A tissue-engineered rostral migratory stream for directed neuronal replacement
John C. O’Donnell , Kritika S. Katiyar , , Kate V. Panzer, D. Kacy Cullen , ,
Abstract New neurons are integrated into the circuitry of the olfactory bulb throughout the lifespan in the mamma‐lian brain—including in humans. These new neurons are born in the subventricular zone and subsequently mature as they are guided over long distances via the rostral migratory stream through mechanisms we are only just beginning to understand. Regeneration after brain injury is very limited, and although some neuroblasts from the rostral migratory stream will leave the path and migrate toward cortical lesion sites,this neuronal replacement is generally not sustained and therefore does not provide enough new neurons to alleviate functional de ficits. Using newly discovered microtissue engineering techniques, we have built the first self‐contained, implantable constructs that mimic the architecture and function of the rostral migratory stream. This engineered microtissue emulates the dense cord‐like bundles of astrocytic somata and processes that are the hallmark anatomical feature of the glial tube. As such, our living microtissue‐en‐gineered rostral migratory stream can serve as an in vitro test bed for unlocking the secrets of neuroblast migration and maturation, and may potentially serve as a living transplantable construct derived from a patient’s own cells that can redirect their own neuroblasts into lesion sites for sustained neuronal replace‐ment following brain injury or neurodegenerative disease. In this paper, we summarize the development of fabrication methods for this microtissue‐engineered rostral migratory stream and provide proof‐of‐princi‐ple evidence that it promotes and directs migration of immature neurons.
Key Words: rostral migratory stream; glial tube; astrocyte; neuroblast; brain injury; neural repair; neural regeneration; tissue engineering
Introduction
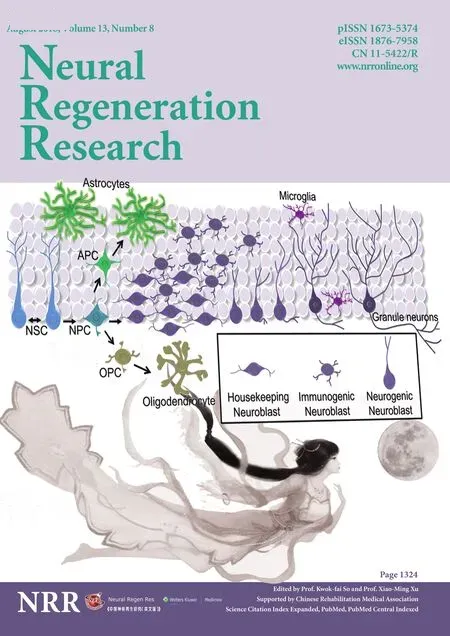
Neurogenesis continues post‐development in the brains of humans and other mammals, but it is limited to the dentate gyrus and subventricular zone (SVZ) (Zhao et al., 2008; Ming and Song, 2011). Remarkably, newly born neurons from the SVZ migrate long distances to the olfactory bulb along a path‐way comprised of aligned astrocytes referred to as the glial tube. This rostral migratory stream (RMS) is active through‐out one’s lifetime, and therefore may present an endogenous source to replace neurons lost due to aging, neurodegenera‐tive disease, and/or brain injury. However, neuroblasts are in‐trinsically programmed to follow the RMS owing to a precise presentation of spatial cues along astrocytes comprising the glial tube (Gengatharan et al., 2016). Neural tissue engineer‐ing yields promising three‐dimensional (3D) constructs to facilitate nervous system regeneration by replicating speci fic neuroanatomical features. In an exciting recent development,we have created the first implantable microtissue designed to replicate the structure and function of the glial tube (Figure 1).This biologically‐inspired strategy—referred to as microtissue astrocytic constructs (MACs)—may therefore be useful to re‐direct migration of endogenous neuroblastsin vivoand could also serve as an anatomically‐relevant test bed to study the RMS or accelerate neuroblast maturationin vitro. MACs are generated based on newfound microtissue engineering tech‐niques that promote self‐assembly of astrocytes into networks of longitudinally‐aligned bundles (Winter et al., 2016; Katiyar et al., 2018). In compelling proof‐of‐concept experiments, we found that MACs directly facilitate the alignment and migra‐tion of immature neurons.
