骨巨细胞瘤临床循证诊疗指南
中国医师协会骨科医师分会骨肿瘤专业委员会
郭卫1*李建民2*沈靖南3*屠重棋4*
(1.北京大学人民医院骨肿瘤科,北京100044;2.山东大学齐鲁医院骨科,济南250012;3.中山大学第一附属医院骨科,广州510080;4.四川大学华西医院骨科,成都610041)
1 方法学
证据推荐等级方法采用GRADE(Grading of Recommendations Assessment,Development and Evaluation)方法,内容见表1。
2 骨巨细胞瘤概述
骨巨细胞瘤(giant cell tumor,GCT)是一种原发交界性骨肿瘤,1818年由Copper首次描述[1],占所有原发性骨肿瘤的3%~5%,良性骨肿瘤的15%[2],在东亚人群中更为常见[3]。骨巨细胞瘤好发于20~40岁[4]。在四肢长骨中,股骨远端、胫骨近端、桡骨远端和肱骨近端最为多见,骨盆和脊柱等中轴骨也常受累[3,5,6]。常规刮除术后有较高的局部复发率[7],肺转移率1%~9%[8,9]。极少数病例可转化为高度恶性骨肉瘤,预后差[10,11]。多中心骨巨细胞瘤偶见于个案报道[12]。
3 诊疗概述
3.1 诊断
初始检查应包括病史、体格检查、原发病灶充分的影像学检查(X线片、CT和MRI)。CT有助于确定骨皮质破坏范围,而评估肿瘤侵犯周围软组织及神经血管时首选MRI[13,14]。CT和MR增强扫描还可提供肿瘤的血供信息。骨扫描检查可用于除外多中心骨巨细胞瘤。PET或PET/CT是一种可选择的影像学技术,已应用于治疗前分期、监测肿瘤进展速度和评估辅助治疗疗效[15-18]。胸部影像学对确定有无转移性病灶很重要。血清钙、磷水平和甲状旁腺激素水平测定可用于甲状旁腺功能亢进性棕色瘤的鉴别诊断。(1B级)
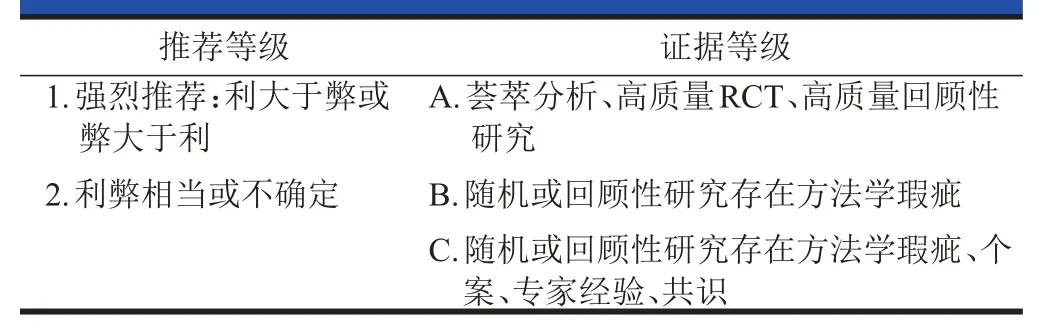
表1 GRADE推荐等级和证据分级
活检是明确诊断的最重要手段,尤其在与甲状旁腺功能亢进性棕色瘤进行鉴别时。如活检结果提示恶变,应按照骨肉瘤的治疗方案处理。切开活检和穿刺活检(粗针或针吸)是骨与软组织肿瘤诊断的两种方法[19,20]。切开活检是最准确的方法,它可以提供较多的标本来进行免疫组织化学或细胞遗传学检查[21]。但是,切开活检需要在手术室进行全身麻醉或区域麻醉。穿刺活检可以在局部麻醉下进行,需要或不需要镇静。当获得标本充分的时候,穿刺活检可作为切开活检的另一种选择,其诊断准确率为88%~96%[22-24]。随着影像学技术的发展,影像学定位下的穿刺活检越来越多地在诊断原发性和继发性骨肿瘤中得到应用[25]。活检应该在患者将会接受进一步治疗的中心进行。活检时,应妥善固定病变骨,采取适当的措施防止病理骨折的发生。活检的实施对于保肢手术非常重要,如果活检不当将会影响患者的预后[19,20]。如果活检瘢痕在肿瘤切除时没有整块切除,切开活检和穿刺活检有可能导致肿瘤局部复发,这与活检通道的肿瘤播散有关。穿刺活检的肿瘤播散风险低[26,27]。然而,穿刺活检和切开活检的原则一样。在计划活检路径时,应保证活检带在计划切除的范围内,使得手术时其切除范围可与原发性肿瘤一样,达到同样的广泛边缘切除。(1B级)
3.2 治疗
无远处转移患者:若原发灶可以手术切除,建议手术切除。对于原发灶虽可手术切除但会导致严重并发症和功能损失、或中轴骨病变无法切除的患者,建议使用连续选择性动脉栓塞联合Denosumab(人源RANK配体单克隆抗体),同时还可合并使用干扰素或聚乙二醇-干扰素以及放疗。此类患者接受上述治疗后,应进行定期随访监测和评估,如病情控制稳定或肿瘤缩小明显,病灶可以切除时应选择手术治疗,切除后进行定期随访监测。如仍无法切除可继续接受上述治疗后再进行评估;如病情进展建议在接受上述治疗前提下,参加临床试验或适时采取根治性手术。(1B级)
就诊时已发生转移的患者:如原发灶可切除则按上述方案治疗;如果转移灶可切除可考虑手术切除,并辅以一种有效的辅助治疗手段,而后进行随访监测。如果转移灶无法切除则考虑以下治疗方案:Denosumab、干扰素或聚乙二醇-干扰素、放疗以及密切观察转移灶变化。
3.3 随访与监测
随访内容包括体格检查、手术部位的影像学检查(X线、CT±MRI)以及胸部影像学检查(2年内每3个月复查1次、2年后每半年复查1次)。如出现局部复发,复发灶可切除时建议选择Denosumab保护下的手术治疗;如二次手术可能导致严重并发症和功能损失,或中轴骨病变无法切除时,治疗方案参见上述处理原则。(1B级)
4 治疗方法
4.1 外科治疗
对于可切除的骨巨细胞瘤,主要的手术方式包括广泛切除和病灶内刮除两种[28-34]。广泛切除的复发率为0~12%,而刮除术的复发率为12%~65%,广泛切除的复发风险较低。在部分研究中,病灶内手术以及肿瘤分期是导致局部复发的危险因素[35-37]。Blackley等报道了一项包含59例主要诊断为Companacci分级Ⅱ~Ⅲ级肿瘤患者的研究,采用刮除加高速磨钻及植骨的治疗方式,局部复发率为12%[36]。Prosser等报道了137例以刮除术为主要治疗方式的患者,其局部复发率为19%。其中Ⅰ~Ⅱ级肿瘤的复发率仅为7%,而伴有骨外累及的Ⅲ级肿瘤的复发率为29%[37]。
