Local anesthetic infiltration before open reduction and internalfixation for ankle fracture:a single-blind randomized controlled study
Juan Lopez-Valencia ,Juan Jonathan De la Cruz-PachecoJoel Galindo-AvalosJuan Manuel Gómez-GómezAlexis Rubén Álvarez-NarvaézAvelino Colín-VázquezAnapaola Koch-Leopo
1 High Specialty Medical Unit ‘‘Dr.Victorio de la Fuente Narváez’’,Mexican Institute of Social Security,Colector 15 s/n(Av.Fortuna)Esq.Av.Politécnico nacional.Col.Magdalena de las Salinas,Delegación Gustavo A.Madero,Mexico City,Mexico
2 Instituto de Seguridad y Servicios Sociales para los Trabajadores del Estado,Av.Marina Nacional 261 Col.Tacuba,Delegación Miguel Hidalgo,Mexico City,Mexico
Abstract
Key words:ankle fracture; surgery; local anesthetic infiltration; ropivacaine; bupivacaine; preemptive analgesia; randomized controlled trial
INTRODUCTION
Musculoskeletal injuries have become increasingly more common in the USA,with approximately three out of everyfive injuries occurring to this system.Fractures represent the second most frequent injury(25%).Ankle fractures occur in 187 per 100,000 persons every year.1Ankle fractures are a common musculoskeletal injury that occurs in a bimodal distribution.Young men predispose to ankle fractures because of high energy trauma and older women predispose to ankle fractures because of osteopenia and osteoporosis.2Ankle fractures constitute approximately 10% of all fractures and are the most common surgically orthopedic injury.3Supinationexternal rotation(SE)ankle fractures,also known as Weber B type ankle fractures are the most common ankle fractures and account for nearly 80% of all ankle fractures.4,5A decision for operative or non-operative treatment is based on the stability of the ankle; unstable fractures have a better outcome with surgical treatment than those treated conservatively.Medial instability associated with a lateral malleolar fracture can result from a medial malleolar fracture,a deltoid ligament lesion or a combination of osseous and ligamentous lesions.6While isolated lateral malleolar fractures may be biomechanically stable and amenable to non-operative treatment more complex bi-and trimalleolar ankle fractures and syndesmotic injuries often require open reduction and internalfixation(ORIF)to restore the native biomechanics of the ankle and prevent premature joint degeneration.Ankle fractures are painful.Generally,inadequate postoperative pain treatment may affect pulmonary function negatively,developing into atelectasis or pulmonary infections,and prolong recovery.Intense,uncontrolled postoperative pain may also lead to persistent pain.Being female,low educational level,report of illness or chronic illness were found to be predictors of chronic pain in a Norwegian cohort.7
It has been suggested that preoperative infiltration of local anesthetics provides a greater reduction in postoperative pain than perioperative or postoperative infiltration; nerve impulse block resulting from local infiltration prevents nociceptive impulses from reaching the central nervous system and suppresses the sustained state of hyperexcitability responsible for intense postoperative pain.8A clear correlation between increased local and regional anesthesia use and the success of major knee and shoulder procedures in an ambulatory setting has been shown.The preferred indication for local infiltration is foot and ankle surgery,as it allows for earlier ambulation and reduces the risk of falls when compared to more extensive blocks of the lower limp.9
Local and regional analgesia provides optimal analgesia,especially during mobilization,with significant reduction in using morphine-containing agents and its associated side effects,and faster functional recovery.It significantly reduces the in flammatory reaction at the incision.Local anesthetic infiltration into a surgical wound or joint blocks the pain at its origin -the surgical site itself -without altering motor function.This method is virtually devoid of side effects and it is particularly well-suited after ambulatory surgery.9
The purpose of this study was to investigate the preoperative use effects of local infiltration of ropivacaine or bupivacaine in pain management for open reduction and internalfixation treatment for ankle fractures.
