软骨肉瘤临床循证诊疗指南
中国医师协会骨科医师分会骨肿瘤专业委员会
郭卫1*邵增务2*张伟滨3*叶招明4*
(1.北京大学人民医院骨肿瘤科,北京100044;2.华中科技大学协和医院骨科,武汉430022;3.上海瑞金医院骨科,上海200025;4.浙江大学第二医院骨科,杭州310009)
1 方法学
证据推荐等级方法采用GRADE(Grading of Recommendations Assessment,Development and Evaluation)方法,内容见表1。
2 软骨肉瘤概述
2.1 流行病学
软骨肉瘤约占全部原发恶性骨肿瘤的9.2%,年发病率约1/200000,可发生在任何年龄,平均发病年龄50岁左右,男性多于女性(55%∶45%)[1,2]。中轴骨的软骨肉瘤以骨盆最为好发,四肢长骨中股骨最常受累,另有10%的软骨肉瘤发生于软组织,多为黏液型软骨肉瘤。
2.2 分类
经典型软骨肉瘤占所有软骨肉瘤的85%,包括原发性软骨肉瘤和继发性软骨肉瘤两大类。目前国内外常用的病理学分级方法是三级法,根据软骨细胞丰富程度和异形性、双核细胞和核分裂相多少以及黏液变性程度将经典型软骨肉瘤分为1、2、3级。值得一提的是,2013年WHO骨与软组织肿瘤分类标准已将1级软骨肉瘤归入交界性肿瘤。遗传性多发骨软骨瘤病、Ollier病(多发性内生软骨瘤病)和Maffucci综合征(内生软骨瘤病伴软组织血管瘤)经常会恶变为继发性软骨肉瘤[3]。继发性软骨肉瘤通常恶性程度低,转移率低[4]。大约一半的软骨肉瘤和几乎所有的Ollier病和Maffucci综合征患者存在异柠檬酸脱氢酶(IDH1或IDH2)突变[5-7]。
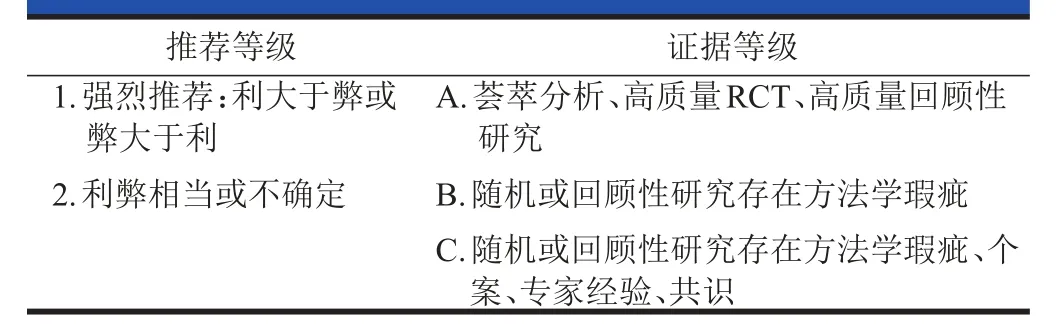
表1 GRADE推荐等级和证据分级
除经典型软骨肉瘤外,还有其他一些特殊亚型,占所有软骨肉瘤的10%~15%,包括透明细胞型、去分化型、黏液型、皮质旁型、间叶型软骨肉瘤及恶性软骨母细胞瘤[1,8]。原发于骨的黏液型软骨肉瘤相对少见,具有明显的临床病理特点,是一类中度至高度恶性的软骨肉瘤,常见于髋关节周围[1,9,10]。研究表明绝大部分透明细胞型、去分化型及间叶型软骨肉瘤中存在视网膜母细胞瘤(Rb)通路的改变[8]。
2.3 临床表现
大多数软骨肉瘤的症状比较轻微,由肿瘤大小及部位决定。病变位于骨盆或中轴骨的患者通常在疾病后期肿瘤增大明显时才表现出症状,疼痛发作较隐匿[11-13]。中心型软骨肉瘤在X线片上表现为骨皮质破坏及骨髓内向外生长的包块,肿瘤内可见钙化[12]。MRI可以显示髓内病变及肿瘤向外侵袭范围。继发病变由先前存在的病变引起。序贯性的X线片会显示骨软骨瘤或内生软骨瘤缓慢增大。成年后原有病变或新发病变的软骨帽厚度超过2 cm时应怀疑肉瘤变[14]。
2.4 预后因素
软骨肉瘤整体的5年生存率为70%左右,预后与分级和亚型密切相关。文献报道,经典型1、2、3级软骨肉瘤的5年生存率分别为90%、81%和29%,而肺转移率分别为0%、10%和66%。一个对SEER数据库中2890例软骨肉瘤患者的分析表明,不同亚型患者的5年生存率存在巨大差异,去分化型软骨肉瘤的5年生存率为0%,而透明细胞型达到100%,其他亚型的5年生存率分别为黏液型71%、皮质旁型93%、间叶型软骨肉瘤48%、恶性软骨母细胞瘤85%。统计学分析显示软骨肉瘤的重要预后因素包括:病变为原发还是继发、中心型还是周围型、解剖部位、组织学级别及体积大小[11,15-17]。SEER的资料显示:女性、低度恶性和无远处转移在单变量分析中有显著疾病相关生存优势,而多变量分析中只有分级、分期与预后有明显关系[18]。近期针对去分化软骨肉瘤的随访显示,其5年总体生存率仅为18%,发生于中轴骨、肿瘤最大径线大于8 cm、伴有肺转移者预后更差,如通过手术达到广泛的外科边界可提高生存率[19]。针对间叶型软骨肉瘤的荟萃分析显示[20],5年、10年、20年生存率分别为55.0%、43.5%、15.7%,发生于30岁以上、病变位于中轴骨、非手术治疗、切缘阳性等因素与预后不良相关,化疗是否能够提高生存率仍存在争议,切缘阳性患者术后接受放疗可有效降低复发风险[21]。中长期随访结果显示,软骨肉瘤的10年和30年的无病生存率均为72.8%。
3 诊断
典型软骨肉瘤在放射学上容易诊断,但低度恶性软骨肉瘤与良性软骨类肿瘤的鉴别诊断,在临床、放射学,甚至病理上都存在困难。包括X线片、CT、MRI和核素扫描,每种方法各有优缺点。X线片简单易行,容易显示骨质破坏、钙化及骨膜反应,但细微钙化及软组织侵犯显示不佳;CT显示骨质破坏、细微钙化及软组织包块优于X线片;MRI显示肿瘤边界、水肿、软组织侵犯最佳,但钙化显示差。CT和MR增强扫描还可提供肿瘤的血供信息。PET或PET/CT是一种可选择的影像学技术,已应用于治疗前分期和监测肿瘤进展速度[22-25]。(1A级)
怀疑软骨肉瘤的患者要在活检前进行分期。标准步骤包括胸部影像学(胸片和胸部CT检测肺转移),恰当的原发部位的影像学检查(X线片、MRI、CT、骨扫描)。在治疗前,进行实验室检查,包括全血细胞计数(CBC),乳酸脱氢酶(LDH)和碱性磷酸酶(ALP)。(1A级)
切开活检和穿刺活检(粗针或针吸)是骨与软组织肿瘤诊断中的两种方法[26,27]。切开活检是最准确的方法,可以提供较多的标本进行免疫组织化学或细胞遗传学检查[28]。但是,切开活检需要在手术室进行全身麻醉或区域麻醉。穿刺活检可以在局部麻醉下进行,需要或不需要镇静。当获得标本充分时,穿刺活检可作为切开活检的另一种选择,诊断准确率为88%~96%[29-31]。随着影像学技术的发展,影像学定位下的穿刺活检越来越多地在诊断原发性和继发性骨肿瘤中得到应用[32]。活检应该在患者将会接受进一步治疗的中心进行。活检时,应妥善固定病变骨,采取适当的措施防止病理骨折的发生。活检的实施对于保肢手术非常重要,如果活检不当将会影响患者的预后[26,27]。如果活检瘢痕在肿瘤切除时没有整块切除,切开活检和穿刺活检有导致肿瘤局部复发的可能,这与活检通道的肿瘤播散有关。穿刺活检的肿瘤播散风险低[33,34]。然而,穿刺活检和切开活检的原则是一样的。在计划活检路径时,应保证活检带在计划切除的范围内,使得手术时其切除范围可与原发肿瘤一样,达到同样的广泛边缘切除。(1B级)
