Amnion epithelial cells – a novel therapy for ischemic stroke?
Megan A. Evans, Brad R.S. Broughton, Grant R. Drummond, Henry Ma, Thanh G. Phan, Euan M. Wallace , Rebecca Lim ,Christopher G. Sobey,
Abstract Stroke is a leading cause of death and disability and new therapies are desperately needed. Given the complex nature of ischemic brain injury, it has been postulated that cell‐based therapies may be useful.However, cell resources, invasive extraction procedures, immunological rejection, tumorigenesis and eth‐ical challenges make it unlikely that many stem cell types could serve as a practical source for therapy. By contrast, these issues do not pertain to human amnion epithelial cells (hAECs), which are placenta‐derived stem cells. We recently assessed the effects of systemically delivered hAECs on stroke outcome using four animal models of stroke. We demonstrated that when injected intravenously after ischemia onset, hAECs migrate preferentially to the spleen and injured brain to limit apoptosis and in flammation, and attenuate early brain in filtration of immune cells, progression of infarction and systemic immunosuppression and to ultimately ameliorate functional de ficits. When administration of hAECs is delayed by 1-3 days post‐stroke, long‐term functional recovery can still be enhanced in young and aged mice of either sex. Moreover,our proof‐of‐principle findings suggest that hAECs are effective at limiting post‐stroke infarct development in non‐human primates. Overall, the results suggest that hAECs could be a viable clinical stroke therapy.
Key Words: ischemic stroke; cerebral infarction; stem cells; human amnion epithelial cells; in flammation;immunosuppression; brain repair; mouse; non-human primate
Introduction
Stroke is the world’s second leading cause of death after ischemic heart disease, accounting for 6.7 million deaths annually (Mozaffarian et al., 2016). It is also the greatest cause of long‐term disability in adults, with up to half of all survivors failing to regain independence (Mozaffarian et al., 2016). Currently, there is only one approved phar‐macological agent available to treat stroke, recombinant tissue plasminogen activator (rtPA), which must be ad‐ministered within a 4.5 hours window of stroke onset and only after computed tomography (CT) or magnetic reso‐nance imaging (MRI) has diagnosed a thrombotic cause.Due to these strict timing limitations, only approximately 15% of stroke patients are eligible to receive rtPA (Phan et al., 2018). An additional therapy involving endovascu‐lar clot retrieval (ECR), for large clot removal, has been recently approved for use up to 8 hours from the onset of stroke in patients who have received rtPA or who are already taking anti‐coagulant medication (Phan et al.,2018). However, even with this extended time window,less than 5% of additional patients are eligible for ECR(Phan et al., 2018). Consequently, there is a desperate need to identify additional effective therapies to improve outcome for a larger proportion of stroke patients.
Cell‐based therapies, which have the potential to tar‐get multiple injury mechanisms in a more coordinated manner, have been gaining interest as a treatment option for stroke. While a number of different cell types have been evaluated for stroke therapy, the most commonly used type of cells is stem cells. Stem cells are de fined as undifferentiated cells capable of self‐renewal, and can be broadly classified as being of embryonic, fetal or adult origin (Broughton et al., 2013). Administration of various stem cell lineages has been reported to reduce brain inju‐ry and facilitate recovery after experimental stroke. Nota‐bly, it has been documented that stem cells can be admin‐istered up to several days after stroke and still promote improvement or recovery (Broughton et al., 2013). Fur‐ther, there have been a number of clinical trials assessing the safety and/or efficacy of stem cell therapy for stroke,which have reported varying levels of success (Nagpal et al., 2017). The most frequently used stem cell types in stroke research include embryonic, mesenchymal (usually derived from bone marrow or umbilical cord), neural and induced pluripotent stem cells (Broughton et al., 2013).Whilst all of these cell types have been demonstrated to have efficacy at improving experimental stroke outcome,they possess a number of limitations, which may restrict their use as a routine treatment option. These limitations include immune rejection, tumor formation, limited sources and availability, invasive extraction, unsuitability for systemic delivery and/or ethical concerns (Broughton et al., 2013). However, none of these limitations appear to pertain to the human amnion epithelial cell (hAEC)(Broughton et al., 2013; Evans et al., 2018).