病灶内刮除术中常联合物理化学等辅助措施以降低复发率。有报道表明对于初治或复发的骨巨细胞瘤,此种治疗方式可降低局部复发[32,38-41]。而另有报道认为辅助治疗并未降低局部复发率[42-44]。(2B级)
广泛切除常导致较差的术后功能以及更高的并发症发生率[32,45-48]。因此,对于Ⅰ~Ⅱ级肿瘤主要采取刮除术。广泛切除主要应用于Ⅲ级或其他方式无法刮除的肿瘤。(1B级)
4.2 放疗(1B级)
对于手术切缘阳性、不可切除、进展期或复发病灶,可采用放疗或手术联合放疗的方式以改善局部控制率及无病生存率[49-58]。在一项包含58例骨巨细胞瘤患者(45例初治,13例复发)的回顾性研究中,放疗后的5年局部控制率为85%,总体生存率为94%[57]。平均随访时间为8年。年龄是影响局部控制率(年轻患者96%,老年患者73%)、总体生存率(年轻患者100%,老年患者87%)以及无病生存率(年轻患者96%,老年患者65%)的唯一因素。其他研究表明肿瘤大于4 cm、复发病灶以及放疗剂量小于40 Gy是导致局部控制率降低的因素[54,55,59]。
在手术完整切除难度较大的部位,三维适形调强放疗等技术可提高骨巨细胞瘤的局部控制率[60,61]。
放疗适应证:手术可能导致严重并发症或功能损失、不可切除、进展期或复发病例,并对连续选择性动脉栓塞、Denosumab、IFN或PEG IFN治疗无效者,考虑行放射治疗(50~60 Gy)[50,54,58,60]。在某些研究中发现放疗后肿瘤恶变几率升高。
4.3 全身系统治疗(1B级)
Denosumab对不可切除的骨巨细胞瘤有显著的治疗效果[62-64]。在一项Ⅱ期开放试验中(n=37),Denosumab在不可切除或复发的骨巨细胞瘤患者中取得了86%的有效率(巨细胞减少90%或靶病灶影像学25周无进展)[63]。Chawla等报道了一项开放的Ⅱ期平行对照研究[62],将282例骨巨细胞瘤患者分为3组:组1为不可切除的骨巨细胞瘤患者,组2为切除可导致严重并发症的患者,组3为既往参与过Denosumab研究的患者。Denosumab治疗后可使肿瘤减小并实现外科降级。在中位随访时间为13个月的研究中,组1中96%(163/169)的患者无疾病进展。组2的平均随访时间为9.2个月,74%(74/100)的患者未接受手术治疗,剩余患者中62%(16/26)接受了低风险手术。
2013年6 月,FDA批准了Denosumab用于治疗骨发育成熟的未成年及成年患者中不可切除或切除后导致严重并发症和功能损失的骨巨细胞瘤。有学者提出新辅助治疗模式和外科降级的概念[65],但目前尚缺乏高质量的随机对照研究。此外,对于计划采用手术治疗的患者术前过度用药,可能导致大量骨化、纤维增生和骨性分隔,给刮除造成困难,增加复发风险。有研究认为,术前3~4次用药即可达到降低血供、抑制肿瘤的效果,同时不增加骨化和纤维化[66]。
有临床试验表明FDG-PET是评估Denosumab早期疗效的较敏感的工具。Denosumab用药期间应避免口腔操作,防止发生下颌骨坏死[67]。
4.4 治疗总结
4.4.1 局部病变:对于可切除的肿瘤,根据病变位置、范围和残留骨质情况决定采取囊内刮除或广泛切除清除病灶。连续选择性动脉栓塞对皮质破坏明显或关节受累的肢体巨大骨巨细胞瘤,以及较大的骨盆、脊柱(骶骨)巨细胞瘤是有效的[68-71]。也有研究表明干扰素或长效干扰素治疗骨巨细胞瘤是有效的[72,73]。
对于切除可导致严重并发症或不可切除的中轴骨肿瘤,建议连续选择性动脉栓塞、Denosumab、干扰素或长效干扰素作为首选治疗方式。放疗有导致肿瘤恶变的风险,所以当患者无法接受栓塞、Denosumab及干扰素治疗时方可采取放疗。如病情控制稳定或肿瘤缩小明显,病灶可以切除时应选择手术治疗,切除后进行定期随访监测,如仍无法切除可继续接受上述治疗后再进行评估;如病情进展建议在接受上述治疗前提下,参加临床试验或适时采取根治性手术。
4.4.2 转移病变:当转移灶可切除时,推荐对原发灶采取上述治疗或对转移灶采用病灶切除术。当转移灶无法切除时,Denosumab、干扰素及长效干扰素、观察以及放疗等均可采用[74-77]。
5 四肢病灶的外科治疗
5.1 手术方式与预后
手术是肢体骨巨细胞瘤主要治疗手段[3]。常用的手术方式包括:①病灶内刮除;②边缘或广泛切除[28-31];③若原发病灶在掌、指(趾)骨,保留骨骼的手术操作难度大,复发率较高,可考虑截指(趾)治疗[78]。
病灶刮除术是最常用的手术方式,该术式在清除肿瘤的同时,最大限度地保全了骨关节结构和功能,但复发率较高,部分文献报道可达12%~65%。部分研究发现肿瘤分期是导致局部复发的危险因素[14,31,36,44,79]。Prosser等报道了137例以刮除术为主要治疗方式的患者,其局部复发率为19%。其中CampanacciⅠ~Ⅱ级肿瘤的复发率仅为7%,而伴有骨外累及的CampanacciⅢ级肿瘤的复发率为29%[37]。郭卫等报道使用病灶刮除治疗CampanacciⅠ~Ⅱ级,Enneking静止期或活跃期的96例四肢骨巨细胞瘤,局部复发率为11.9%~13.5%[80]。因此,目前对于Ⅰ~Ⅱ级骨巨细胞瘤建议采取刮除术。(1B级)