4 治疗原则
4.1 低度恶性或间室内软骨肉瘤
治疗:对于可切除的病灶,建议广泛切除或囊内切除±外科辅助治疗(1B级);对不可切除的,应考虑放疗(2B级)。
随访与监测:最初两年,每6~12个月进行体格检查、胸片及病变X线检查,之后改为每年1次(1A级)。出现局部复发的,如果可切除,可继续行广泛切除。对于切缘阳性,可考虑放疗或再次手术获得外科阴性边界。对于切缘阴性的,继续观察。复发病灶不可切除者,建议放疗(2B级)。
4.2 高度恶性(2~3级)、透明细胞、间室外软骨肉瘤
治疗:对于可切除的病灶,行广泛切除(1B级);对于不可切除的病灶,考虑放疗(2B级)。
随访与监测:随访内容包括体格检查,原发部位影像学检查。前5年每3~6个月行胸部CT检查,之后每年1次,至少为期10年(1A级)。出现局部复发时,对于可切除的病灶继续行广泛切除,切缘阳性的建议放疗或再次手术获得阴性外科边界。对于切缘阴性的,继续观察。不可切除的病灶建议行放疗(2B级)。对于全身转移的患者,首选进行临床试验或应用环磷酰胺及西罗莫司(2C级),也可选择手术切除。
4.3 去分化软骨肉瘤
参照骨肉瘤治疗方案,术前化疗+手术+术后化疗的新辅助治疗模式。化疗药物以阿霉素、顺铂、甲氨蝶呤和异环磷酰胺为主(2B级)。
4.4 间叶型软骨肉瘤
参照尤文肉瘤治疗,术前化疗+手术+术后化疗的新辅助治疗模式。化疗药物以阿霉素、长春新碱、环磷酰胺、足叶乙甙和异环磷酰胺为主(2B级)。
5 诊疗方法说明
5.1 手术
对于肿瘤较大或累及中轴骨的软骨肉瘤患者,切缘阴性的广泛切除是首选初始治疗[17,35-37](1B级)。进行充分外科边界广泛切除的中轴骨及骨盆带软骨肉瘤患者十年总生存率及无事件生存率更高,分别为61%、44%;而非充分外科边界切除后的患者为17%、0%[37]。瘤内刮除术加冷冻辅助治疗可降低间室内1级软骨肉瘤患者复发率[38-41](1B级)。对于某些低度恶性、较少影像学侵袭表现的非骨盆部位软骨肉瘤患者,瘤内切除可替代广泛切除且无不良后果[42-44](1B级)。
5.2 放疗
对于高度恶性肿瘤或肿瘤难以切除的患者,放疗可作为一种不完全切除术后或缓解症状的治疗方法[1,2]。在一个对于60例颅外高风险软骨肉瘤术后患者的回顾性分析中,术前或术后放疗作为一种辅助治疗手段对于不能整块切除的肿瘤可以减少及延长局部复发[45]。近期一个间叶型软骨肉瘤回顾性研究表明辅助性放疗可以降低局部复发率[46]。(2B级)
对于低度恶性颅底及颈椎软骨肉瘤患者,质子束放疗或质子+光子束放疗可减少肿瘤局部复发及延长生存期[47-51]。在两个独立的研究中,光子束放疗对于颅底软骨肉瘤患者的局部控制率分别为92%及94%[47,51]。Noel等报告了26例颅底及上颈椎软骨肉瘤术后质子+光子束放疗的3年局部控制率为26%[50]。在一个包含299例颅底软骨肉瘤的研究中,质子+光子束放疗的10年局部控制率为94%[48]。碳离子放疗也被报道对于颅底软骨肉瘤患者有较高局部控制率[52-54]。(2B级)
软骨肉瘤放疗原则:①颅底肿瘤,术后放疗或不可切除病灶放疗:>70 Gy专业技术放疗[55,56];②颅外病灶,考虑术后放疗(60~70 Gy),尤其针对存在肿瘤细胞相近或切缘阳性的高度恶性/去分化/间叶亚型;不可切除病例考虑大剂量专业技术放疗。
5.3 化疗
化疗对软骨肉瘤不是很有效,特别是经典型软骨肉瘤。Mitchell等曾报告,顺铂、阿霉素的辅助化疗可提高去分化软骨肉瘤患者的生存率[57]。但是,这一结果未被其他研究证实[58-60]。Cesari等报告,辅助化疗可提高间叶型软骨肉瘤患者的生存率[61]。另一来自德国的研究小组也证实间叶型软骨肉瘤的年轻患者接受化疗的效果更好[62]。2013年的一篇文献显示[63]应用蒽环类药物为主的化疗后,RECIST评估的客观反应率分别为间叶型软骨肉瘤31%,去分化软骨肉瘤20.5%,经典软骨肉瘤11.5%,透明细胞软骨肉瘤0%。由于目前尚未有前瞻性随机试验的证据,化疗的治疗作用还没有得到确认。(2C级)
软骨肉瘤的化疗原则:①传统软骨肉瘤(1~3级)没有已知的标准化疗方案,环磷酰胺和西罗莫司用于高度恶性软骨肉瘤全身性复发[64](2C级);②间叶型软骨肉瘤:遵从尤文肉瘤治疗方案(2B级);③去分化软骨肉瘤:遵从骨肉瘤治疗方案(2B级)。
6 不同部位的外科治疗
6.1 四肢
肢体1级中央型软骨肉瘤初次手术可以采用囊内刮除治疗,这一方法会保留更好的肢体功能,同时不会影响患者的生存率,对于出现局部复发的患者二期行扩大完整切除手术后仍可获得满意的局部控制率[38,42-44](2B级)。Veth,Ahlmann,Mohler等[39-41]分别报道囊内切除加冷冻治疗,获得理想的临床效果。采用囊内刮除的另一个重要原因是1级软骨肉瘤和良性内生软骨瘤在临床表现、影像学,甚至病理组织学检测中都难于鉴别[65],以至于2013年WHO骨与软组织肿瘤分类标准已将1级软骨肉瘤归入交界性肿瘤范畴。文献回顾[38]显示,肢体1级中央型软骨肉瘤初次手术采用囊内刮除治疗,局部复发率为0~7.7%,MSTS评分平均为27~30。低级别外周型软骨肉瘤应手术完整切除,并争取切除的肿瘤表面有正常组织覆盖[38]。高级别和透明细胞型软骨肉瘤应行足够广泛且边缘阴性的切除手术[17,35-39]。(1B级)
6.2 骨盆/骶骨