hAECs
hAECs are derived from the epithelial layer of the am‐nion, which is the sac that encloses the developing fetus and is attached to the placenta. hAECs are fetal in origin and thus display a high degree of pluripotency. However,as these cells are obtained from discarded term placen‐tae, they do not possess ethical constraints to their use as do embryonic stem cells, for example (Broughton et al.,2013). Also unlike some of the other stem cell lineages,hAECs are readily available and do not require invasive extraction procedures for harvesting. Likely reflecting their role in maintaining maternal immune tolerance of the fetus during pregnancy, hAECs are immunologically inert and have low surface expression of human leuko‐cyte antigen (HLA)‐A, HLA‐B, HLA‐C and HLA‐DR,which are key antigens involved in transplant rejection(Broughton et al., 2013; Phan et al., 2018). On the other hand, hAECs express and release the non‐polymorphic,non‐classical antigen, HLA‐G, which is able to directly suppress immune responses. Consistent with these prop‐erties, it has been known for over 35 years that hAECs can be safely transplanted into humans without evidence of immune rejection (Broughton et al., 2013). Amnion cells or strips of amnion membrane have long been used to reduce scarring and promote healing in burn victims or following corneal surgery, also suggesting hAECs are well tolerated by a recipient’s immune system. Furthermore,hAECs do not form tumorsin vivoas they lack telomer‐ase enzyme, nor do they differentiate into fibroblasts, as can mesenchymal stem cells, for example (Broughton et al., 2013; Phan et al., 2018). Overall this pro file of charac‐teristics suggests that hAECs are an inherently safer cell for transplantation than many other stem cell types.
hAECs as A Potential Therapy for Stroke
To exploit the above‐mentioned beneficial properties,we recently tested the efficacy of systemically delivered hAECs to improve a number of outcome measures in four animal models of ischemic stroke (Evans et al.,2018). The cells were harvested from term placentae of healthy women following uncomplicated pregnancies,and were stored frozen under good manufacturing prac‐tice conditions until use. Importantly, the cells were administered, without further manipulation, to immune competent animals with no evidence of immune rejec‐tion. Our data indicate that hAECs provided substantial bene fit even when administered up to 3 days following a stroke. Speci fically we showed that when administered to mice acutely after onset of cerebral ischemia, hAECs mi‐grate to the injured brain in a C‐X‐C chemokine receptor(CXCR)4‐dependent manner to limit apoptosis and in‐flammation, attenuate early brain in filtration of immune cells, reduce progression of infarction and ultimately ameliorate functional de ficits (Figure 1). We also showed that a considerable number of hAECs migrate to the spleen, and that an intact spleen is required for hAECs to fully elicit their neuroprotective effects. Additionally,we found that hAECs are effective at blunting systemic post‐stroke immunosuppression, a phenomenon that leaves stroke patients particularly vulnerable to infectious complications (Anrather and Iadecola, 2016) (Figure 1).Moreover, when administration of hAECs was delayed by 1–3 days post‐stroke, long‐term functional recovery was still observed to be enhanced in young and aged mice of either sex, regardless of infarct size. The data also sug‐gest that hAECs may enhance endogenous brain repair processes, as we observed changes to the structure of the glial scar, and more microtubule‐associated protein 2(MAP‐2)‐positive cells present in the peri‐infarct region in animals treated with hAECs (Figure 1). To further assess and extend the potential translatability of our find‐ings we also obtained proof‐of‐principle evidence that in‐travenous (i.v.) administration of hAECs reduces infarct development in non‐human primates (i.e., marmosets).Overall, these findings strongly indicate that hAECs could be a viable and effective clinical stroke therapy.
An important feature of our pre‐clinical study was that hAECs were administered systemically post‐stroke (Ev‐ans et al., 2018). While one previous study reported that hAECs could reduce infarct volume and behavioral de fi‐cits following ischemic stroke when administered directly into the injured brain tissue (Liu et al., 2008), intracere‐bral administration of hAECs is unlikely to be practicable clinically for several reasons. First, intracerebral admin‐istration will likely require expensive imaging equip‐ment and expertise not readily available in many stroke centres. Intracerebral administration may itself cause further brain injury, and it is an approach which does not likely target the systemic mechanisms that contribute to impaired outcomes after stroke, particularly the systemic immune response (Anrather and Iadecola, 2016).
Studies indicate that hAECs possess potent immuno‐modulatory properties and can reduce inflammation in several experimental disease settings (Broughton et al.,2013; Tan et al., 2014, 2015). It is therefore not surprising that a common finding across our mouse models of ce‐rebral ischemia was that hAECs were able to modify the post‐stroke immune response. More specifically, when administered acutely following transient cerebral isch‐emia, hAECs therapy limited the numbers of immune cells (neutrophils, monocytes/macrophages, B cells and T cells) and M1 polarized macrophages present in the brain. Following permanent cerebral ischemia, hAECs also reduced numbers of brain‐infiltrating T cells. Fur‐ther, when hAECs were administered in a delayed man‐ner (after 24 hours) following photothrombotic stroke,they were still able to modify the stroke‐induced changes occurring to peripheral myeloid and lymphoid cell pop‐ulations. It is likely that early administration of hAECs is necessary to sequester inflammation, which contributes to secondary brain damage following acute stroke. How‐ever, we predict that modulating the immune response once stroke‐induced brain injury is established would still be bene ficial for overall recovery. For instance, it is known that hAECs can promote T regulatory cell expan‐sion and M2 macrophage polarization (Tan et al., 2014,2015), which may assist in brain repair processes (An‐rather and Iadecola, 2016).