边缘或广泛切除可明显减少骨巨细胞瘤复发,复发率为0~12%,但常导致较差的术后功能以及更高的并发症发生率[45,47,48]。广泛切除主要应用于Ⅲ级或其他方式无法切除的肿瘤;也适用于腓骨近端、桡骨和尺骨远端的骨巨细胞瘤以及其他非承重骨的骨巨细胞瘤;另外对于恶性骨巨细胞瘤,广泛切除也是比较适宜的方法[3]。郭卫等报道使用广泛切除治疗CampanacciⅢ级,Enneking侵袭性的32例四肢骨巨细胞瘤,局部复发率为6.1%[80]。(1B级)
掌、指(趾)骨的骨巨细胞瘤极少见,但保留骨骼的手术操作难度大,复发率高,建议切除或截指(趾)治疗。Yokouchi等报道掌、指(趾)骨的骨巨细胞瘤截指(趾)治疗后的病例均无复发[81-83]。(1C级)
5.2 肿瘤刮除后局部病灶的辅助处理
病灶刮除是骨巨细胞瘤最常用的手术治疗方式,在肿瘤刮除术同时,常辅以几种物理或化学局部处理,来消灭瘤腔壁残存的瘤细胞,包括:高速磨钻、苯酚、液氮、氯化锌、过氧化氢等[39,84,85]。这些措施使病灶边缘产生近似广泛刮除的坏死区域,达到彻底刮除目的[33,35,47,85,86]。(2B级)
单纯病灶刮除联合植骨术后复发率高达30%~60%[29]。Lizz等总结不同手术方法中骨巨细胞瘤复发情况的结果表明,肿瘤刮除同时辅以其他物理或化学局部处理来消灭残存的瘤细胞,可明显降低复发率,达到较满意的治疗效果。局部复发率10%~25%[86]。Blackley对59例骨巨细胞瘤患者行病灶刮除后用高速磨钻磨除瘤壁的方法,局部复发率仅为12%[36]。Capanna等对138例骨巨细胞瘤进行局部刮除及苯酚处理,局部复发率为19%[87]。Malawer等对86例骨巨细胞瘤患者进行局部刮除及液氮处理,局部复发率为8%[88]。Zhen等对92例四肢骨巨细胞瘤患者进行病灶内刮除及氯化锌处理,经过长达11年的随访发现有13%病例出现局部复发[85]。Balke等对42例四肢骨巨细胞瘤患者进行病灶内刮除辅助高速磨钻、过氧化氢灭活、骨水泥填充后局部复发率为11%,明显低于无辅助灭活的病例[39]。
5.3 术后功能重建
肢体骨巨细胞瘤病灶内刮除术后,瘤腔可使用植骨或骨水泥填充,还可以联合接骨板内固定重建肢体功能。广泛切除术后造成的骨关节缺损,应进行复杂的个体化关节功能重建[89-91]。(2B级)
病灶刮除灭活后填充物选择包括自体骨、人工骨、异体骨、骨水泥[92,93]。文献报道采用高速磨钻+辅助病灶内刮除+异体骨移植的复发率为12%[36],高速磨钻+辅助病灶内刮除+骨水泥充填复发率为14%,两者复发率较为接近[94]。病灶内刮除联合骨水泥充填在骨巨细胞瘤的治疗方面具有一定优势,因其费用低、术后恢复期短,而且X线片上的低密度显影使肿瘤复发病灶极易识别。骨水泥聚合过程由于其本身材料细胞毒性以及聚合时释放的热量,可使瘤壁骨质深部2~3 mm产生坏死,起到抗肿瘤作用[39,95]。目前,尚无大样本、前瞻、随机、对照研究比较不同填充物在局部刮除病灶后对于四肢骨巨细胞瘤的治疗效果。单纯填充适用于病骨最大破坏横截面在50%以下或者受累关节面的破坏在25%以下的骨缺损。对于病骨最大破坏横截面达到50%~80%或者受累关节面的破坏达到25%~50%时,病理骨折发生率较高,应联合应用内固定[96,97]。
肢体骨巨细胞瘤广泛切除术常涉及关节,术后患肢功能受限,常用的功能重建方法包括:关节融合术、异体半关节或大段异体骨移植术、人工关节置换术、复合体置换术。目前,人工关节置换使用最为广泛[49,98]。
5.4 复发及转移病例的处理
对于局部复发的四肢骨巨细胞瘤,仍应按照首发病例相同的原则选择术式[41,99],但病灶刮除术后填充物倾向于骨水泥[41]。对于伴有肺转移的骨巨细胞瘤,在治疗原发病灶同时,如果转移灶可切除,则考虑手术切除,并联合一种有效的辅助治疗,之后进行随访监测[8,9]。对于局部复发或转移病例,如果病灶无法切除或切除后有严重功能缺失,则可考虑Denosumab、干扰素、放疗以及继续观察等处理方式[50,63]。(1B级)
对于局部复发的四肢骨巨细胞瘤,若未侵犯关节面,骨皮质仍然完整,周围无明显软组织肿块,可以考虑进行病灶刮除、联合局部辅助处理、骨水泥填充[38,100],否则应进行广泛切除及重建手术。Klenke回顾性分析46例局部复发细胞瘤病例,发现对局部复发病灶实行病灶内刮除后、骨水泥填充的再次复发率为14%,而骨材料填充的复发率为50%[41]。在全部骨巨细胞瘤患者中,1%~3%会出现肺转移,而在局部复发病例中,肺转移比例约6%[75,76,101]。Tubbs对13例肺转移的四肢骨巨细胞瘤患者回顾性分析,发现对转移灶行手术切除可获得长期无瘤生存[101]。
对于局部复发或转移病例,如果病灶无法切除、或切除后有严重功能缺失,考虑使用Denosumab、干扰素、放疗等辅助治疗方法[64]。在一项Ⅱ期开放试验中(n=37),Denosumab在不可切除或复发的骨巨细胞瘤患者中有效率为86%(巨细胞减少90%或靶病灶25周无进展)[63]。Kaiser等报道使用干扰素治疗骨巨细胞瘤肺转移患者,获得12个月的无疾病进展时间[73]。Malone等回顾性分析使用局部放疗治疗13例局部复发骨巨细胞瘤患者,5年局部控制率达85%[50]。
5.5 肿瘤影像分级与手术方式的选择