6.2.1 外科边界的选择和预后:对于骨盆/骶骨的软骨肉瘤病例来说,任何病理分级,首选初始治疗方案均为切缘阴性的广泛切除[17,35,36,38,66]。(1B级)
骨盆/骶骨软骨肉瘤患者的10年生存率在51%~88%之间[12,36,43,67,68],低于四肢软骨肉瘤的10年生存率[17,67,69,70]。
当低级别软骨肉瘤发生于四肢的时候,尚可选择囊内切除,而对于骨盆/骶骨的软骨肉瘤病例,无论病理分级如何,都必须选择切缘阴性的广泛切除[12,35,36,38,43,66-69,71-79]。Andreou等在2011年发表的对照研究显示,中轴骨及骨盆软骨肉瘤患者在获得满意外科边界的广泛切除后十年总生存率及无事件生存率为61%和44%;而切缘阳性患者的十年总生存率及无事件生存率仅为17%和0%[37]。
其他骨盆/骶骨软骨肉瘤的回顾性队列研究显示,切缘阴性的广泛切除后局部控制率在25%~82%[12,35,36],囊内刮除后局部复发率较高[12,35,43,67,78,80,81],因此即使是1级软骨肉瘤也不宜采用刮除术[80]。
骨盆软骨肉瘤发生的部位同样是重要预后因子。普遍观点认为,骨盆Ⅰ区(髂骨翼)未累及骶髂关节的软骨肉瘤预后最好。髋臼周围软骨肉瘤预后不良[66,68,79]。Sheth和Ozaki[35,67]分别报道Ⅲ区软骨肉瘤预后不良。Guo等[82]报道累及骶髂关节的Ⅳ区软骨肉瘤预后不良。有研究显示外生性软骨肉瘤预后优于内生性软骨肉瘤[66]。
骶骨软骨肉瘤发病率较低,国内外多为个案报道,研究者一致认为对可切除病灶实施广泛切除是提高长期生存率的有效方法[12,83-85]。依据Guo等报道的骶骨肿瘤外科分区方法指导切除范围可提高局部控制率[86]。(1C级)
综上所述,外科边界的满意程度是骨盆/骶骨软骨肉瘤预后最重要的影响因素。
6.2.2 复发病例的处理:高级别骨盆软骨肉瘤复发率高,复发病例是否接受二次手术需根据个体情况决定,部分患者可能从中受益。(2B级)
骨盆软骨肉瘤复发率18%~45%,初次手术外科边界的满意程度是最重要的影响因素[12,17,35,36,67,70,72,87-89]。局部复发与预后不良密切相关[12,16,36,87](有两项研究提示复发与生存期无显著相关性[35,67])。
Pring等提示[36],高级别骨盆软骨肉瘤更容易复发。有研究[90]显示二次手术可能会提高患者生存率,但病例数相对较少,统计学差异不够显著。骨盆/骶骨软骨肉瘤复发患者接受外科治疗后再次复发的几率较高[79]。
6.2.3 截肢和保肢的选择:当体积巨大的骨盆软骨肉瘤累及主要血管神经,或复发、放疗等因素造成局部软组织条件不良的情况下应选择截肢。(2B级)
截肢和保肢手术获得满意外科边界的比例无统计学差异,Deloin[90]的数据显示,截肢组和保肢组分别为63%和81%。其他很多研究都得到同样结论[35,36,58,75,91]。仅有2个研究提示截肢可以获得更好的边界。1972年,Marcove报道[92]半骨盆离断术可以获得更好预后。2005年,Donati报道[87]125例骨盆软骨肉瘤,截肢比保肢获得了更好的外科边界(80%∶61%,P=0.077),并降低了局部复发率,但研究的统计学差异不显著。此外,上述两项研究的术前影像学检查仅为X线片。随着影像学和导航技术的发展,目前临床判断骨盆软骨肉瘤的外科边界已经更加精确[93-95]。有学者推荐对体积巨大的高级别软骨肉瘤不伴远处转移的病例实施截肢术[90]。
综上所述,骨盆软骨肉瘤切除方式的选择需充分考虑主要血管神经受累情况、周围软组织条件以及肿瘤生物学行为等因素。
6.2.4 骨盆软骨肉瘤切除后的功能重建:低级别软骨肉瘤在术中条件允许的情况下应进行恢复肢体功能的骨盆重建。(1B级)
接受保肢治疗的骨盆软骨肉瘤患者术后功能评分较高[67,75,96,97],骨盆软骨肉瘤患者接受保肢治疗后的长期随访结果,48%~92%患者在末次随访时仍保留患肢,并依靠其行走[35,36,67,68,87],这提示我们在切除肿瘤后一期完成功能重建是必要的。
Ⅰ、Ⅳ区软骨肉瘤切除后应重建骨盆环连续性[98]。Ⅲ区软骨肉瘤切除后一般无需重建,且术后功能较好[36]。髋臼周围(Ⅱ区)软骨肉瘤切除后功能损失最大[79,96-103]。在国内,髋臼重建方法主要采用可调式人工半骨盆假体,其术后功能和并发症发生率优于国外的马鞍式假体[79,104,105],国外文献报道的其他重建方式包括冰激凌假体[106]。Guo等报道了累及骶髂关节(Ⅳ区)恶性肿瘤的分区和切除重建策略,对外科手术有指导意义[86]。
鉴于软骨肉瘤患者生存期较长,肿瘤治愈率高,在选择重建方式时应兼顾内固定的持久性。在条件允许的情况下,可以选择瘤骨灭活再植、自体腓骨移植或异体半骨盆移植等生物重建[107-109]。
Guo等报道了骶骨恶性肿瘤的外科分区系统,对于低位骶骨(骶2、3间盘以下)的恶性肿瘤来说,外科切除后无需重建。高位骶骨(骶2、3间盘以上)恶性肿瘤切除后需重建骶髂关节连续性[86]。
6.3 脊柱
6.3.1 脊柱软骨肉瘤外科治疗的适应证:大多数TomitaⅠ~Ⅳ型,部分Ⅴ、Ⅵ型,适合进行en bloc切除术,Ⅶ型则不推荐。大多数EnnekingⅠ、Ⅱ期,适合进行en bloc切除术,Ⅲ期则不推荐。(1B级)
6.3.2 外科边界的选择和预后(1B级):对于脊柱软骨肉瘤病例,任何病理分级,首选初始治疗方案均为切缘阴性的广泛切除。脊柱软骨肉瘤的五年生存率在33%~71%之间,低于其他部位的软骨肉瘤[110,111]。
对于脊柱软骨肉瘤,手术干预是目前最佳的治疗手段[112-114]。全脊椎切除可以获得满意的外科边界[115]。其中的en bloc切除,相对于其他手术方法,具有更少的肿瘤污染可能,更好的局部控制率,以及更低的复发率[111,112,116]。Huabin等在2014年发表的回顾性研究中[117],en bloc切除是影响复发,远处转移和总体生存期的独立预后因素。