Anatomical Inspiration and Characterization to Date
Glial tube astrocytes possess a bipolar morphology, ex‐tending processes in opposite directions along the RMS in parallel with each other to form a cord‐like bundle. We have established that these structural features are recapitulated in MACs (Winter et al., 2016; Katiyar et al., 2018). As sum‐marized in Figure 1B, the overall biofabrication process involves seeding the inner lumen of custom‐built, hollow hydrogel micro‐columns with dissociated astrocytes. Then,over a remarkably short timeframe of just several hours, the cells spontaneously self‐assemble into dense cables of longi‐tudinally‐aligned astrocytes with bipolar morphology. This MAC biofabrication process was optimized by systematically testing several criteria, including culture media constituents,micro‐column diameter, collagen concentration, and cell seeding density (Winter et al., 2016). We found that cultur‐ing in serum‐free defined media induced a process‐bearing morphology in astrocytes, whereas media containing serum promoted a proliferative phenotype of flat astrocytes lacking processes, consistent with previous reports (Morrison and de Vellis, 1981; Kim et al., 1983; Katiyar et al., 2016). Therefore,all micro‐columns loaded with astrocytes were fed serum‐free medium. The micro‐columns were fabricated using agarose,speci fically chosen based on biocompatibility, mass transport properties, optical transparency, and perhaps most impor‐tantly for this application, lack of adhesive ligands so that while providing geometric structure it would not inhibit 3D cell/microtissue remodeling. As such, we found that it was necessary to coat the inner lumen of the agarose micro‐col‐umns with type 1 rat tail collagen to promote initial astrocyte adhesion. Subsequently, the breakthrough most responsible for MAC self‐assembly was our observation that decreasing the inner diameter of the micro‐columns increased the degree of astrocytic alignment, with diameters of < 350 μm resulting in preferential process extension along the longitudinal axis.These results suggested that the angle of curvature of the in‐ner lumen had a strong in fluence over the direction of process growth. We also optimized the collagen concentration within the inner lumen. Collagen loaded at 2.0 mg/mL formed a solid core within the micro‐column, preventing seeding with astrocytes, while concentrations of 0.0 and 0.5 mg/mL result‐ed in a lack of cell adhesion. Fortunately, 1.0 mg/mL collagen not only provided necessary adhesive properties, but was also sufficiently permissive as to allow astrocytes to remodel the extracellular matrix, pulling in collagen with their processes to incorporate it into their longitudinally‐aligned bundles.To test for effects of seeding density, astrocytes were loaded into micro‐columns with an inner diameter of 350 μm at‘low” (2—3 × 105cells/mL), ‘medium” (5—6 × 105cells/mL),or ‘high” (9—12 × 105cells/mL) cell concentrations. While all seeding densities resulted in alignment of processes, higher densities were associated with robust bundling of astrocytes and collagen to form dense cables of longitudinally‐aligned astrocytes.
These bundled MACs were found to be exceptionally durable and flexible (Figure 1G), and they exhibit encour‐aging signs of neuronal support and interaction (Figure 1I). Indeed, we previously demonstrated that MACs can be extracted from the hydrogel micro‐columns after bundling and reshaped into various orientations without damage to the astrocytes (Winter et al., 2016; Katiyar et al., 2018). This durability allows for the implantation profile to be signifi‐cantly reduced by extracting the bundles from the larger(“sacrificial”) micro‐column before implantation, and the flexibility allows the constructs to assume a non‐linear shape to accommodate specialized anatomical needs. We have previously performed stereotaxic implantation of similar‐ly‐shaped neuronal constructs into the cortex, thalamus, and striatum, so the procedures have all been well‐established in our laboratory (Struzyna et al., 2015b; Harris et al., 2016;Serruya et al., 2017). Moving forward, these microtissue constructs may provide a powerfulin vitroplatform for studying the RMS, and offer exciting potential for enhancing and redirecting endogenous neuroblast migrationin vivoto promote neuroregeneration after injury or disease.

Figure 2 Immature neurons migrate out of cortical neuronal aggregates and along bundled microtissue astrocytic constructs (MACs), but not into micro-columns coated with collagen-only.
A Unique In Vitro Test Bed to Study Neuroblast Migration and Maturation
Periodically, members of a subset of neural stem cells in the SVZ take a step towards maturation by becoming neu‐roblasts. These neuroblasts then migrate within a cord‐like bundle of astrocytes comprising the glial tube of the RMS,arriving in the olfactory bulb where they continue to devel‐op into mature interneurons that integrate into the existing circuitry (Lois and Alvarez‐Buylla, 1994; Peretto et al., 1997;Wang et al., 2011; Gengatharan et al., 2016). Many basic questions facing adult neurogenesis, migration, maturation,and physiological relevance remain unanswered (Ming and Song, 2011). Anin vitrosystem for studying these phenom‐ena would offer new capabilities and experimental control.For example, anin vitroRMS model could allow for precise manipulation of conditions at the source, migratory path,or destination (after exiting the far end of thein vitroRMS)to answer important questions regarding the timing and lo‐cation of cell fate determination during adult neurogenesis.Contact with astrocytes in otherin vitrosystems increases neuroblast migration distance and proliferation of precursor cells to form new neuroblasts, but results from these stud‐ies lacked signature features of the RMS, such as astrocyte organization or neuroblast chain migration (Lim and Al‐varez‐Buylla, 1999; Zhang et al., 2016). Studying adult neu‐rogenesis in human tissue presents even greater challenges of accessibility and control. Anin vitroRMS made from human induced neural progenitor cells would allow investi‐gators to ask speci fic questions that are currently untestable.It is noteworthy that as a complimentary proof‐of‐concept for this general approach, we have previously used a customin vitroparadigm consisting of traumatically‐injured 3D neuronal‐astrocytic co‐cultures as a test bed to study and optimize factors associated with therapeutic implantation of exogenous neural stem cells (Cullen et al., 2007, 2011).