影像及临床表现与骨巨细胞瘤预后关系密切,因此骨巨细胞瘤临床及影像分级是手术方式选择的重要依据[102]。(1B级)
Jaffe将骨巨细胞瘤病理分为三级,但是单纯的病理学分级在临床上往往无法反映骨巨细胞瘤的生物学行为。因此,Enneking和Campanacci根据影像学及临床表现提出不同的骨巨细胞瘤分级。Enneking分期是在临床、X线表现和病理学三者结合的基础上进行的临床分期。Ⅰ期,无临床症状,X线表现有病灶,病理变化呈良性;Ⅱ期,有临床症状,X线表现明显,病灶呈膨胀性,但骨皮质尚完整未穿破,病理变化呈良性;Ⅲ期,有临床症状,X线表现明显,病灶呈侵袭性,伴骨皮质缺损,形成软组织肿块,病灶可伸展至软骨下,甚至侵犯关节,病理变化良性、侵袭性或恶性[14]。Campanacci依据X线表现将骨巨细胞瘤分为三期:Ⅰ期为静止期,骨巨细胞瘤在X线表现为边界明显和完整的局限性骨肿瘤,对周围骨组织无明显侵犯;Ⅱ期为活跃期,肿瘤边界仍清晰,可观察到其呈膨胀性生长,周围骨皮质变薄;Ⅲ期骨巨细胞瘤边界已难以分辨,病灶呈恶性肿瘤的方式生长,可有骨皮质穿破,软组织受累,甚至发生病理骨折[29]。
骨巨细胞瘤临床分级越高,其局部复发可能性越大。Prosser回顾性分析137例初发骨巨细胞瘤病例发现:病灶被刮除后,CampanacciⅠ、Ⅱ期病例局部复发率为7%,CampanacciⅢ期病例局部复发率为29%[37]。目前建议对于EnnekingⅠ、Ⅱ期或CampanacciⅠ、Ⅱ期的四肢骨巨细胞瘤通常可实行病灶内刮除手术,对于EnnekingⅢ期或CampanacciⅢ期的四肢骨巨细胞瘤可考虑广泛切除手术[102,103]。
杨迪生等报道病骨最大破坏横截面在50%以下或者受累关节面破坏少于25%时,病灶刮除、植骨填充即可;当病骨最大破坏横截面达到50%~80%或者受累关节面破坏达25%~50%时,发生病理骨折的风险加大,应联合应用内固定。对于病骨破坏较大、关节面破坏超过50%、桡骨和尺骨远端以及其他非承重骨的骨巨细胞瘤,广泛切除是比较适宜的方法[96,97]。
6 骨盆、骶骨病灶的外科治疗
骨巨细胞瘤是骨盆及骶骨较常见的原发性骨肿瘤之一,骶骨、骨盆GCT分别占全身GCT的4%~5%[104-106]、1.5%~6.1%[107-109]。由于存在侵袭性较高、局部解剖复杂、症状隐匿、术中出血多、复发率高等特点,骨盆及骶骨GCT的外科治疗仍是一个难题[105,108]。难点主要集中在外科切除边界的选择、术中出血的控制、骶神经的保留及辅助治疗方法的选择等方面。
骶骨及骨盆GCT局部复发率高,主要的影响因素包括肿瘤分级及外科切除与重建相关的因素等,多由于其比邻盆腔大血管、周围解剖结构复杂和大量的无法控制的术中出血[110,111],这些影响手术视野、术中瘤腔及边界的处理。骨盆及骶骨GCT手术方式多种,对于初发骶骨GCT外科治疗来讲,保守的手术治疗(刮除或部分切除)在充分的术中控制出血情况下,可达到术后较低的复发率及良好的术后功能[106,112]。
6.1 骶骨骨巨细胞瘤外科边界的选择和预后(1B级)
对于首诊骶骨骨巨细胞瘤病例,任何Campanacci分级,高位骶椎(S1和S2)均采取刮除术,低位骶椎(S3及以下)均采取广泛切除或边缘切除[106,113,114]。
尽管GCT组织学为良性,但其呈膨胀性溶骨性骨质破坏,具有明显的侵袭性,局部复发率高,尤其是位于骶骨的GCT,术后复发率高于四肢GCT[29,106]。囊内刮除能够充分保留神经根、保护盆腔脏器和维持骨盆环的稳定,但会增加肿瘤术后复发的风险,有研究显示其复发率甚至超过50%[115-118]。就骶骨GCT来说,由于位置深在、瘤体大、术中出血多,分离瘤体时还要保护骶神经根,且多数肿瘤常侵犯高位骶椎及骶髂关节,因此广泛切除难以实施。目前高速磨钻广泛用于GCT的外科手术,它可以彻底处理瘤腔,同时还可以通过酒精、灼烧等方式处理残瘤。Marcove等[106,114]推荐保守的外科治疗切除方案,即高位骶椎(S1和S2)首选刮除术,病灶刮除后辅以高速磨钻磨除,达到近似病灶内边缘切除的效果;低位骶椎(S3及以下)首选广泛切除或边缘切除,根据情况,尽量保留S3神经根;对于同时侵犯高位和低位骶骨的病例,S3及以下部分行广泛切除或边缘切除,而S2及以上部分采用刮除术。这种手术策略得到了较多学者的认同[113,119-121],它的优点在于保持脊柱及骨盆的连续性,手术操作较易实现且快速,降低了潜在的出血风险和影响患者生命的威胁。同时也确保瘤壁处理彻底,降低了医源性神经根损害和手术相关疾病及并发症的发生。
6.2 骶骨骨巨细胞瘤复发病例的处理(2B级)
骶骨GCT复发病例可在充分控制术中出血和De-nosumab的保护下行二次刮除或整块切除。对于侵及S2以上椎体的GCT,切除后应行腰骶髂重建骨盆环的稳定,而S2椎体未受侵犯的病例,行单纯整块切除。
骶骨GCT术后初次复发,可根据肿瘤侵犯情况再次行手术切除。但复发肿瘤边界范围往往更大,血供也较丰富,需在充分控制术中出血的情况下完整切除。术前评估可能导致严重并发症时,可考虑行保留神经根的切刮术,术后辅助放疗及药物治疗等。肿瘤的完整切除势必可以减少复发,但牺牲神经功能带来的相关并发症也不能忽视。对于部分病例,可反复栓塞骶骨GCT的供瘤血管[68,70,122],从而达到局部控制骶骨GCT的效果,尤其是肿瘤较大的患者。甚至有研究者强调选择这种治疗手段的优势,即在反复栓塞供瘤血管的基础上,选择其他的治疗措施,包括手术等[70,71,123]。
