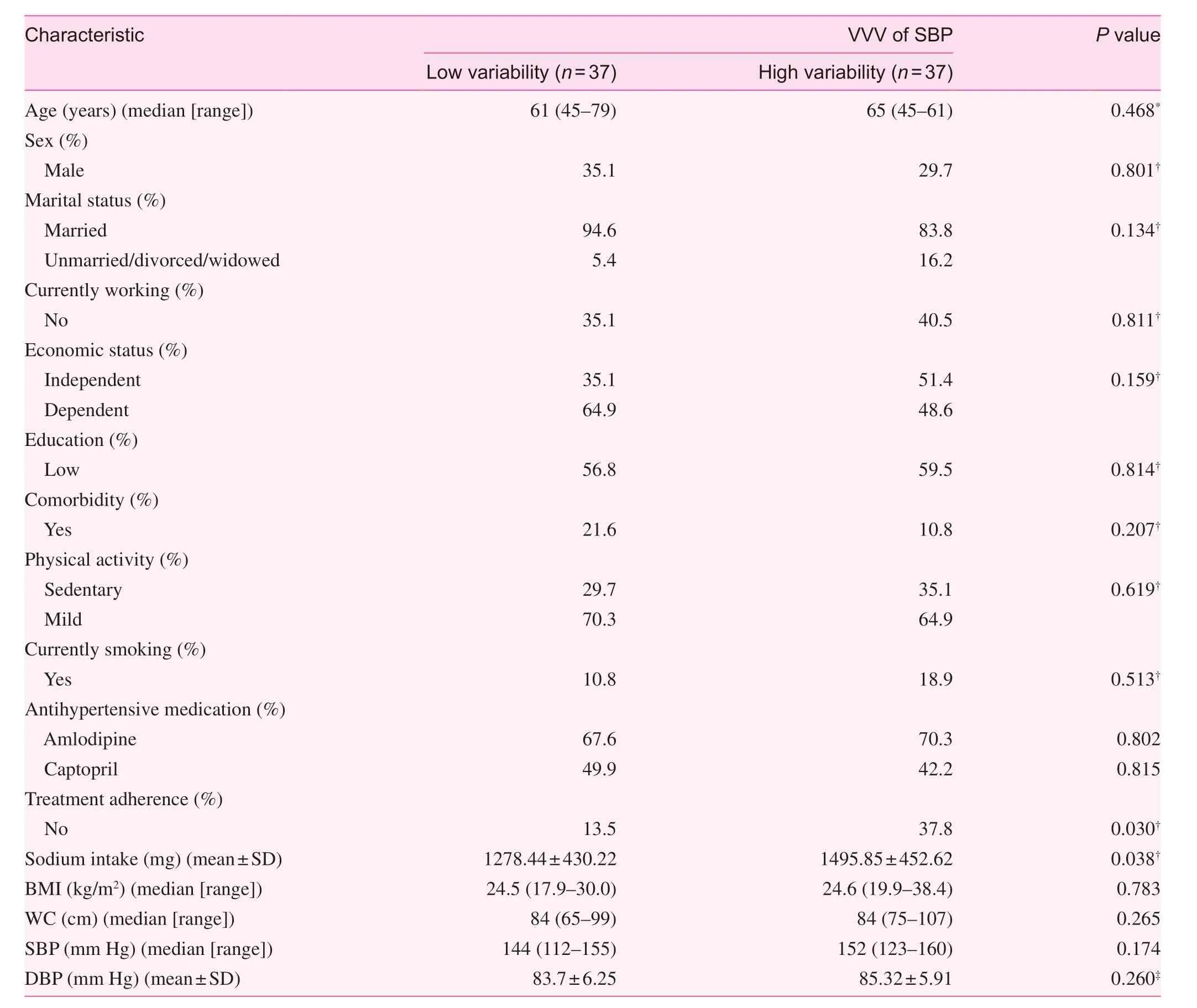
Table 2. Characteristics of participants based on the level of visit-to-visit variability (VVV) of systolic blood pressure (SBP)
The results of the present study results show that nonadherence to antihypertensive medication was independently associated with higher SBP variability between visits incomparison with strict adherence to medication, and this remained signif icant after multivariate adjustment. A similar f inding was obtained by Kronish et al. [ 16], who analyzed the ALLHAT population and used SDIM as their primary BPV index, and adherence was self-reported with guidance from the Adherence Survival Kit. After adjustment in multivariable analysis, nonadherent participants demonstrated 0.8 higher SDIM of SBP than adherent participants (95.0% CI 0.7— 1.0,P < 0.001). This result was similar for individuals who later changed to nonadherent from adherent (0.9; 95.0% CI 0.5—1.3, P < 0.001), while those who became adherent conversely showed a 0.7 decrease in SDIM of SBP (95.0% CI - 1.0 to- 0.3, P < 0.001) [ 16, 23]. Two studies that recruited a considerable number of participants, the African American Study of Kidney Disease and Hypertension (AASK) ( n = 988) [ 24] and a study that used data from the Cohort Study of Medication Adherence among Older Adults (CoSMO) ( n = 1391) [ 25],used pill count or pharmacy pill rates to def ine adherence into several categories. Both studies reported a linear association between poorer adherence and higher levels of variability.As a summary of these f indings, despite the low accuracy of the nonadherence predictive model in the current study(AUC < 0.7), addressing the level of adherence as a goal in a patient’ s therapeutic planning in addition to the conventional mean absolute BP at each visit will probably result in improvement of long-term outcomes in hypertensive patients.
