A proposed model for best practice in nursing clinical teaching in China
(Department of Surgery, Fujian Provincial Governmental Hospital, Fuzhou, Fujian, 350001)
Introduction
Clinical teaching is the backbone of nursing education. The teacher's central role is clinical instruction or clinical teaching, rather than supervision. Supervision implies administrative activities such as overseeing, directing, and managing the work of others[1]. Practice can provide students with a chance to learn about clinical reasoning and judgment[2]. Moreover, clinical experience is critical in transforming a student nurse into a professional nurse.
In China, nursing education has its own unique features. The clinical teaching for the related learning experience among nursing students is handled by staff nurses on duty, and not clinical instructors from the colleges of nursing. Although only one nursing student is assigned to each staff nurse, clinical teaching takes place during the duty hours of the staff nurse. These staff nurses are selected from specific nursing units, and have at least three years of clinical experiences. They are appointed by the nursing administration, and are assigned to a nursing student upon receiving the university's request letter. The university pays remuneration to the appointed staff nurses according to their supervision hours[3].
With the above unique features of China's nursing education, however, some concerns emerge. ①The quality of clinical teachers varies .②Clinical teachers do not effectively combine theory and practice. ③The common practice of staff nurses acting as clinical teachers seems to be to use nursing students merely as “extra hands”. It seems that the concentrated arrangement of clinical instruction is more for the convenience of the agency than for the education of nursing students[4].
The aim of this study is to investigate the experiences of current nursing clinical teaching in China, and to design a corresponding model to bridge the gap between practices of clinical teachers in clinical settings in China and the clinical instructors standard teaching practice in clinical settings in the Philippines.
Methods
Design
A phenomenological-qualitative, non-experimental type of research, including focus group discussions were utilized to discover the actual experiences of staff nurses regarding the nursing clinical teaching model as utilized in China in the study.
Sample
The population in this study was staff nurses/clinical teachers in China. Quota sampling was used to recruit the participants to mimic the known characteristics of the target group and to ensure an adequate number of subjects in each stratum.
From the one hundred and twenty-eight staff nurse participants of this study, twenty-seven were recruited for the five focus groups to be conducted with the following number of members per unit.
The general criteria for inclusion were being a staff nurse, currently working in a clinic and having at least 3 years' clinical teaching experience. Participants were personally recruited by the researcher discretely through visiting one by one to inform them the details and invite them to be participants. The researcher chose clinical teachers with higher education levels and more experience as participants (see Table 1).
Data collection
For five groups, comprising three to eight staff nurses/clinical teachers per group working in different clinical units, were used for data collection, and this involved questioning them about their perspectives on the past and present experiences of clinical teachers on clinical teaching the nursing students in China (see Fig 1). Each interview only lasts about 40 to 60 min since all of them have a family, and act as housewife at their home. The researcher initiated the interview with a briefing covering the objectives of the activity, observance of confidentiality and informed consent signified by the presence of participants. Permission to audio record the proceeding and for the presence of a research assistant to record the flow of discussion was sought from the participants. Five participants of the focus group refused to be recorded. In this case, the interviewer documented the proceedings by taking notes. In addition, data from recordings and written material were securely stored.

Table 1. Profile of FGD Participants
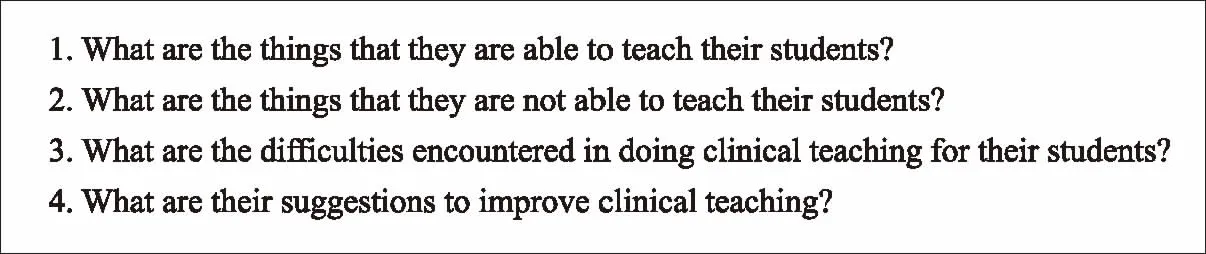
Figure 1. Open-ended questions for focus groups with staff nurses/clinical teachers
Data analysis
According to Grove et al[5], text is considered a rich source of data. Analyzing qualitative data occurred concurrently with the data collection, rather than sequentially as in quantitative data. All audio-taped data was transcribed and content analysis using triangulation technique applied. Three research assistants were asked to read the same transcript word by word and sentence by sentence independently and highlight the repeated words or sentences; they were also asked to make side notes for each paragraph, summarizing key points according to their understanding. Afterwards, principal researchers compared and integrated the results of the three assistants' analyses, which were then categorized.