Regarding the use of MACs as anin vitrotest bed, our re‐cent studies suggest that MACs effectively emulate the mor‐phology, organization, and protein expression of the glial tubes. To test whether MACs functionally emulate the glial tubes with respect to driving immature neuron migration,we performed a preliminary migration assay experiment.On day 0, collagen‐coated micro‐columns were either seed‐ed with astrocytes or left empty to serve as controls. Cortical neurons were harvested from embryonic day 18 rats and a“forced cell aggregation” method was applied using gentle centrifugation within inverted pyramid micro‐wells to form neuronal aggregate micro‐spheres as described previously(Struzyna et al., 2017). Overnight, neuronal aggregates were virally transduced (adeno‐associated virus (AAV) vector,synapsin promoter) to express green fluorescent protein(GFP), and separately, astrocytes within micro‐columns aligned and bundled the collagen‐coated lumen to form MACs. On day 1, we placed the GFP‐labeled cortical neuronal aggregates in one end of micro‐columns containing densely bundled MACs, or into the cell‐free collagen control mi‐cro‐columns. On day 3 (48 hours post‐aggregate placement)we observed chain migration of immature neurons out of the aggregates and along the MACs; in contrast, neuron migra‐tion was not observed in the collagen control micro‐columns,demonstrating proof‐of‐principle that this technology can se‐lectively facilitate and direct migration of immature neurons(Figure 2). Therefore, MACs offer a unique platform to study the RMS and neuroblast migrationin vitro.
Neuroregeneration after Injury
Neuronal proliferation/migration is altered after brain injury,in some cases resulting in migration of neuroblasts to injury sites, and their presence within the first week after injury can improve recoveryvianeurotrophic factor release. However,during this acute period the environment is not conducive to neuronal replacement or regeneration. Formation of a glial scar after injury—while vital for reestablishing the blood brain barrier and limiting the spread of inflammation and excitotoxicity (Rolls et al., 2009)—has also been shown in many studies to act as an extrinsic barrier to axon regener‐ation and cell migration (Fawcett and Asher, 1999; Silver and Miller, 2004; Burda and Sofroniew, 2014; Ohtake and Li,2015). However, neuroblasts from the SVZ were found to mi‐grate out of the RMS and into damaged striatum after middle cerebral artery occlusion in rats, where they developed into mature neurons and formed synapses with surviving neurons 90 days post injury, though the level of neuronal replacement did not appear to have a physiological impact (Yamashita et al., 2006). This suggests that although neuroregeneration in the adult mammalian brain is severely lacking, inherent mechanisms do exist for neuronal replacement. MACs can potentially amplify and augment the brain’s existing mecha‐nisms for replacing lost neurons in order to achieve levels of neuroregeneration that are sufficient to improve recovery.
Implantation of MACs to Enhance Endogenous Neuroregenerative Processes
MACs are the first implantable microtissue constructs de‐signed to redirect the migration of endogenous neuroblasts from the RMS to sites throughout the brain. Whereas prior studies have transplanted fetal grafts, single cell suspensions,or cells in 3D matrices, our method is considerably different in that the final cytoarchitecture of the MAC—mimicking that of the RMS—is fully biofabricatedin vitroand then precisely delivered to redirect migration of endogenous neuroblasts to sites of neurodegeneration. While the direct implantation of neural stem cells into injury sites has been shown to improve outcome by providing neurotrophic factors, appropriate maturation and integration of these ex‐ogenous cells to functionally replace lost neurons remains a signi ficant challenge (Rolfe and Sun, 2015; Yamashita et al.,2017). In contrast, endogenous neuroblasts from the SVZ have been observed migrating into injured striatum and forming mature, synaptically‐integrated neurons (Yamashita et al., 2006). MACs may be able to expand and sustain this natural regenerative response of SVZ neuroblasts after inju‐ry. Of note, migration and maturation of neuroblasts along the RMS relies on complex, dynamic signaling between astrocytes and neuroblasts (Mason et al., 2001; García‐Mar‐qués et al., 2010; Gengatharan et al., 2016). Unlike extracel‐lular‐matrix‐based constructs that simply offer a permissive substrate (Fon et al., 2014; Ajioka et al., 2015; Fujioka et al.,2017), MACs possess a unique astrocytic microtissue make‐up that can provide directional, structural, and neurotrophic support, making them capable of sending and responding to complex signals with migrating neuroblasts and the local micro‐environment. In this way, MACs are an example of a tissue engineered “living scaffold”—a class of implantable constructs designed to facilitate nervous system regenera‐tion by emulating developmental mechanisms facilitated by living cells in a de fined anatomically‐inspired architecture—similar to other constructs being developed by our group(Struzyna et al., 2014, 2015a).