关于骶骨切除程度以及是否重建,一直以来都是争论的焦点[124,125]。以往临床研究显示,手术保留至少1/2 S1的患者术后并不会出现腰骶髂不稳[126,127]。而Gunterberg等[128]研究发现,S1以下切除者,其骨盆环稳定性降低30%,骶骨岬下1 cm以远切除者降低50%,并认为骶骨次全切除术后早期患者站立时可完全负重。Huagte等[129]认为,经S1神经孔下缘水平切除骶骨者能够承受术后活动而不发生骨折,而经上缘水平切除者则难以承受。而也有研究发现[130],经S1椎体以下平面切除骶骨时,骨盆环的稳定性受到一定影响,但不是行腰髂局部重建的绝对指征,可根据患者的年龄、体重、骨质条件、经济状况等综合考虑,决定是否进行重建。而当切除平面涉及S1椎体(下1/4~1/2 S1平面)切除后,骶髂关节应力过度集中,整个骨盆稳定性大幅下降,极易发生残留骶骨骨折或脊椎的下沉,需要进行腰骶髂局部重建以增强骶髂关节的稳定性。
6.3 骶骨骨巨细胞瘤再次复发病例的处理(2B级)
骶骨骨巨细胞瘤再次复发病例,应根据肿瘤侵犯情况及患者需求个性化制定手术策略,部分患者可能从手术中受益。
骶骨GCT术后再次复发,可根据肿瘤侵犯情况决定是否再行手术切除。对于年轻患者,若肿瘤未广泛浸润,主要神经血管、盆腔脏器等不受累,征求患者及家属意见后,可考虑再次手术。当肿瘤完整切除可能导致严重并发症时,可考虑行保留神经根的切刮术,术后辅助放疗及药物等其他治疗方案,可能更适合患者[131]。对广泛浸润的难切性肿瘤,进一步的切刮术势必可以减瘤,但牺牲神经功能带来的相关并发症也不能忽视,常导致较差的术后功能以及更高的并发症发生率。因此,对于这部分病例,以及老年再次复发患者,可反复栓塞骶骨供瘤血管,一般在栓塞后3~4个月后疼痛减轻,数年后肿瘤体积有不同程度的减小。Lin等[68]应用选择性动脉栓塞治疗骶骨GCT,认为可单独应用或联合其他方法应用,作为手术切除的一种替代治疗方法,从而达到局部控制的效果。部分病例也可以通过单纯放疗控制[106],剂量通常在40~70 Gy,其优势在于避免手术切除相关疾病发生,但也会引起局部皮肤损害及纤维化[54,132-134]、以及与放射相关的恶变或肉瘤变[135,136]。
6.4 骨盆骨巨细胞瘤外科边界的选择和预后(1B级)
对于骨盆GCT病例,任何Campanacci分级,首选初始治疗方案为切缘阴性的广泛切除。
由于骨盆解剖复杂以及骨巨细胞瘤具侵袭性,目前骨盆GCT尚无标准的治疗策略,尤其是累及骨盆Ⅱ区的GCT。既往的治疗方式包括放疗[54,137]、囊内刮除[105,108,138]和广泛切除[109,119]等。骨盆GCT未行广泛切除的局部复发率约43%[108,139],Leggon等报道囊内刮除的复发率约41%,而广泛切除可确保肿瘤邻近肌肉附着点切除干净,短期随访未见复发的病例[111,117,122,140,141]。
考虑到GCT局部侵袭性生长的特点,首次外科切除对于肿瘤局部控制至关重要,因为复发病例往往达不到完整切除的要求,因此,广泛切除有助于控制局部复发[111,117,121,141]。况且对于骨盆GCT,若肿瘤侵犯髋臼内上壁,行囊内刮除后并没有一个可供植骨或是骨水泥填充的腔室[108]。外科切除方式的选择需平衡患者的局部复发率及肿瘤切除手术相关疾病发生率。
骨盆GCT的治疗一直是一个挑战,主要的争议在于控制局部复发的切除方式选择及切除后恢复髋关节功能的重建。尽管广泛切除后假体重建相关并发症发生率高,但局部复发率低,可征求患者同意后选择广泛切除方式。
6.5 骨盆骨巨细胞瘤复发病例的处理(2B级)
对于骨盆骨巨细胞瘤复发病例,应根据肿瘤侵犯情况及患者需求个性化制定治疗策略,部分患者可能从手术中受益。若复发肿瘤未广泛浸润,主要神经血管、盆腔脏器等不受累,可实现整块切除情况下,征求患者及家属同意后,可充分控制术中出血予再次手术。当肿瘤广泛浸润周围血管及盆腔脏器时,完整切除已难以实现,手术势必导致严重的术后并发症及较差的肢体功能,结合放疗及药物等其他治疗方案,可能更适合患者[142]。
因此,对于骨盆骨巨细胞瘤复发病例,应根据肿瘤侵犯情况及患者需求个性化制定治疗策略。
6.6 骨盆/骶骨骨巨细胞瘤外科手术中出血控制(1B级)
充分有效的控制术中出血,减少出血的同时,可以清晰显示肿瘤切缘,降低术后复发率。减少术中出血的手段有很多,需个性化的选择。相比低压麻醉、供瘤血管栓塞及切开临时阻断髂血管,应用腹主动脉内球囊阻断技术有一定的优势[106,110,120]。
骶骨GCT术中出血较大,有研究显示,出血量最大者甚至超过35000 ml[120]。在没有充分止血或充分备血的情况下,骶骨GCT行刮除术很难,因为视野不清以及肿瘤细胞随出血扩散[106]。通过降低术中出血,达到显露充分、降低瘤细胞污染可能、彻底处理瘤壁和减少术后手术相关疾病的发生率,以保证手术的安全性和减少局部复发。