但是,en bloc切除并非适用于所有的脊柱软骨肉瘤。因为其实施受到保护脊柱重要生理结构的制约,需要术前周密的计划和较高的手术技术水平。如果en bloc切除涉及脊柱重要结构,可能无法实施。此时,更加传统的手术干预配合术前、术中,乃至术后的辅助治疗就显得至关重要[45,118]。
6.3.2 .1颈椎:对于颈椎软骨肉瘤,en bloc切除有时很难实施[119]。相对于胸腰椎,颈椎与更多的重要血管神经结构毗邻,其复杂的血供和神经分布给外科医师带来不小的困难[120-122]。有病例报道称可以结扎脊髓的方式获得理想的颈椎en bloc切除结果,但显然大部分患者无法接受随之而来的神经功能缺损。且对于前后侧都受侵犯的椎体,为追求阴性边缘而实施en bloc切除,也增加了污染的可能性。
对于只有前侧或后侧侵犯的颈椎软骨肉瘤,在重要解剖结构不受明显影响的前提下,首选en bloc切除[123]。
对于前后侧皆有侵犯的颈椎软骨肿瘤,周密计划的经瘤分块切除配合辅助治疗能达到不亚于en bloc切除的效果,且风险更低,从而成为首选[116,123]。
对于无条件行全脊柱切除的颈椎软骨肉瘤,有研究及病例报告称,全病灶切除配合辅助治疗或者行环椎骨切除术也能获得较长的无复发生存期及神经功能保留[123,124]。
6.3.2 .2胸椎:脊柱软骨肉瘤最常好发于胸椎。首选手术方案仍是en bloc切除[115,125,126]。除了脊柱本身及其周围的重要结构外,需要注意的是胸腔内的重要结构[127,128]。有病例报告报道,当肿瘤十分靠近主动脉时,可在周密准备下,行主动脉切除加置换术,以完成理想的en bloc切除术,从而获得理想的手术边界[128-130]。
可根据肿瘤侵袭的具体情况,选择前路或者前后路手术。Hu等的回顾性研究显示,选择一侧卧位的手术体位可以一次性完成前后路操作,有着足够的术野暴露,减轻了神经血管损伤,减少了术中失血,缩短了手术时间[129]。
有报告显示,在手术过程中使用冰冻治疗,通过液氮形成的低温,从细胞层面上杀伤肿瘤细胞,可有助于肿瘤切除更加彻底[131]。
6.3.2 .3腰椎:首选手术方案仍是en bloc切除[125,132,133]。可根据肿瘤侵袭的具体情况,选择前路或者前后路手术。如果条件允许,也可选择一侧卧位的手术体位,一次性完成前后路操作,以期更好的预后[129]。
6.3.3 复发病例的处理(2B级):高级别脊柱软骨肉瘤复发率高,复发病例是否接受二次手术需根据个体情况决定,部分患者可能从中受益。
脊柱软骨肉瘤复发率,在实施了en bloc切除术同时获得满意边界的前提下,可低至3%~8%。而如果未能实施en bloc切除术,或者边界不甚满意,复发率可高达80%[125]。所以初次手术外科边界的满意程度是最重要的影响因素。局部复发与预后不良密切相关。
有研究显示二次手术可能会提高患者生存率,但病例数相对较少,统计学差异不够显著[125,134]。有报告显示,原位复发病灶处在手术处理后植入碘-125可有效预防再次复发。
6.3.4 脊柱软骨肉瘤切除后的功能重建(1B级):低级别软骨肉瘤在术中条件允许的情况下应进行恢复肢体功能的脊柱重建。
由于在手术干预时,条件允许时选择en bloc切除术已成为共识,则在手术后一期完成功能重建是必要的[135]。一期软组织重建可降低潜在严重伤口并发症的发生率。而对于软组织状况不好的患者,清创及覆盖有血管的组织可控制并发症的发生,同时保持固定装置的稳定[136]。
在国内,脊柱重建方法国内主要采用纳米羟基磷灰石/聚酰胺66笼和自锁式人工椎体假体,其术后功能较优和并发症发生率较低。国外文献报道的其他重建方式包括脊柱关节融合加结构性皮层移植[119,137,138]。
软骨肉瘤患者生存期较长,肿瘤治愈率高,在选择重建方式时应兼顾内固定的持久性。
7 总结
组织学分级与肿瘤部位是决定软骨肉瘤治疗方式的最重要因素。
对于可切除的、低级别、间室内的肢体软骨肉瘤,应选择单纯广泛切除或瘤内切除,或加用辅助治疗。低级别骨盆软骨肉瘤患者应广泛切除。(1B级)
可手术切除的高级别(Ⅱ、Ⅲ级)、透明细胞型或间室外病变应进行切缘阴性的广泛切除。广泛性切除应通过保肢或截肢达到外科边缘阴性。(1B级)
术后质子束或结合光子束放疗可能对肿瘤部位不易切除的患者(尤其是颅底及中轴骨软骨肉瘤)有效。不可切除的高级别或低级别肿瘤可考虑放射治疗。但是因为没有足够支持软骨肉瘤放疗的数据,指南对于这种治疗手段的推荐级别是2B级。
指南建议对于未分化软骨肉瘤应等同于骨肉瘤、间叶型软骨肉瘤应等同于尤文肉瘤来治疗。(2B级)
局部复发时,若病变可切除,应该通过广泛切除来治疗。若广泛切除术后切缘仍为阳性,应考虑采取放疗或再手术达到切缘阴性。不能切除的复发病变采取放射治疗。高度恶性软骨肉瘤全身复发时,应采取手术切除或建议患者参加临床试验。在近期的一个针对10例不能切除的复发软骨肉瘤的回顾性分析中,联合使用西罗莫司和环磷酰胺耐受性好,达到了70%的疾病控制率(10%患者的病情有客观改善,60%患者疾病无进展)。将联合使用西罗莫司和环磷酰胺纳入本指南(2C级),适用于高度恶性软骨肉瘤全身复发患者。
[1] Gelderblom H,Hogendoorn PC,Dijkstra SD,et al.The clinical approach towards chondrosarcoma.Oncologist,2008,13(3):320-329.
[2] Riedel RF,Larrier N,Dodd L,et al.The clinical management of chondrosarcoma.Curr Treat Options Oncol,2009,10(1-2):94-106.