Findings
The themes which were identified and used to describe the experiences of the twenty-seven staff nurses on duty while serving simultaneously as clinical teachers. The findings from the focus group discussion are presented as thick, rich data of the participants’ reflections of teaching in the clinical practicum, how they came to know the consequences of being a clinical teacher. There are four themes with thirteen subheadings. This is presented as the voices and perceptions of the clinical teachers as a participant observer. The categories containing similar contexts were combined, and main categories were formed. Lastly, the categorising process resulted in main and subcategories describing prerequisites (see Table 2).
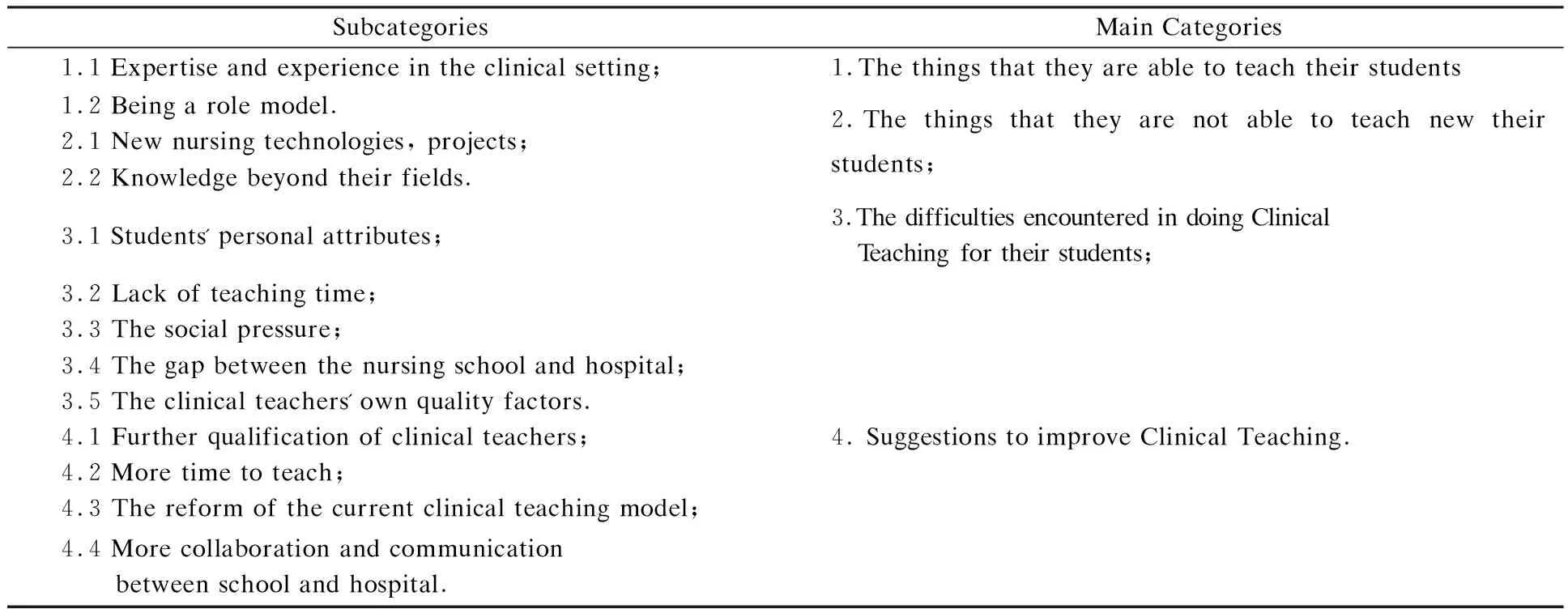
Table 2. The combination of focus group interviews in the data analysis and categorization process
Discussion
A view from the 27 clinical teachers/staff nurses included the roles they assumed, the associated responsibilities they encountered associated with those roles, and their personal concerns related to teaching in the clinical practicum. Their responses and narratives provided the detail and structure for each category and theme. Perspectives and images from within the world of the clinical teachers conveyed the elements of the clinical practicum. The clinical teacher as an architect of the clinical practicum develops the blueprint to plan for a solid teaching/ learning structure.