Mimicking the RMS may also facilitate development of neu‐roblasts during migration along MACs, allowing for the new neurons to functionally replace lost neurons after the majority of the degeneration has occurred instead of merely acting as neurotrophic factories in the acute and sub‐acute time periods.Moreover, their miniature form factor allows for minimally in‐vasive, stereotactic delivery into the brain (Harris et al., 2016).In rat models, we have previously demonstrated the ability to precisely microinject allogeneic neuronal microtissue con‐structs, which maintain pre‐transplant architecture, survive,and integrate into the native nervous system (Struzyna et al.,2015b; Harris et al., 2016; Serruya et al., 2017). In addition to directing and augmenting delivery and maturation of neuro‐blasts, MACs may also be able to deliver neuroblasts through the glial scar and into the injury site, thereby providing a sus‐tained supply of new endogenous neurons to replace lost cells.If the astrocytes in our construct become reactive via interac‐tion with the glial scar, we can modify secondary biomaterial encasement to prevent MAC disorganization and scar‐mediat‐ed activation. This approach to mimicking the brain’s existing method for neuronal replacement may be relevant for multiple neurological afflictions, including traumatic brain injury (TBI),stroke, and neurodegenerative disease.
Conclusions and Future Directions
We have developed techniques to fabricate densely‐bun‐dled cables of longitudinally‐aligned bipolar astrocytes that are durable and flexible enough for extraction from their microtubule chrysalis to allow for minimally‐disruptive transplantation. We have demonstrated that MACs can fa‐cilitate migration of neuroblastsin vitro, providing evidence of functional emulation of the RMS in addition to their structural similarities with the glial tube. MACs provide a novelin vitrotest bed for answering questions about the RMS, neuroblast migration, and cell fate determination that could not previously be addressed due to technical limita‐tions. Current approaches to regeneration after TBI, stroke,or neurodegeneration can generally be categorized as either pharmacological or stem cell transplant strategies. In devel‐oping MACs, we are pursuing a new strategy to amplify the brain’s inherent—though currently insufficient—mechanism for replacing lost neurons, in which neuroblasts migrate tangentially out of the RMS toward sites of injury. The glial tubes of the RMS are the most efficient means of facilitating neuroblast migration and maturation in the mammalian brain through adulthood, and we believe that by emulating the glial tubes, MACs can enhance and sustain the brain’s natural regenerative response.
Acknowledgments:The authors thank Dayo O. Adewole, University of Pennsylvania for technical assistance with these studies.
Author contributions:JCO’D participated in the design and execution of the work described, and wrote the initial draft of the manuscript. KSK participated in design and execution and KVP participated in execution. DKC conceived of the strategy, participated in design, and guided execution. All authors contributed to editing the manuscript.
Conflicts of interest:None declared.
Financial support:This work was supported by the National Institutes of Health [U01-NS094340 (Cullen), F31-NS090746 (Katiyar)&F32-NS103253 (O’Donnell)], University of Pennsylvania [Center for Undergraduate Research&Fellowships (Panzer)], Michael J. Fox Foundation[Therapeutic Pipeline Program #9998 (Cullen)], Department of Veterans Affairs [RR&D Merit Review I01-RX001097 (Cullen)&BLR&D Merit Review I01-BX003748 (Cullen)], and the U.S. Army Medical Research and Materiel Command [W81XWH-16-1-0796 (Cullen)].
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- In Memoriam: Ray Grill (1966–2018)
- Reorganization of injured anterior cingulums in a hemorrhagic stroke patient
- A novel chronic nerve compression model in the rat
- Analgesic effect of AG490, a Janus kinase inhibitor, on oxaliplatin-induced acute neuropathic pain
- Three-dimensional visualization of the functional fascicular groups of a long-segment peripheral nerve
- Novel conductive polypyrrole/silk fibroin scaffold for neural tissue repair