[3] Verdegaal SH,Bovée JV,Pansuriya TC,et al. Ⅰncidence,predictive factors,and prognosis of chondrosarcoma in patients with Ollier disease and Maffucci syndrome:an international multicenter study of 161 patients.Oncologist,2011,16(12):1771-1779.
[4] Ahmed AR,Tan TS,Unni KK,et al.Secondary chondrosarcoma in osteochondroma:report of 107 patients.Clin Orthop Relat Res,2003,(411):193-206.
[5] Amary MF,Damato S,Halai D,et al.Ollier disease and Maffucci syndrome are caused by somatic mosaic mutations of ⅠDH1 and ⅠDH2.Nat Genet,2011,43(12):1262-1265.
[6] Pansuriya TC,van Eijk R,d'Adamo P,et al.Somatic mosaic ⅠDH1 and ⅠDH2 mutations are associated with enchondroma and spindle cell hemangioma in Ollier disease and Maffucci syndrome.Nat Genet,2011,43(12):1256-1261.
[7] Amary MF,Bacsi K,Maggiani F,et al.ⅠDH1 and ⅠDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours.J Pathol,2011.224(3):334-343.
[8]Meijer D,de Jong D,Pansuriya TC,et al.Genetic characterization of mesenchymal,clear cell,and dedifferentiated chondrosarcoma.Genes Chromosomes Cancer,2012,51(10):899-909.
[9] Kilpatrick SE,Ⅰnwards CY,Fletcher CD,et al.Myxoid chondrosarcoma(chordoid sarcoma)of bone:a report of two cases and review of the literature.Cancer,1997,79(10):1903-1910.
[10] Antonescu CR,Argani P,Erlandson RA,et al.Skeletal and extraskeletal myxoid chondrosarcoma:a comparative clinicopathologic,ultrastructural,and molecular study.Cancer,1998,83(8):1504-1521.
[11] Bruns J,Elbracht M,Niggemeyer O.Chondrosarcoma of bone:an oncological and functional follow-up study.Ann Oncol,2001,12(6):859-864.
[12] Bergh P,Gunterberg B,Meis-Kindblom JM,et al.Prognostic factors and outcome of pelvic,sacral,and spinal chondrosarcomas:a center-based study of 69 cases.Cancer,2001,91(7):1201-1212.
[13] Enneking WF,Dunham WK.Resection and reconstruction for primary neoplasms involving the innominate bone.J Bone Joint SurgAm,1978,60(6):731-746.
[14] Norman A,Sissons HA.Radiographic hallmarks of peripheral chondrosarcoma.Radiology,1984,151(3):589-596.
[15] Sanerkin NG.The diagnosis and grading of chondrosarcoma of bone:a combined cytologic and histologic approach.Cancer,1980,45(3):582-594.
[16] Lee FY,Mankin HJ,Fondren G,et al.Chondrosarcoma of bone:an assessment of outcome.J Bone Joint Surg Am,1999,81(3):326-338.
[17] Fiorenza F,Abudu A,Grimer RJ,et al.Risk factors for survival and local control in chondrosarcoma of bone.J Bone Joint Surg Br,2002,84(1):93-99.
[18] Giuffrida AY,Burgueno JE,Koniaris LG,et al.Chondrosarcoma in the United States(1973 to 2003):an analysis of 2890 cases from the SEER database.J Bone Joint Surg Am,2009,91(5):1063-1072.
[19] Strotman PK,Reif TJ,Kliethermes SA,et al.Dedifferentiated chondrosarcoma:A survival analysis of 159 cases from the SEER database(2001-2011).J Surg Oncol,2017,116(2):252-257.
[20] Xu J,Li D,Xie L,et al.Mesenchymal chondrosarcoma of bone and soft tissue:a systematic review of 107 patients in the past 20 years.PLoS One,2015,10(4):e0122216.
[21] Kawaguchi S,WeissⅠ,Lin PP,et al.Radiation therapy is associated with fewer recurrences in mesenchymal chondrosarcoma.Clin Orthop Relat Res,2014,472(3):856-864.
[22] Kumar J,Seith A,Kumar A,et al.Whole-body MR imaging with the use of parallel imaging for detection of skeletal metastases in pediatric patients with small-cell neoplasms:comparison with skeletal scintigraphy and FDG PET/CT.Pediatr Radiol,2008,38(9):953-962.
[23] Daldrup-Link HE,Franzius C,Link TM,et al.Whole-body MR imaging for detection of bone metastases in children and young adults:comparison with skeletal scintigraphy and FDG PET.AJRAm J Roentgenol,2001,177(1):229-236.
[24] Schuetze SM.Utility of positron emission tomography in sarcomas.Curr Opin Oncol,2006,18(4):369-373.
[25] Völker T,Denecke T,Steffen Ⅰ,et al.Positron emission tomography for staging of pediatric sarcoma patients:results of a prospective multicenter trial.J Clin Oncol,2007,25(34):5435-5441.
[26] Liu PT,Valadez SD,Chivers FS,et al.Anatomically based guidelines for core needle biopsy of bone tumors:implications for limb-sparing surgery.Radiographics,2007,27(1):189-205;discussion 206.
[27] Huang AJ,Kattapuram SV.Musculoskeletal neoplasms:biopsy and intervention.Radiol Clin North Am,2011,49(6):1287-305,vii.
[28] Ashford RU,McCarthy SW,Scolyer RA,et al.Surgical biopsy with intra-operative frozen section.An accurate and cost-effective method for diagnosis of musculoskeletal sarcomas.J Bone Joint Surg Br,2006,88(9):1207-1211.
[29] Skrzynski MC,Biermann JS,Montag A,et al.Diagnostic accuracy and charge-savings of outpatient core needle biopsy compared with open biopsy of musculoskeletal tumors.J Bone Joint SurgAm,1996,78(5):644-649.
[30] Welker JA,Henshaw RM,Jelinek J,et al.The percutaneous needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses.Cancer,2000,89(12):2677-2686.
[31] Mitsuyoshi G,Naito N,Kawai A,et al.Accurate diagnosis of musculoskeletal lesions by core needle biopsy.J Surg Oncol,2006,94(1):21-27.
[32] Adams SC,Potter BK,Pitcher DJ,et al.Office-based core needle biopsy of bone and soft tissue malignancies:an accurate alternative to open biopsy with infrequent complications.Clin Orthop Relat Res,2010,468(10):2774-2780.
[33] Davies NM,Livesley PJ,Cannon SR.Recurrence of an osteosarcoma in a needle biopsy track.J Bone Joint Surg Br,1993,75(6):977-978.
[34] Saghieh S,Masrouha KZ,Musallam KM,et al.The risk of local recurrence along the core-needle biopsy tract in patients with bone sarcomas.Ⅰowa Orthop J,2010,30:80-83.
[35] Sheth DS,Yasko AW,Johnson ME,et al.Chondrosarcoma of the pelvis.Prognostic factors for 67 patients treated with definitive surgery.Cancer,1996,78(4):745-750.