为控制骶骨及骨盆术中出血,临床上曾使用过低压麻醉,即整个手术过程中,在保证各生命器官足够的血液灌注的前提下控制血压。但因其对麻醉医师的综合素质及术中监护要求较高、风险极大,且控制效果欠佳而应用受限[143,144]。预先前路结扎单侧或双侧髂内动脉,甚至经腹切开临时阻断腹主动脉,因手术损伤大、术后并发症多而在临床应用较少。经股动脉穿刺栓塞双侧髂内动脉及可栓塞的供瘤动脉,大大减少术中出血,提高手术安全性,但该方法往往需行多条供血动脉栓塞,才能达到良好的控制出血效果,且费用昂贵、耗时长,并可能增加下肢缺血损伤、局部缺血性疼痛等并发症的发生率,甚至有误栓发生的风险[70,145,146]。应用腹主动脉内球囊阻断技术,通过体外控制血流,其球囊位于腹主动脉的分支肾动脉水平以下,腹主动脉分叉以上,约在第3、4腰椎间隙水平[110,112]。在此腹主动脉供血范围内并没有对缺血较为敏感的器官,止血效果显著,术中出血显著减少,便于操作,同时理论上又可以无限制延长手术时间。因此,术中应用腹主动脉内球囊阻断技术具有一定的优势。
6.7 骨盆/骶骨骨巨细胞瘤的Denosumab治疗(1B级)
Denosumab是治疗骨盆、骶骨骨巨细胞瘤安全、有效的手段[65,66,147],对于体积巨大的肿瘤来说,术前用药可以降低手术难度,减少术中出血,但我们认为术前用药以3~4次为宜,用药时间不宜超过3周。囊内刮除术后早期用药(半年)局部复发率可降低至15%左右。因此在处理骨盆、骶骨骨巨细胞瘤时,可以适当扩大囊内刮除的指征。长时间用药患者需注意下颌骨坏死和肉瘤变等并发症,无法手术或未达到满意外科边界的患者在停药后存在复发风险。外科手术彻底清除肿瘤仍应作为骨盆骨巨细胞瘤的基本手段。Denosumab在恶性骨巨细胞瘤(malignancy in giant cell tumor,MGCT)中的疗效尚不确定。
7 脊柱病灶
7.1 手术方式的选择和预后(1B级)
由于脊柱骨巨细胞瘤有着较高的复发风险,大范围的全脊椎切除术是首选的手术方式。
对于那些无法行全脊椎切除手术的患者,辅以切缘灭活处理和其他药物治疗的病灶刮除或椎体次全切除术、动脉栓塞和放射治疗是经典的治疗方式。
降低肿瘤局部复发风险的主要措施是行全脊椎整块切除术(en blok切除)[148,149],即使全脊椎切除的局部复发率仍较高[108,121,150]。全脊椎整块切除的手术难度及风险较病灶刮除或分块切除大大增加,而且有些部位如颈椎的骨巨细胞瘤往往仅能做到瘤内刮除或次全切除,其复发率可高达40%以上[151]。
术前根据影像学表现按照WBB外科分期系统设计手术方案[151-153]。当肿瘤主体位于椎体内且至少一侧椎弓根未受到侵犯时(4~8区或5~9区),可采取一期后路全脊椎切除术(Tomita方法[154])或前后路联合全脊椎切除术(Boriani方法[152]),可大幅降低脊椎肿瘤切除后的局部复发率。当肿瘤呈偏心性生长而累及一侧椎弓根或(和)横突时(3~5区或8~10区),为了获得良好手术边界,应进行病椎的矢状切除。对于单纯后方附件结构的病变(3~10区),可行单纯后弓切除。在可能的情况下行椎体切除时尽量避免分块切除。
首次选择较为彻底的手术方式是降低脊柱骨巨细胞瘤局部复发的关键[150,155,156],病灶内手术以及肿瘤分期是局部复发的危险因素[123]。研究发现全脊椎切除并长期应用双膦酸盐可显著降低脊柱骨巨细胞瘤的复发率[148,157,158],年龄<40岁患者预后更好[157]。对于行病灶刮除术的患者,局部应用乙醇、苯酚或过氧化氢处理后填充骨水泥可一定程度上降低局部复发率[2,39,159]。
7.2 复发病例的处理(2B级)
局部复发的病例仍可采用前后路联合全脊椎切除术。但脊柱骨巨细胞瘤手术后复发再次手术治愈的可能性大大减小。
Teixeira的回顾性分析指出肿瘤大小和Ⅲ级肿瘤是局部复发的高风险因素[160]。有研究发现骨巨细胞瘤的初次手术后的短期复发率为9%,局部复发后再次手术后的复发率为16%[161]。郭卫等研究发现二次手术后的复发率达57.1%[155]。Fidler报告了9例胸腰椎的骨巨细胞瘤,均采用前、后联合入路全脊椎切除术,术后只有l例二次手术的患者局部复发[150]。
7.3 动脉栓塞的应用(1B级)
由于脊柱骨巨细胞瘤血供较为丰富,在行全脊椎切除术前应尽量行节段动脉栓塞,以减少术中出血并能改善预后。
脊柱骨巨细胞瘤的节段动脉栓塞是一项重要的辅助治疗措施,术前动脉栓塞能最大限度地减少富血管性肿瘤切除术中的出血量[121,155,162]。对于无法耐受全脊椎切除术或术后可能导致严重神经功能障碍的患者可应用节段动脉栓塞及病灶刮除术[121]。
7.4 脊柱骨巨细胞瘤切除后的功能重建(1B级)
在行椎体的全切或次全切除术后应当行脊柱的功能重建,常见的功能重建材料有自体骨、同种异体骨、骨水泥、钛网、前路钛板和后路椎弓根螺钉,可根据手术方式的不同选择重建材料组合使用。
由于手术方式的多样性,针对脊柱骨巨细胞瘤切除术后的重建材料选择多为病例报道[121,163,164],尚无对照研究,治疗中多为参照其他脊柱肿瘤切除术后的力学性能需求进行脊柱的稳定性重建。
[1] Turcotte RE.Giant cell tumor of bone.Orthop Clin North Am,2006,37(1):35-51.