SUBJECTS AND METHODS
Ethics statement
The study protocol was approved by the local ethics committee(IMSS ethical committee; approval No.R-2016-3401-55)on September 26,2016 and registered with ClnicalTrials.gov(Identifier:NCT02949674)on October 31,2016.All procedures performed in studies involving human participants were in accordance with the principles of the 1964Helsinki Declarationand its later amendments or comparable ethical standards.Informed consent was obtained from all individual participants included in the study.
Design and setting
This prospective single-blind randomized controlled trial was conducted between October 2016 and October 2017 at the Emergency Room of Traumatology,Orthopedic and Rehabilitation High Specialty Unit Dr.Victorio de la Fuente Narvaez that belongs to the Mexican Security Institute.
Study population
Ninety-three patients were included in this study.They were adult individuals(≥ 18 years old)with type B ankle fractures who underwent ORIF only through a lateral incision(with or without talar shift)and accepted to participate in the study(informed consent signature).Patients with other injury or fracture(polytrauma),or those who had a history of neuropathy or pain alteration before the ankle fracture,or those with skin injury before ORIF or open fractures were excluded from this study.Patients who did not complete the follow-up or desired terminating the study during the follow-up were withdrawn from this study.
Local anesthetic infiltration
The included patients were randomly divided into three groups:ropivacaine,bupivacaine,and control(n= 31 patients per group).All of them were prepared for ORIF.After spinal anesthesia(hyperbaric bupivacaine 0.5%,7.5 mg,Pisa laboratory,Guadalajara,México),local anesthetic infiltration with 37.5 mg 0.75% ropivacaine(Pisa laboratory,Guadalajara,México),25 mg 0.5% bupivacaine(Pisa laboratory),or no local anesthetic infiltration was applied in the ropivacaine,bupivacaine,or control groups,respectively(Figure 1).All patients underwent ORIF with only a direct lateral approach and then simple bandage was applied.Only patients were blinded to group assignment.The analgesic drugs only include nonsteroidal anti-in flammatory drugs,precisely acetaminophen 1 g,once every 8 hours,and ketorolac 30 mg intravenously once every 8 hours.
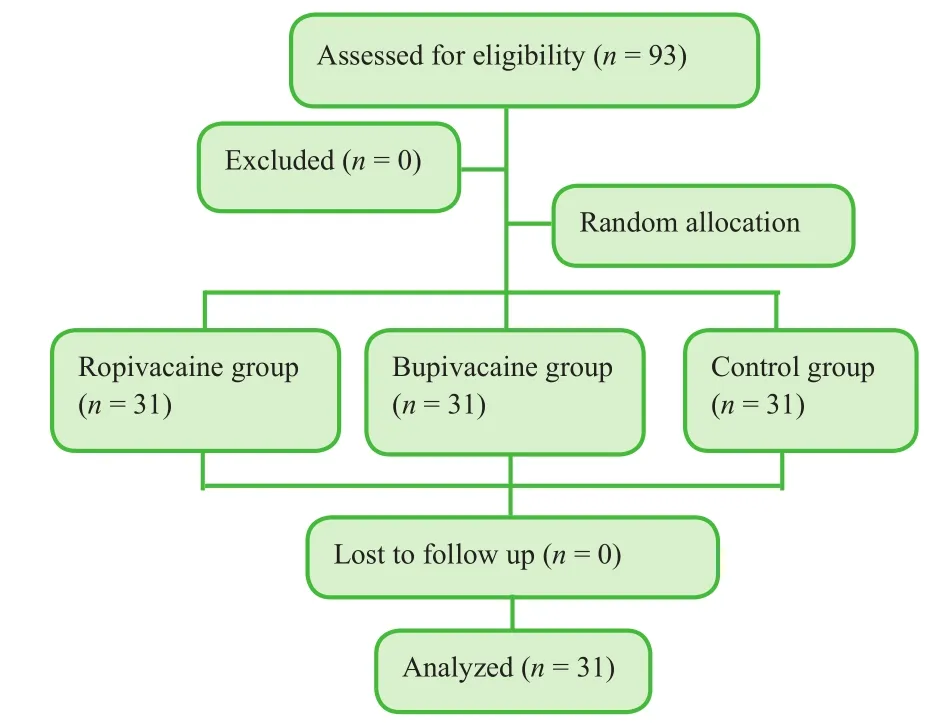
Figure 1:Flow chart(CONSORT diagram).