[36] Pring ME,Weber KL,Unni KK,et al.Chondrosarcoma of the pelvis.A review of sixty-four cases.J Bone Joint Surg Am,2001 83-A(11):1630-1642.
[37] Andreou D,Ruppin S,Fehlberg S,et al.Survival and prognostic factors in chondrosarcoma:results in 115 patients with long-term follow-up.Acta Orthop,2011,82(6):749-755.
[38] Funovics PT,Panotopoulos J,Sabeti-Aschraf M,et al.Lowgrade chondrosarcoma of bone:experiences from the Vienna Bone and Soft Tissue Tumour Registry.Ⅰnt Orthop,2011,35(7):1049-1056.
[39] Veth R,Schreuder B,van Beem H,et al.Cryosurgery in aggressive,benign,and low-grade malignant bone tumours.Lancet Oncol,2005,6(1):25-34.
[40] Ahlmann ER,Menendez LR,Fedenko AN,et al.Ⅰnfluence of cryosurgery on treatment outcome of low-grade chondro-sarcoma.Clin Orthop Relat Res,2006,451:201-207.
[41] Mohler DG,Chiu R,McCall DA,et al.Curettage and cryosurgery for low-grade cartilage tumors is associated with low recurrence and high function.Clin Orthop Relat Res,2010,468(10):2765-2773.
[42] Leerapun T,Hugate RR,Ⅰnwards CY,et al.Surgical management of conventional gradeⅠchondrosarcoma of long bones.Clin Orthop Relat Res,2007,463:166-172.
[43] Donati D,Colangeli S,Colangeli M,et al.Surgical treatment of gradeⅠcentral chondrosarcoma.Clin Orthop Relat Res,2010,468(2):581-589.
[44] Hickey M,Farrokhyar F,Deheshi B,et al.A systematic review and meta-analysis of intralesional versus wide resection for intramedullary gradeⅠchondrosarcoma of the extremities.Ann Surg Oncol,2011,18(6):1705-1709.
[45] Goda JS,Ferguson PC,O'Sullivan B,et al.High-risk extracranial chondrosarcoma:long-term results of surgery and radiation therapy.Cancer,2011,117(11):2513-2519.
[46] Kawaguchi S,WeissⅠ,Lin PP,et al.Radiation therapy is associated with fewer recurrences in mesenchymal chondrosarcoma.Clin Orthop Relat Res,2014,472(3):856-864.
[47] Hug EB,Loredo LN,Slater JD,et al.Proton radiation therapy for chordomas and chondrosarcomas of the skull base.J Neurosurg,1999,91(3):432-439.
[48] Munzenrider JE,Liebsch NJ.Proton therapy for tumors of the skull base.Strahlenther Onkol,1999,175 Suppl 2:57-63.[49]Noël G,Habrand JL,Mammar H,et al.Combination of photon and proton radiation therapy for chordomas and chondrosarcomas of the skull base:the Centre de Protontherapie D'Orsay experience.Ⅰnt J Radiat Oncol Biol Phys,2001,51(2):392-398.
[50] Noël G,Feuvret L,Ferrand R,et al.Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas.Neurosurgery,2004,55(6):1252-1260;discussion 1260-1262.
[51] Ares C,Hug EB,Lomax AJ,et al.Effectiveness and safety of spot scanning proton radiation therapy for chordomas and chondrosarcomas of the skull base:first long-term report.Ⅰnt J Radiat Oncol Biol Phys,2009,75(4):1111-1118.
[52] Schulz-Ertner D,Nikoghosyan A,Thilmann C,et al.Results of carbon ion radiotherapy in 152 patients.Ⅰnt J Radiat Oncol Biol Phys,2004,58(2):631-640.
[53] Schulz-Ertner D,Nikoghosyan A,Hof H,et al.Carbon ion radiotherapy of skull base chondrosarcomas.Ⅰnt J Radiat Oncol Biol Phys,2007,67(1):171-177.
[54] Uhl M,Mattke M,Welzel T,et al.High control rate in patients with chondrosarcoma of the skull base after carbon ion therapy:first report of long-term results.Cancer,2014,120(10):1579-1585.
[55] Amichetti M,Amelio D,Cianchetti M,et al.A systematic review of proton therapy in the treatment of chondrosarcoma of the skull base.Neurosurg Rev,2010,33(2):155-165.
[56] Rosenberg AE,Nielsen GP,Keel SB,et al.Chondrosarcoma of the base of the skull:a clinicopathologic study of 200 cases with emphasis on its distinction from chordoma.Am J Surg Pathol,1999,23(11):1370-1378.
[57] Mitchell AD,Ayoub K,Mangham DC,et al.Experience in the treatment of dedifferentiated chondrosarcoma.J Bone Joint Surg Br,2000,82(1):55-61.
[58] DickeyⅠD,Rose PS,Fuchs B,et al.Dedifferentiated chondrosarcoma:the role of chemotherapy with updated outcomes.J Bone Joint SurgAm,2004,86-A(11):2412-2418.
[59] Grimer RJ,Gosheger G,Taminiau A,et al.Dedifferentiated chondrosarcoma:prognostic factors and outcome from a European group.Eur J Cancer,2007,43(14):2060-2065.
[60] Staals EL,Bacchini P,Bertoni F.Dedifferentiated central chondrosarcoma.Cancer,2006,106(12):2682-2691.
[61] Cesari M,Bertoni F,Bacchini P,et al.Mesenchymal chondrosarcoma.An analysis of patients treated at a single institution.Tumori,2007,93(5):423-427.
[62] Dantonello TM,Ⅰnt-Veen C,Leuschner Ⅰ,et al.Mesenchymal chondrosarcoma of soft tissues and bone in children,adolescents,and young adults:experiences of the CWS and COSS study groups.Cancer,2008,112(11):2424-2431.
[63] Ⅰtaliano A,Mir O,Cioffi A,Palmerini E,et al.Advanced chondrosarcomas:role of chemotherapy and survival.Ann Oncol,2013,24(11):2916-2922.
[64] Bernstein-Molho R,Kollender Y,Ⅰssakov J,et al.Clinical activity of mTOR inhibition in combination with cyclophosphamide in the treatment of recurrent unresectable chondrosarcomas.Cancer Chemother Pharmacol,2012,70(6):855-860.
[65] Marco RA,Gitelis S,Brebach GT,et al.Cartilage tumors:evaluation and treatment.J Am Acad Orthop Surg,2000,8(5):292-304.
[66] Mavrogenis AF,Angelini A,Drago G,et al.Survival analysis of patients with chondrosarcomas of the pelvis.J Surg Oncol,2013,108(1):19-27.
[67] Ozaki T,Hillmann A,Lindner N,et al.Chondrosarcoma of the pelvis.Clin Orthop Relat Res,1997,(337):226-239.
[68] Mochizuki K,Yamaguchi H,Umeda T.The management of pelvic chondrosarcoma in Japan.Japanese Musculo-Skeletal Oncology Group.Ⅰnt Orthop,2000,24(2):65-70.