Thethingsthattheyareabletoteachtheirstudents
This theme reflects how knowledge is embedded in clinical practice and the importance of the clinical teacher being able to capture these moments to help students place learning within the context of the clinical setting. Supamanee et al[6]agreed that clinical teachers had the ability to expose nursing students to an effective clinical experience, which directly enhanced the development of confidence and competence.
Barker et al[7]stated that clinical teachers were considered the vital link between the concepts and evidence-based approaches to care and the realities of actual practice. Clinical teachers believed that being a role model in clinical education is the most effective and proper way for transmitting professional experiences and attitudes. Parsell et al[8]stated that the example set by the clinical teacher was the most powerful way for students to acquire the values, attitudes and behaviour needed for practice. It was important for clinical teachers to be role models with regard to teaching and thinking. As Zilembo et al[9]described the clinical teacher as a role model exhibiting behaviors that reflect the values and beliefs of the nursing profession.
Thethingsthattheyarenotabletoteachtheirstudents
Clinical teachers described the challenges they faced as they performed their roles. The continuous development of disciplines, the introduction of high-grade equipment and the continuous development of many new specialized nursing technologies and projects required the staff nurses/clinical teachers to improve their own quality constantly, to meet the requirements of nursing students, and to adapt the needs of the Times[10].
In addition, the staff nurses/clinical teachers' original education level is low, and with the development of the society, the nursing students' education level is becoming higher and higher. From 2010 to 2012, according to the Nursing Department, of the nursing students practicing in the hospital, 20% of them were from the technical secondary schools, 70% of them were from junior college and 10% of them were from the undergraduate course. However, the original education of the staff nurses/clinical teachers is uneven, 69% of have a technical secondary school education level and only 31% have a junior college or above degree level. It is common that a staff nurse/clinical teacher with a junior college education level is assigned to students with the bachelor education level, and a staff nurse/clinical teacher with a technical secondary school education level is assigned to a students with the junior or bachelor degree education level. This reveals the limited knowledge structure of the staff nurse/clinical teacher, who can't meet the further knowledge demand of nursing students, according to the perceptions of the participants.
ThedifficultiesencounteredindoingClinicalTeachingfortheirstudents
Clinical teachers described their frustrations with their students. According to a study done by Yu, Xu[4], about 70% students are the only child in the family as a result of China's one-child policy. Brought up in a prevailingly overprotective family environment, many of these graduates have demonstrated deficits in the affective domain of their development, such as in decision-making, conflict and ethical dilemma resolution, collaboration, delegation and leadership.
Participants however agreed that in most cases time did not allow for a detailed clinical teaching, because clinical teachers had their busy routines and schedules. A study by Diefenbeck et al[11]indicated that staff nurses naturally assumed a heavy responsibility in making precept for nursing students. The time and energy consumed in providing precept through monitoring and teaching greatly adds to the pressure on the overburdened and overworked nurse.
Joel[12]noted that: “The most meaningful change has been the growing strength and knowledge of the consumer.” Facing these social pressures, clinical teachers always view patient care as being of a higher priority to students’ education. According to the perceptions of clinical teachers, the learning environment in the clinical teaching area may not be as well controlled as desired owing to certain constraints. These constraints in the clinical milieu included students' lack of initiative and dedication, excessive workload, time constraints, social pressure and changes regarding the nursing school and hospital and tension between providing adequate knowledge and applying multiply teaching methods. Besides, the primary aim of Health Care centers is to provide quality health care to patients, with the student taking the role of a service provider. In addition, challenges included a lack of formal objectives from the student and not knowing what to expect from the students[7,11].