Pain assessment
We used the Visual Analog Scale(VAS)score10,11(0 = no pain,10 = maximum pain)to assess pain in patients at 4,8,12 and 24 hours after surgery.
Statistical analysis
Statistical analysis was performed using SPSS version 23.0 software(IBM,Armonk,NY,USA).One-way analysis of variance and the chi-square test were used.All data are expressed as the mean ± SD.AP-value < 0.05 was considered statistically significant.
RESULTS
Demographic data
Demographic data of 93 included patients,consisting of 51 women and 42 men,are shown in Table 1.Demographic characteristics of these patients were analyzed.
Pain
At 4 hours after ORIF,a more obvious analgesic benefit was observed in the ropivacaine group than in the bupivacaine and control groups(P< 0.05).There was no significant statistical significant in the analgesic effect among the three groups at 8,12 and 24 hours after surgery(P> 0.05)(Table 2).

Table 1:Demographic characteristics of patients in the ropivacaine,bupivacaine,and control groups

Table 2:Comparison of Visual Analog Scale scores among the three groups
DISCUSSION
Preemptive analgesia refers to the analgesic administration before surgical insult or tissue injury.It is based on the concept that central and peripheral sensitizations are the mayor causes of hypersensitivity to pain after injury.Preemptive analgesia can be done with nonsteroidal anti-in flammatory drugs,local anesthetics,cyclooxygenase-2-specific inhibitors,steroids,N-methyl-D-aspartate antagonists,alfa-2 agonist and anticonvulsants.12Regional anesthesia has been shown to improve postoperative pain control.13,14Peripheral nerve blocks have long been underused for acute pain management in orthopedic trauma.However,the associated side effects,time required to perform,and lack of the necessary expertise are some of the potential causes for not providing peripheral nerve blocks on a large scale.Common concerns in using peripheral nerve blocks include delayed ability to monitor postoperative neurological function and masking acute compartment syndrome.15
Ropivacaine has the similar efficiency to bupivacaine but it is associated with a longer acting and fewer complications in the nervous and cardiovascular systems.16It tends to have a quicker onset time than bupivacaine(by 2-15 minutes).17A clinically adequate dose of ropivacaine appears to be associated with a lower incidence of motor block and faster regression of motor block that stimulates earlier mobilization than bupivacaine.18
In a randomized clinical trial,19patients with femoral neck fractures underwent surgical treatment with internalfixation with two parallel hook pins.The analgesic effects of intraoperative infiltration with ropivacaine followed by six postoperative injections through an intra-articular catheter in 8-hour intervals(ropivacaine group)were compared with placebo(saline group).Results showed that there was no significant difference in consumption of standardized opioid rescue analgesics or pain between ropivacaine and saline groups.With the exception of reduction in nausea in the ropivacaine group on postoperative day 2,there was no significant difference in the occurrence of side effects between two groups.
In another randomized clinical trial,20patients with femoral fracture underwent surgical treatment with platefixation,intramedullary device or arthroplasty for a range of femoral fracture patterns.The efficacy of multimodal drug(ropivacaine,epinephrine and morphine)injectionversusno injection in pain control was compared.Results showed that the local drug injection improved pain control(as demonstrated by lower VAS score)and reduced narcotic utilization over thefirst operative day with no observed adverse effects than no injection.Therefore,we believe that multimodal analgesia is a better approach to prevent postoperative pain in patients with acute fracture than no analgesia.A combination of several drugs can be made to have better outcomes.More alternatives should be investigated in patients undergoing ORIF for ankle fractures like using a higher dose of local anesthetic,local anesthetic combinations or multimodal analgesia itself.