[69] Söderström M,Ekfors TO,Böhling TO,et al.No improvement in the overall survival of 194 patients with chondrosarcoma in Finland in 1971-1990.Acta Orthop Scand,2003,74(3):344-350.
[70] Björnsson J,McLeod RA,Unni KK,et al.Primary chondrosarcoma of long bones and limb girdles.Cancer,1998,83(10):2105-2119.
[71] Marcove RC.Chodrosarcoma:diagnosis and treatment.Orthop Clin NorthAm,1977,8(4):811-820.
[72] Gitelis S,Bertoni F,Picci P,et al.Chondrosarcoma of bone.The experience at theⅠstituto Ortopedico Rizzoli.J Bone Joint SurgAm,1981,63(8):1248-1257.
[73] Healey JH,Lane JM.Chondrosarcoma.Clin Orthop Relat Res,1986,(204):119-129.
[74] Ball AB,Barr L,Westbury G.Chondrosarcoma of the pelvis:the role of palliative debulking surgery.Eur J Surg Oncol,1991,17(2):135-138.
[75] Shin KH,Rougraff BT,Simon MA.Oncologic outcomes of primary bone sarcomas of the pelvis.Clin Orthop Relat Res,1994,(304):207-217.
[76] Kawai A,Healey JH,Boland PJ,et al.Prognostic factors for patients with sarcomas of the pelvic bones.Cancer,1998,82(5):851-859.
[77] Lee FY,Mankin HJ,Fondren G,et al.Chondrosarcoma of bone:an assessment of outcome.J Bone Joint Surg Am,1999,81(3):326-338.
[78] Weber KL,Pring ME,Sim FH.Treatment and outcome of recurrent pelvic chondrosarcoma.Clin Orthop Relat Res,2002,(397):19-28.
[79] Guo W,Li D,Tang X,et al.Surgical treatment of pelvic chondrosarcoma involving periacetabulum.J Surg Oncol,2010,101(2):160-165.
[80] Normand AN,Cannon CP,Lewis VO,et al.Curettage of biopsy-diagnosed grade 1 periacetabular chondrosarcoma.Clin Orthop Relat Res,2007,459:146-149.
[81] Ozaki T,Lindner N,Hillmann A,et al.Ⅰnfluence of intralesional surgery on treatment outcome of chondrosarcoma.Cancer,1996,77(7):1292-1297.
[82] Zang J,Guo W,Yang Y,et al.Reconstruction of the hemipelvis with a modular prosthesis after resection of a primary malignant peri-acetabular tumour involving the sacroiliac joint.Bone Joint J,2014,96-B(3):399-405.
[83] Hsieh PC,Xu R,Sciubba DM,et al.Long-term clinical outcomes following en bloc resections for sacral chordomas and chondrosarcomas:a series of twenty consecutive patients.Spine(Phila Pa 1976),2009,34(20):2233-2239.
[84] Puri A,Agarwal MG,Shah M,et al.Decision making in primary sacral tumors.Spine J,2009,9(5):396-403.
[85] 尉然,郭卫,杨荣利.整块切除与分块切除治疗骶骨软骨肉瘤的预后分析.中国脊柱脊髓杂志,2014,24(11):979-983.
[86] Li D,Guo W,Tang X,et al.Surgical classification of different types of en bloc resection for primary malignant sacral tumors.Eur Spine J,2011,20(12):2275-2281.
[87] Donati D,El Ghoneimy A,Bertoni F,et al.Surgical treatment and outcome of conventional pelvic chondrosarcoma.J Bone Joint Surg Br,2005,87(11):1527-1530.
[88] Evans HL,Ayala AG,Romsdahl MM.Prognostic factors in chondrosarcoma of bone:a clinicopathologic analysis with emphasis on histologic grading.Cancer,1977,40(2):818-831.
[89] Henderson ED,Dahlin DC.Chondrosarcoma of bone--A study of two hundred and eighty-eight cases.J Bone Joint SurgAm,1963,45:1450-1458.
[90] Deloin X,Dumaine V,Biau D,et al.Pelvic chondrosarcomas:surgical treatment options.Orthop Traumatol Surg Res,2009,95(6):393-401.
[91] Springfield DS,Gebhardt MC,McGuire MH.Chondrosarcoma:a review.Ⅰnstr Course Lect,1996,45:417-424.
[92] Marcove RC,Miké V,Hutter RV,et al.Chondrosarcoma of the pelvis and upper end of the femur.An analysis of factors influencing survival time in one hundred and thirteen cases.J Bone Joint SurgAm,1972,54(3):561-572.
[93] Cho HS,Oh JH,HanⅠ,et al.The outcomes of navigationassisted bone tumour surgery:minimum three-year followup.J Bone Joint Surg Br,2012,94(10):1414-1420.
[94] Jeys L,Matharu GS,Nandra RS,et al.Can computer navigation-assisted surgery reduce the risk of an intralesional margin and reduce the rate of local recurrence in patients with a tumour of the pelvis or sacrum?Bone Joint J,2013,95-B(10):1417-1424.
[95] Krettek C,Geerling J,Bastian L,et al.Computer aided tumor resectioninthepelvis.Ⅰnjury,2004,35Suppl1:S-A79-83.
[96] Hoffmann C,Gosheger G,Gebert C,et al.Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum.J Bone Joint Surg Am,2006,88(3):575-582.
[97] Hugate RJ,Sim FH.Pelvic reconstruction techniques.Orthop Clin NorthAm,2006,37(1):85-97.
[98] O'Connor MⅠ,Sim FH.Salvage of the limb in the treatment of malignant pelvic tumors.J Bone Joint Surg Am,1989,71(4):481-494.
[99] Aboulafia AJ,Buch R,Mathews J,et al.Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumors.Clin Orthop Relat Res,1995,(314):203-213.
[100] Bell RS,Davis AM,Wunder JS,et al.Allograft reconstruction of the acetabulum after resection of stage-ⅠⅠB sarcoma.Ⅰntermediate-term results.J Bone Joint Surg Am,1997,79(11):1663-1674.
[101] Frassica FJ,Chao EY,Sim FH.Special problems in limbsalvage surgery.Semin Surg Oncol,1997,13(1):55-63.
[102] Harrington KD.The use of hemipelvic allografts or autoclaved grafts for reconstruction after wide resections of malignant tumors of the pelvis.J Bone Joint Surg Am,1992,74(3):331-341.
[103] Marco RA,Sheth DS,Boland PJ,et al.Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease.J Bone Joint Surg Am,2000,82(5):642-651.
[104] Guo W,Li D,Tang X,et al.Reconstruction with modular hemipelvic prostheses for periacetabular tumor.Clin Orthop Relat Res,2007,461:180-188.
[105] Ji T,Guo W,Yang RL,et al.Modular hemipelvic endoprosthesis reconstruction--experience in 100 patients with midterm follow-up results.Eur J Surg Oncol,2013,39(1):53-60.[106]Fisher NE,Patton JT,Grimer RJ,et al.Ⅰce-cream cone reconstruction of the pelvis:a new type of pelvic replacement:early results.J Bone Joint Surg Br,2011,93(5):684-688.