Suggestionstoimproveclinicalteaching
Most of the participants suggested that high quality clinical teachers are necessary for clinical teaching. In their opinions, enthusiasm and enjoyment of teaching were qualities of good teachers. This notion was echoed by Price et al[13]. In addition, it is better if the clinical teacher has working knowledge of different aspects of the curriculum. Meiring et al[14]identified this in 2013. The participants' emphasis on teachers’ ability to adapt to varying conditions and to draw on a wide educational repertoire also resembles findings by Kaviani et al[15].
In the clinical education programme, clinical teachers need to take cognizance of the important teaching-learning strategies. These may be easily integrated with various teaching-learning activities. Clinical teachers need more time to perform these programs. The clinical teachers elaborated on the aspect of time in the interviews, stating that sufficient time should be allocated for clinical teaching.
There seemed to be a conflicting role of the teacher as provider of information and knowledge, and yet at the same time as health care provider. In the current clinical model in China, clinical teachers valued approachability as the most important attribute of the clinical teacher. They stated that they try to assure approachability by making it clear that they (as teachers) are available and willing to help students. It is particularly important for clinical teachers not to appear to be threatening. But there are so many constants under the current clinical teaching model. They hoped a new model could be applied to the clinical setup.
For the clinical teaching structure, it is important to consider the views of the participants regarding the general clinical education structure as it provides a context for suggestions on teaching activities. Even though their responses might have been influenced by the fact that they were used to the current clinical teaching model, it should be noted that clinical teachers preferred to work in a new framework. It should be pointed out that their responses may not necessarily have reflected their preference, but it reflected their needs.
Otherwise, aspects of the school and hospital should be adequately sequenced and linked. Unified rules and processes need to be established by the school and the hospital. The relationship of nursing school and hospital is crucial in providing ongoing support. The contents of the communication between the two organizations are not only in the formulation of guidelines, but also in the standardization of teachers. The findings put emphasis on the strong link between school and hospital. They considered this kind of cooperation as a good beginning for the reform of clinical teaching.
The findings from the focus group discussions may guide clinical education for clinical teachers. It can do so by providing guidelines on clinical teaching. By suggesting a clinical teaching model as described above and by providing guidelines for teaching, clinical teaching may be made more consistent.
CONCLUSION
Reviewing the literature revealed the congruency to findings, which concluded that the clinical teacher's workload, lack of support from peers, and lack of time spent with the student negatively affected the role of the clinical teacher, leading to fatigue and burnout. The relationship between the clinical teachers and students can be challenging because of the clinical hours decided by clinical teachers. Clinical teachers play a vital role in supporting, teaching, supervising and assessing students in clinical settings as they transition to the graduate nurse role. These nurses are not able to meet the demands of the health care organization under the one-to-one relationship in recent years.
As a result, it is not clear what the staff nurses/clinical teachers utilize in China think of as being effective model in teaching the nursing students in clinical setting. Therefore, our qualitative study set out to determine the perceptions among the clinical teachers with regard to clinical teaching model.
The researchers have come up to the idea of a campaign on dissemination of information to these groups of clinical teachers rendering teaching to the nursing students in clinical setting in China. The current clinical teaching instruction in Philippines may be invited to further strengthen the importance of clinical teachers on teaching nursing students in China. A program maybe entitled “CP's Proposed Nursing Clinical Teaching Model” (Figure 2).
As shown in the Figure, a full-time faculty member, who is a clinical adviser prepared minimally at the bachelor's degree level, is responsible for the simultaneous supervision and oversight of clinical groups of nursing students, each group has two to four students. Before the nursing students exposure to clinical setting, they have been formed several groups by school. When they exposure to clinical setting, different groups are assigned to different units by hospital. Baccalaureate-prepared staff nurse in each unit, recognized by hospital as clinical teacher in this model, who provide direct clinical instruction to clinical groups in different units. The faculty-student ratio is from 1∶1 to 1∶2-4. A graduate/junior nurse will help to care for the patients while the clinical teacher is teaching. In effect, this arrangement allows the clinical teacher can have more time on clinical teaching.