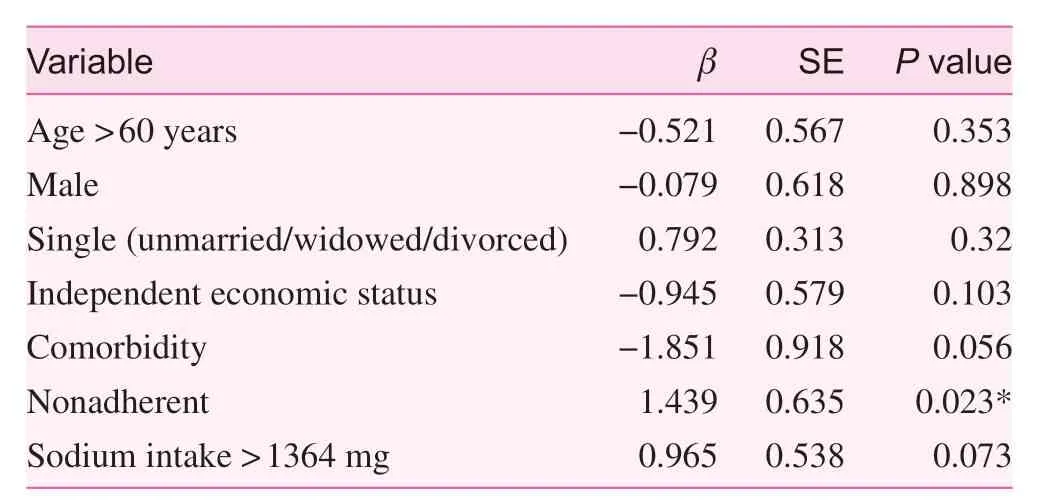
Table 3. Multivariate logistic regression results of study variables for high visit-to visit variability patients
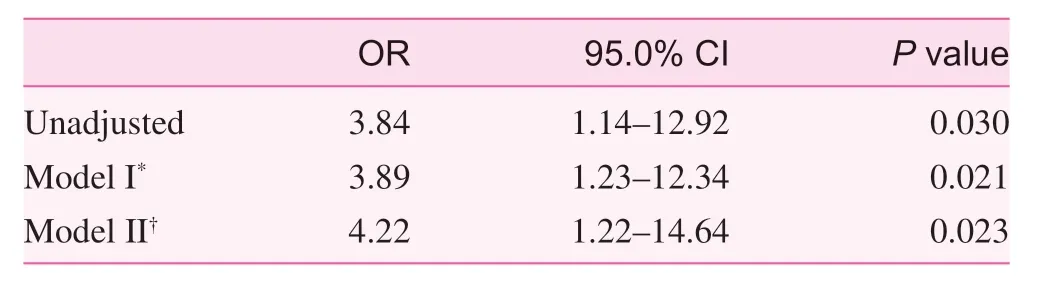
Table 4. Odds ratios of adherence status for high visit-to-visit variability patients
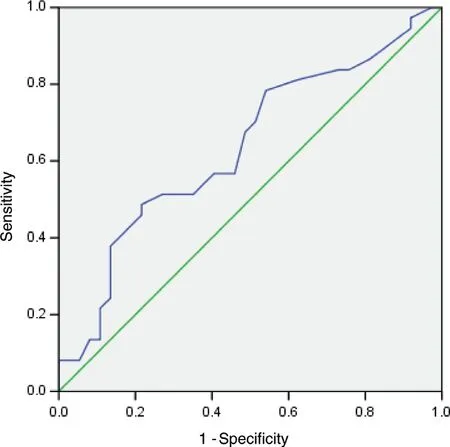
Fig. 1. Area under the curve of the receiver operating characteristic between nonadherence to medication (based on percentage of days covered) and high variability of blood pressure.