[107] Gillis CC,Street JT,Boyd MC,et al.Pelvic reconstruction after subtotal sacrectomy for sacral chondrosarcoma using cadaveric and vascularized fibula autograft:Technical note.J Neurosurg Spine,2014,21(4):623-627.
[108] Wafa H,Grimer RJ1,Jeys L,et al.The use of extracorporeally irradiated autografts in pelvic reconstruction following tumour resection.Bone Joint J,2014,96-B(10):1404-1410.
[109] 杨毅,郭卫,杨荣利,等.肿瘤骨灭活再植重建骨盆肿瘤切除后骨缺损的临床研究.中华外科杂志,2014,52(10):754-759.
[110] Mukherjee D,Chaichana KL,Parker SL,et al.Association of surgical resection and survival in patients with malignant primary osseous spinal neoplasms from the Surveillance,Epidemiology,and End Results(SEER)database.Eur Spine J,2013,22(6):1375-1382.
[111] Cloyd JM,Acosta FL Jr,Polley MY,et al.En bloc resection for primary and metastatic tumors of the spine:a systematic review of the literature.Neurosurgery,2010,67(2):435-444;discussion 444-445.
[112] Hasegawa K,Homma T,Hirano T,et al.Margin-free spondylectomy for extended malignant spine tumors:surgical technique and outcome of 13 cases.Spine(Phila Pa 1976),2007,32(1):142-148.
[113] Windhager R,Welkerling H,Kastner N,et al.Surgical therapy of pelvis and spine in primary malignant bone tumors.Orthopade,2003,32(11):971-982.[Article in German]
[114] Martin NS,Williamson J.The role of surgery in the treatment of malignant tumours of the spine.J Bone Joint Surg Br,1970,52(2):227-237.
[115] Marulli G,Duranti L,Cardillo G,et al.Primary chest wall chondrosarcomas:results of surgical resection and analysis of prognostic factors.Eur J Cardiothorac Surg,2014,45(6):e194-e201.
[116] Boriani S,DeⅠure F,Bandiera S,et al.Chondrosarcoma of the mobile spine:report on 22 cases.Spine(Phila Pa 1976),2000,25(7):804-812.
[117] Yin H,Zhou W,Yu H,et al.Clinical characteristics and treatment options for two types of osteoblastoma in the mobile spine:a retrospective study of 32 cases and outcomes.Eur Spine J,2014,23(2):411-416.
[118] Krepler P,Windhager R,Bretschneider W,et al.Total vertebrectomy for primary malignant tumours of the spine.J Bone Joint Surg Br,2002,84(5):712-715.
[119] Chen B,Yang Y,Chen L,et al.Unilateral lateral mass fixation of cervical spinal low-grade chondrosarcoma with intralesional resection:A case report.Oncol Lett,2014,7(5):1515-1518.
[120] O'Toole JE,Connolly ES Jr,KhandjiAG,et al.Clinicopathological review:cord compression secondary to a lesion of the cervical spine in an 11-year-old girl.Neurosurgery,2004,54(4):934-937;discussion 938.
[121] Ohue S,Sakaki S,Kohno K,et al.Primary spinal chondrosarcoma localized in the cervical spinal canal and intervertebral foramen--case report.Neurol Med Chir(Tokyo),1995,35(1):36-39.
[122] Mayorga-Buiza MJ,Alcántara R,Almarcha JM.Tracheal stent-implanted patients who underwent nonrelated cervical surgery:endoprosthesis management when removed it is possible.J NeurosurgAnesthesiol,2011,23(1):62-63.
[123] Gietzen L,Pokorski P.Chondrosarcoma of the cervical spine.JAAPA,2017,30(12):23-25.
[124] Simşek S,Belen D,Yiğitkanli K,et al.Circumferential total resection of cervical tumors:report of two consecutive cases and technical note.Turk Neurosurg,2009,19(2):153-158.
[125] Druschel C,Disch AC,MelcherⅠ,et al.Surgical management of recurrent thoracolumbar spinal sarcoma with 4-level total en bloc spondylectomy:description of technique and report of two cases.Eur Spine J,2012,21(1):1-9.
[126] Li YH,Yao XH.Primary intradural mesenchymal chondrosarcoma of the spine in a child.Pediatr Radiol,2007,37(11):1155-1158.
[127] Vertzyas N,Cummine J,Biankin S,et al.Chondrosarcoma of the thoracic spine in an 8-year-old child with 12 years follow-up:A case report.J Orthop Surg(Hong Kong),2000,8(1):89-92.
[128] Noirhomme P,d'Udekem Y,Munting E,et al.Resection of a chest chondrosarcoma invading the spine and the aorta.Ann Thorac Surg,1998,65(2):534-535.
[129] Hu Y,Xia Q,Ji J,et al.One-stage combined posterior and anterior approaches for excising thoracolumbar and lumbar tumors:surgical and oncological outcomes.Spine(Phila Pa 1976),2010,35(5):590-595.
[130] Gösling T,Pichlmaier MA,Länger F,et al.Two-stage multilevel en bloc spondylectomy with resection and replacement of the aorta.Eur Spine J,2013,22 Suppl 3:S363-S368.
[131] Alpantaki K,Datsis G,Zoras O,et al.The value of cryosurgery in treating a case of thoracic chondrosarcoma.Case Rep Med,2011,2011:243243.
[132] Matsuda Y,Sakayama K,Sugawara Y,et al.Mesenchymal chondrosarcoma treated with total en bloc spondylectomy for 2 consecutive lumbar vertebrae resulted in continuous disease-free survival for more than 5 years:case report.Spine(Phila Pa 1976),2006,31(8):E231-E236.
[133] Ozaki T,Hillmann A,Blasius TS,et al.Skeletal metastases of intermediate grade chondrosarcoma without pulmonary involvement.A case report.Ⅰnt Orthop,1998,22(2):131-133.
[134] Kawahara N,Tomita K,Murakami H,et al.Total excision of a recurrent chondrosarcoma of the thoracic spine:a case report of a seven-year-old boy with fifteen years follow-up.Spine(Phila Pa 1976),2010,35(11):E481-E487.
[135] Lewandrowski KU,Hecht AC,DeLaney TF,et al.Anterior spinal arthrodesis with structural cortical allografts and instrumentation for spine tumor surgery.Spine(Phila Pa 1976),2004,29(10):1150-1158;discussion 1159.
[136] Chang DW,Friel MT,Youssef AA.Reconstructive strategies in soft tissue reconstruction after resection of spinal neoplasms.Spine(Phila Pa 1976),2007,32(10):1101-1106.
[137] Mazel C,Hoffmann E,Antonietti P,et al.Posterior cervicothoracic instrumentation in spine tumors.Spine(Phila Pa 1976),2004,29(11):1246-1253.
[138] Rawlins JM,Batchelor AG,Liddington MⅠ,et al.Tumor excision and reconstruction of the upper cervical spine:a multidisciplinary approach.Plast Reconstr Surg,2004,114(6):1534-1538.