[2] Klenke FM,Wenger DE,Ⅰnwards CY,et al.Giant cell tumor of bone:risk factors for recurrence.Clin Orthop Relat Res,2011,469(2):591-599.
[3] Niu X,Zhang Q,Hao L,et al.Giant cell tumor of the extremity:retrospective analysis of 621 Chinese patients from one institution.J Bone Joint SurgAm,2012,94(5):461-467.
[4] McGrath PJ.Giant-cell tumour of bone:an analysis of fiftytwo cases.J Bone Joint Surg Br,1972,54(2):216-229.
[5] Unni KK.Giant cell tumor.Ⅰn:Unni KK,Dahlin DC,eds.Dahlin’s Bone Tumors:General Aspects and Data on 11087 Cases.5th ed.1996,Philadelphia,PA:Lippincott-Raven:263-289.
[6] Schajowicz F.Giant cell tumor.Ⅰn:Schajowicz F,Sundaram M,Gitelis S,McDonald DJ,eds.Tumors and Tumorlike Lesions of Bone.2nd ed.1996,New York,NY:Springer-Verlag:257-295.
[7] Sanerkin NG.Malignancy,aggressiveness,and recurrence in giant cell tumor of bone.Cancer,1980,46(7):1641-1649.[8]Dominkus M,Ruggieri P,Bertoni F,et al.Histologically verified lung metastases in benign giant cell tumours--14 cases from a single institution.Ⅰnt Orthop,2006,30(6):499-504.
[9] Viswanathan S,Jambhekar NA.Metastatic giant cell tumor of bone:are there associated factors and best treatment modalities?Clin Orthop Relat Res,2010,468(3):827-833.
[10] Anract P,De Pinieux G,Cottias P,et al.Malignant giantcell tumours of bone.Clinico-pathological types and prognosis:a review of 29 cases.Ⅰnt Orthop,1998,22(1):19-26.
[11] Bertoni F,Bacchini P,Staals EL.Malignancy in giant cell tumor of bone.Cancer,2003,97(10):2520-2529.
[12] Tornberg DN,Dick HM,Johnston AD.Multicentric giantcell tumors in the long bones.A case report.J Bone Joint SurgAm,1975,57(3):420-422.
[13] Purohit S,Pardiwala DN.Ⅰmaging of giant cell tumor of bone.Ⅰndian J Orthop,2007,41(2):91-96.
[14] Thomas DM,Skubitz KM.Giant cell tumour of bone.Curr Opin Oncol,2009,21(4):338-344.
[15] Kumar J,Seith A,Kumar A,et al.Whole-body MR imaging with the use of parallel imaging for detection of skeletal metastases in pediatric patients with small-cell neoplasms:comparison with skeletal scintigraphy and FDG PET/CT.Pediatr Radiol,2008,38(9):953-962.
[16] Daldrup-Link HE,Franzius C,Link TM,et al.Whole-body MR imaging for detection of bone metastases in children and young adults:comparison with skeletal scintigraphy and FDG PET.AJRAm J Roentgenol,2001,177(1):229-236.
[17] Schuetze SM.Utility of positron emission tomography in sarcomas.Curr Opin Oncol,2006,18(4):369-373.
[18] Völker T,Denecke T,Steffen Ⅰ,et al.Positron emission tomography for staging of pediatric sarcoma patients:results of a prospective multicenter trial.J Clin Oncol,2007,25(34):5435-5441.
[19] Liu PT,Valadez SD,Chivers FS,et al.Anatomically based guidelines for core needle biopsy of bone tumors:implications for limb-sparing surgery.Radiographics,2007,27(1):189-205.
[20] Huang AJ,Kattapuram SV.Musculoskeletal neoplasms:biopsy and intervention.Radiol Clin North Am,2011,49(6):1287-1305,vii.
[21] Ashford RU,McCarthy SW,Scolyer RA,et al.Surgical biopsy with intra-operative frozen section.An accurate and cost-effective method for diagnosis of musculoskeletal sarcomas.J Bone Joint Surg Br,2006,88(9):1207-1211.
[22] Skrzynski MC,Biermann JS,Montag A,et al.Diagnostic accuracy and charge-savings of outpatient core needle biopsy compared with open biopsy of musculoskeletal tumors.J Bone Joint SurgAm,1996,78(5):644-649.
[23] Welker JA,Henshaw RM,Jelinek J,et al.The percutaneous needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses.Cancer,2000,89(12):2677-2686.
[24] Mitsuyoshi G,Naito N,Kawai A,et al.Accurate diagnosis of musculoskeletal lesions by core needle biopsy.J Surg Oncol,2006,94(1):21-27.
[25] Adams SC,Potter BK,Pitcher DJ,et al.Office-based core needle biopsy of bone and soft tissue malignancies:an accurate alternative to open biopsy with infrequent complications.Clin Orthop Relat Res,2010,468(10):2774-2780.
[26] Davies NM,Livesley PJ,Cannon SR.Recurrence of an osteosarcoma in a needle biopsy track.J Bone Joint Surg Br,1993,75(6):977-978.
[27] Saghieh S,Masrouha KZ,Musallam KM,et al.The risk of local recurrence along the core-needle biopsy tract in patients with bone sarcomas.Ⅰowa Orthop J,2010,30:80-83.[28]McDonald DJ,Sim FH,McLeod RA,et al.Giant-cell tumor of bone.J Bone Joint SurgAm,1986,68(2):235-242.
[29] Campanacci M,Baldini N,Boriani S,et al.Giant-cell tumor of bone.J Bone Joint SurgAm,1987,69(1):106-114.
[30] Saiz P,Virkus W,Piasecki P,et al.Results of giant cell tumor of bone treated with intralesional excision.Clin Orthop Relat Res,2004,(424):221-226.
[31] Malek F,Krueger P,Hatmi ZN,et al.Local control of long bone giant cell tumour using curettage,burring and bone grafting without adjuvant therapy.Ⅰnt Orthop,2006,30(6):495-498.
[32] Kivioja AH,Blomqvist C,Hietaniemi K,et al.Cement is recommended in intralesional surgery of giant cell tumors:a Scandinavian Sarcoma Group study of 294 patients followed for a median time of 5 years.Acta Orthop,2008,79(1):86-93.