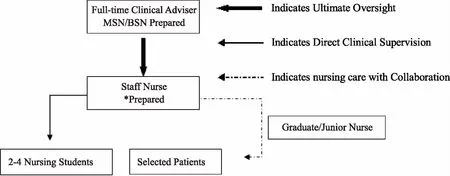
Fig 2. CP's Proposed Nursing Clinical Teaching Model
Introducing a new model of clinical teaching would need collaboration between the school and hospital, to ensure a smooth transition in implementing this long-awaited change. After this, further research is essential to assess its effectiveness.
[1] GABERSON K B, OERMANN M H. Clinical teaching strategies in nursing[M]. 4th Edition. New York: Springer Publishing Company, 2014.
[2] BURNS I, PATERSON I M. Clinical practice and placement support: supporting learning in practice.[J]. Nurse Educ Pract, 2005, 5(1): 3-9.
[3] XIE Y, YU L, ZHOU B. Comparative study on clinical practice training of nursing master degree education in some colleges and schools between in China and America[J]. Chinese Nurs Res, 2011, 75(2): 319-327.
[4] XU Y, XU Z M, ZHANG J, et al. Nursing Education Curriculum in Mainland China and the United States: a Comparative Perspective[J]. J Nurs Educ, 2002, 41(7): 310-316.
[5] GROVE S K, GRAY J, BURNS N. Understanding nursing research:building an evidence-based practice: building an evidence-based practice[M]. 6th ed. Philadelphia: Elsevier W. B. Saunders, 2015.
[6] SUPAMANEE T, KRAIRIKSH M, SINGHAKHUMFU L, et al. Preliminary clinical nursing leadership competency model: a qualitative study from Thailand[J]. Nurs Health Sci, 2011, 13(4): 433-439.
[7] BARKER E R, PITTMAN O. Becoming a super preceptor: a practical guide to preceptorship in today's clinical climate.[J]. J Am Acad Nurse Pract, 2010, 22(3): 144-149.
[8] PARSELL G, BLIGH J. Recent perspectives on clinical teaching.[J]. Med Educ, 2001, 35(4): 409-414.
[9] ZILEMBO M, MONTEROSSO L. Towards a conceptual framework for preceptorship in the clinical education of undergraduate nursing students[J]. Contemp Nurse, 2008, 30(1): 89-94.
[10] ZHOU Y H. The impact of nursing clinical teaching factors and countermeasures[J]. Chinese J Prac Nurs, 2003, 19 (1): 69.
[11] DIEFENBECK C A, PLOWFIELD L A, HERRMAN J W. Clinical immersion: a residency model for nursing education[J]. Nurs Educ Perspect, 2006, 27(2): 72-79.
[12] JOEL L. A, KELLY L. Y. The nursing experience: Trends, challenges, and transition[M]. 4th ed. New York: McGraw-Hill, 2002.
[13] PRICE A, PRICE B. Role modelling practice with students on clinical placements[J]. Nurs Stand, 2009, 24(11): 51-56.
[14] MEIRING A. THE IMAGE OF NURSES AS PERCEIVED BY THE SOUTH AFRICAN PUBLIC[J]. Africa J Nurs Midwifery, 2011, 15(2): 3-15.
[15] KAVIANI N, STILLWELL Y. An evaluative study of clinical preceptorship[J]. Nurse Educ Today, 2000, 20(3): 218-226.
 Journal of Clinical Nursing in Practice2018年4期
Journal of Clinical Nursing in Practice2018年4期
- Journal of Clinical Nursing in Practice的其它文章
- PDCA循环在提高危重症护理记录书写质量中的应用
- 膀胱肿瘤腹壁造口患者出院后的延续护理
- 规范化培训护士人文关怀能力影响因素调查分析
- 视频联合思维导图在行动静脉内瘘术患者健康教育中的应用
- LBL联合PBL教学法在呼吸内科临床带教中的应用
- 高危产妇配偶育儿胜任感现状及影响因素调查