One hypothesis proposed that the pharmacological actions of antihypertensive drugs being used may explain the associations observed between adherence and VVV. Some demonstrated superior action of calcium channel blockers (amlodipine)to reduce BPV [ 26— 29]. The Anglo-Scandinavian Cardiac Outcomes Trial — Blood Pressure Lowering Arm (ASCOTBPLA) involving 19,257 high-BP patients revealed that the group taking amlodipine with or without perindopril had lower BPV between visits than the group taking atenolol with or without bendrof lumethiazide. The effect on VVV further contributed to the risk reduction of stroke and coronary events in the aforementioned group [ 26]. Head-to-head comparison between amlodipine and other drugs (atenolol, lisinopril, chlorthalidone, and losartan) demonstrated a treatment difference of - 1.23 mm Hg (0.46, P = 0.008) by SD and - 0.86 mm Hg(0.31, P = 0.005) by coeff icient of variation [ 29]. However, in ALLHAT, no signif icant effect of medication classes on the nonadherence— high variability relationship was observed [ 16].In our study, we found that the association between nonadherence and VVV was independent of the medication type used.Accordingly, these results provide a perspective on the complexity of the BPV and adherence relationship.
Other remaining covariates, such as demographic, socioeconomic, and behavioral-related factors, comorbidities, and anthropometrics, did not affect VVV. For intake of sodium,despite its well-known role in hypertension and established evidence that sodium restriction leads to substantial BP reduction [ 30], its association with VVV is still unclear. The present study found differences in sodium intake between each VVV group only when sodium intake was categorized as a continuous variable, whereas the association was no longer signif icant in categorical grouping and multivariate study. A study conducted by Diaz et al. [ 18] that recruited adequate numbers of individuals with high-normal DBP suggested that successful dietary sodium reduction during the study period(6 months) was not associated with decreased VVV of SBP with or without body weight reduction. Nevertheless, sodium intake regulation remains important in hypertension therapy,and it is imprudent not to consider it in deciding on the patient’ s management planning. Here we found the mean dietary sodium intake in both VVV groups was surprisingly below the recommendation from the World Health Organization( < 2 g of sodium per day or < 5 g of salt per day) and even far behind Asian population sodium intakes ( > 4.6 g/day).Our f inding is similar to that of a study by Kamso et al. [ 31]in 2007 that involved a similar age group from samples of the Indonesian population (age 55— 80 years), but they found inadequate mean sodium intakes of 0.20 ± 0.02 g/day in males and 0.16 ± 0.02 g/day in females.
Study limitations
Several limitations may hinder the interpretation of our study f indings. First, the total number of samples was rather small,making it impossible to classify BPV into more than two groups as in most prior studies, and thus this may mask actual association attributed to midclassif ication groups. Second, BP was retrospectively extracted from patients’ medical records;there is a possibility that measurements were not conducted following a standard protocol in some cases. Third, quantif ication of dietary sodium intakes using 24-hour food recall questions possess some limitations related to patient recall and some patients may underreport/overreport their diet. Fourth,there was a substantial difference in patient total visits and the time between visits, which could affect the SD of VVV observed in the population. Although there is no gold standard for the minimal number of visits needed to assess VVV, too few or too many total visits will inevitably correlate with VVV especially when expressed as SD of BP. Fifth, the current f indings of VVV predict morbidity outcome only with a low level of evidence because of the predictive model (AUC < 0.7), and therefore we suggest VVV can be used only to support diagnostic evidence.
Conclusion
Nonadherence to antihypertensive medication is associated with higher VVV of SBP. VVV of BP has emerged as a supporting indicator in predicting morbidity and is diagnostic in hypertensive patients, and specif ic intervention targeting factors that affect variability is mandatory. Hence more studies are needed to evaluate the dynamic mechanisms underlying the associations between adherence and VVV, and whether improving factors related to VVV will also improve outcomes.
Conf lict of interest
The authors declare no conf lict of interest.
Funding
This research received no specif ic grant from any funding agency in the public, commercial, or not-for-prof it sectors.
Author contributions
Gusti Ayu Riska Pertiwi was responsible for data gathering and the methodological concept. Anak Agung Arya Wangsa was responsible for manuscript formation and f inal proofreading. I Putu Yuda Prabawa and Agha Bhargah were responsible for statistical analysis. Ida Bagus Amertha Putra Manuaba was responsible for revision of the manuscript and the methodological concept. Ni Wayan Sri Ratni, as an expert in community health in primary health care, and I Putu Gede Budiana, as an expert in cardiology, provided guidance on the preparation of the manuscript.
 Family Medicine and Community Health2018年4期
Family Medicine and Community Health2018年4期
- Family Medicine and Community Health的其它文章
- Effi ciency of community health centers in China during 2013– 2015:A synchronic and diachronic study*
- Nutritional status in adolescent girls: Atte mpt to determine its prevalence and its association with sociodemographic variables
- Predictors of successfully quitting smoking among smokers registered at the quit smoking clinic at a public hospital in northeastern Malaysia
- Relationship between glycemic control and perceived family support among people with type 2 diabetes mellitus seen in a rich kinship network in Southwest Nigeria
- Adherence to clinical guidelines for monitoring diabetes in primary care settings
- Acknowledgement to reviewers