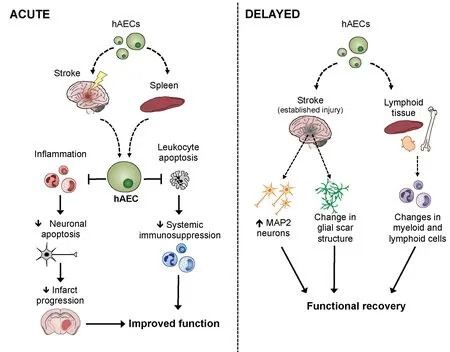
Figure 1 A schematic of the likely mechanisms by which human amnion epithelial cells (hAECs) improve outcome after stroke.
Lung infections are a major cause of post‐stroke mor‐bidity and mortality and can delay recovery processes(Anrather and Iadecola, 2016; Stanley et al., 2016). As mentioned, these infections are thought be a consequence of a profound systemic immunosuppression, which de‐velops over the hours to days following a stroke (Anrather and Iadecola, 2016). Importantly, we found that hAECs were also effective at preventing post‐stroke systemic im‐munosuppression, particularly the reduction in splenic and circulating leukocytes (by apoptosis) and the associ‐ated splenic atrophy (Evans et al., 2018). These changes occurred in association with improved functional out‐come, which may suggest that such mice would develop fewer infections. While we did assess levels of bacteria in the lungs at 72 hours, this only included aerobic (not anaerobic) bacteria. It is currently thought that following a stroke, the gut becomes leaky and as the host’s immune system is compromised, this allows for the translocation of bacteria from the gut to the lungs, resulting in infec‐tion (Stanley et al., 2016). As the majority of bacteria in the gut are anaerobic, future studies should also examine the effect of hAECs on anaerobic lung infections after stroke to fully understand the efficacy of hAECs to pre‐vent post‐stroke infections.
Translational Perspectives
In 1999, a series of conferences was held called the ‘Stroke Treatment Academic Industry Roundtable’ or ‘STAIR’(Stroke Therapy Academic Industry Roundtable (STAIR),1999). The intention of these conferences was to develop guidelines on how to best proceed in the development of stroke therapies in order to overcome the translational roadblock from laboratory to clinic. Similarly, the Stem cell Therapies as an Emerging Paradigm in Stroke or‘STEPS’ meeting was organized to create a framework to guide investigations in stem cell therapy for stroke (Stem Cell Therapies as an Emerging Paradigm in Stroke Par‐ticipants, 2009). Importantly, our studies were performed in support of STAIRs and STEPs recommendations, as we utilized models of permanent and transient cerebral ischemia, models that include cortical and subcortical infarcts, animals of both sexes, as well as aged animals.We assessed different time‐points at which hAECs could be delivered post‐stroke, and outcomes during acute (1–3 days) and delayed (7–56 days) phases. Furthermore, our data from six marmosets were in accordance with the guidelines for therapeutic development, which recom‐mend that once efficacy is established in rodents, studies be carried out in gyrencephalic species, such as non‐hu‐man primates, before taking the therapeutic through to studies in humans. Hence, the next stage of this research will be to assess the safety and efficacy of hAECs in hu‐mans following a stroke. Indeed we have now registered a Phase I clinical trial to assess the maximum tolera‐ble dose of hAECs in human ischemic stroke patients(Australian New Zealand Clinical Trials Registry: AC‐TRN12618000076279p; Phan et al., 2018). From a safety perspective, it is known that hAECs can be injected into healthy humans without evidence of immune rejection or tumor formation and it is therefore predicted that hAECs can also be safely administered to stroke patients(Broughton et al., 2013; Phan et al., 2018). Further, with nearly 4 million births per year in the USA alone, and an average yield of 150–200 million cells per placenta,hAECs are a readily available and relatively cheap source of cells for subsequent clinical application.
Conclusions
Our pre‐clinical study (Evans et al., 2018) provides the first evidence that systemically delivered hAECs can im‐prove outcomes following experimental ischemic stroke.Overall, we suggest that hAECs represent a genuinely new opportunity for the treatment of ischemic stroke with a therapeutic window of efficacy that extends sub‐stantially beyond the current 4.5 hours for rtPA.
Author contributions:All authors contributed to the drafting of the article.
Conflicts of interest:None declared.
Financial support:None.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- In Memoriam: Ray Grill (1966–2018)
- Reorganization of injured anterior cingulums in a hemorrhagic stroke patient
- A novel chronic nerve compression model in the rat
- Analgesic effect of AG490, a Janus kinase inhibitor, on oxaliplatin-induced acute neuropathic pain
- Three-dimensional visualization of the functional fascicular groups of a long-segment peripheral nerve
- Novel conductive polypyrrole/silk fibroin scaffold for neural tissue repair