To conclude,local infiltration with ropivacaine in ORIF for acute ankle fractures reduced pain at 4 hours after surgery better than local infiltration with bupivacaine.However,the efficacy in pain control was not significant between these two analgesia methods.We believe that the most important factor to reduce pain in patients with acute ankle fracture is the fracturefixation itself.
Additionalfiles
Additionalfile 1:Ethical approval documentation.
Additionalfile 2:Model consent form.
Author contributions
Study design:JLV,JJDLCP,JGA,JMGG,ARÁN,ACV,AKL; study protocol:JLV,AKL; study implementation:JJDLCP,JGA,JMGG,ARÁN,ACV; data collection:JJDLCP,JGA,JMGG,ARÁN,ACV;statistical analysis and data discussion:JLV and AKL.All authors approved thefinal version of this paper.
Conflicts of interest
Financial support
None.
Institutional review board statement
This study protocol was approved by the local ethics committee(IMSS ethical committee; approval No.R-2016-3401-55)on September,26,2016,and performed in accordance with theDeclaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.In the form the patients have given their consent for their images and other clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement
This study followed the CONsolidated Standards Of Reporting Trials(CONSORT)statement.
如今是医药卫生体制改革的关键时期,公立医院应该结合自身发展的现实情况与需要,制定出符合社会发展与医药卫生事业发展的战略决策。而对于公立医院来讲,战略决策的制定与改变,必将会对各类资源的配置情况、使用情况、效益情况带来一定的影响。但是改革是未来的发展趋势,是一种客观必然,财务管理工作整体水平必须要随着改革的推进与升华得到进一步提高,而总会计师制度,能够为专业化的财务管理活动提供全方位的保障,如可以为公立医院的财务管理提供组织保障与人员保障等等,进而使得财务管理的功能与价值可以全面发挥出来。
Biostatistics statement
The statistical methods of this study were reviewed by the biostatistician of IMSS High Specialty Medical Unit Victorio de la Fuente Narváez in Mexico.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Individual participant data that underlie the results reported in this article,after deidentification(text,tables,figures,and appendices)will be available.Study protocol,informed consent form will be available immediately after publication.Data will be available for investigations whose proposed use of the data has been approved by an independent review committee identified for this purpose for individual participant data meta-analysis.Proposals should be directed to corresponding author(juanlopez110@hotmail.com).Anonymized trial data will be available indefinitely at mail juanlopez110@hotmail.com.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal,and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License,which allows others to remix,tweak,and build upon the work non-commercially,as long as appropriate credit is given and the new creations are licensed under the identical terms.
 Clinical Trials in Orthopedic Disorder2018年4期
Clinical Trials in Orthopedic Disorder2018年4期
- Clinical Trials in Orthopedic Disorder的其它文章
- Ultrasound-guided supine lumbar plexus block versus iliac fascia block for analgesia in older adult patients undergoing hip replacement:a randomized controlled trial
- Efficacy of arthroscopic surgery for discoid lateral meniscus injury in knee joint:a self-control study
- Clinicopathological characterization of long bone non-union:a prospective cross-sectional study
- Efficiency of tight monitoring by nurse practitioners in rheumatoid arthritis patients in remission after treatment with rituximab:study protocol for a randomized,open-label,controlled trial
- Hemostasis following local versus intravenous tranexamic acid in patients undergoing posterior open reduction and internalfixation of thoracolumbar fractures:study protocol for a parallel-group,randomized controlled trial
- Efficacy of silver needle acupuncture combined with muscle relaxation in the treatment of capulohumeral periarthritis:study protocol for a prospective,single-center,randomized,parallel-controlled trial