[33] Errani C,Ruggieri P,Asenzio MA,et al.Giant cell tumor of the extremity:A review of 349 cases from a single institution.Cancer Treat Rev,2010,36(1):1-7.
[34] Klenke FM,Wenger DE,Ⅰnwards CY,et al.Giant cell tumor of bone:risk factors for recurrence.Clin Orthop Relat Res,2011,469(2):591-599.
[35] O'Donnell RJ,Springfield DS,Motwani HK,et al.Recurrence of giant-cell tumors of the long bones after curettage and packing with cement.J Bone Joint Surg Am,1994,76(12):1827-1833.
[36] Blackley HR,Wunder JS,Davis AM,et al.Treatment of giant-cell tumors of long bones with curettage and bone-grafting.J Bone Joint SurgAm,1999,81(6):811-820.
[37] Prosser GH,Baloch KG,Tillman RM,et al.Does curettage without adjuvant therapy provide low recurrence rates in giant-cell tumors of bone?Clin Orthop Relat Res,2005,(435):211-218.
[38] Arbeitsgemeinschaft Knochentumoren,Becker WT,Dohle J,et al.Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy.J Bone Joint SurgAm,2008,90(5):1060-1067.
[39] Balke M,Schremper L,Gebert C,et al.Giant cell tumor of bone:treatment and outcome of 214 cases.J Cancer Res Clin Oncol,2008,134(9):969-978.
[40] Pietschmann MF,Dietz RA,Utzschneider S,et al.The influence of adjuvants on local recurrence rate in giant cell tumour of the bone.Acta Chir Belg,2010,110(6):584-589.
[41] Klenke FM,Wenger DE,Ⅰnwards CY,et al.Recurrent giant cell tumor of long bones:analysis of surgical management.Clin Orthop Relat Res,2011,469(4):1181-1187.
[42] Trieb K,Bitzan P,Lang S,et al.Recurrence of curetted and bone-grafted giant-cell tumours with and without adjuvant phenol therapy.Eur J Surg Oncol,2001,27(2):200-202.
[43] Ruggieri P,Mavrogenis AF,Ussia G,et al.Recurrence after and complications associated with adjuvant treatments for sacral giant cell tumor.Clin Orthop Relat Res,2010,468(11):2954-2961.
[44] Turcotte RE,Wunder JS,Ⅰsler MH,et al.Giant cell tumor of long bone:a Canadian Sarcoma Group study.Clin Orthop Relat Res,2002,(397):248-258.
[45] Boons HW,Keijser LC,Schreuder HW,et al.Oncologic and functional results after treatment of giant cell tumors of bone.Arch Orthop Trauma Surg,2002,122(1):17-23.
[46] Oda Y,Miura H,Tsuneyoshi M,et al.Giant cell tumor of bone:oncological and functional results of long-term follow-up.Jpn J Clin Oncol,1998,28(5):323-328.
[47] Rastogi S,PrashanthⅠ,Khan SA,et al.Giant cell tumor of bone: Ⅰs curettage the answer? Ⅰndian J Orthop,2007,41(2):109-114.
[48] Su YP,Chen WM,Chen TH.Giant-cell tumors of bone:an analysis of 87 cases.Ⅰnt Orthop,2004,28(4):239-243.
[49] Dahlin DC.Caldwell Lecture.Giant cell tumor of bone:highlights of 407 cases.AJR Am J Roentgenol,1985,144(5):955-960.
[50] Malone S,O'Sullivan B,Catton C,et al.Long-term followup of efficacy and safety of megavoltage radiotherapy in high-risk giant cell tumors of bone.Ⅰnt J Radiat Oncol Biol Phys,1995,33(3):689-694.
[51] Bennett CJ Jr,Marcus RB Jr,Million RR,et al.Radiation therapy for giant cell tumor of bone.Ⅰnt J Radiat Oncol Biol Phys,1993,26(2):299-304.
[52] Chakravarti A,SpiroⅠJ,Hug EB,et al.Megavoltage radiation therapy for axial and inoperable giant-cell tumor of bone.J Bone Joint SurgAm,1999,81(11):1566-1573.
[53] Nair MK,Jyothirmayi R.Radiation therapy in the treatment of giant cell tumor of bone.Ⅰnt J Radiat Oncol Biol Phys,1999,43(5):1065-1069.
[54] Caudell JJ,Ballo MT,Zagars GK,et al.Radiotherapy in the management of giant cell tumor of bone.Ⅰnt J Radiat Oncol Biol Phys,2003,57(1):158-165.
[55] Miszczyk L,Wydmański J,Spindel J.Efficacy of radiotherapy for giant cell tumor of bone:given either postoperatively or as sole treatment.Ⅰnt J Radiat Oncol Biol Phys,2001,49(5):1239-1242.
[56] Feigenberg SJ,Marcus Jr RB,Zlotecki RA,et al.Radiation therapy for giant cell tumors of bone.Clin Orthop Relat Res,2003,(411):207-216.
[57] Bhatia S,Miszczyk L,Roelandts M,et al.Radiotherapy for marginally resected,unresectable or recurrent giant cell tumor of the bone:a rare cancer network study.Rare Tumors,2011,3(4):e48.
[58] Ruka W,Rutkowski P,Morysiński T,et al.The megavoltage radiation therapy in treatment of patients with advanced or difficult giant cell tumors of bone.Ⅰnt J Radiat Oncol Biol Phys,2010,78(2):494-498.
[59] Kantin AV,Shimanovskaia KB,Rokhlin GD.X-ray analy-sis of the results of radiation therapy for giant cell tumors.Vopr Onkol,1972,18(12):46-49.
[60] Hug EB,Muenter MW,Adams JA,et al.3-D-conformal radiation therapy for pediatric giant cell tumors of the skull base.Strahlenther Onkol,2002,178(5):239-244.
[61] Roeder F,Timke C,Zwicker F,et al.Ⅰntensity modulated radiotherapy(ⅠMRT)in benign giant cell tumors--a single institution case series and a short review of the literature.Radiat Oncol,2010,5:18.
[62] Chawla S,Henshaw R,Seeger L,et al.Safety and efficacy of denosumab for adults and skeletally mature adolescents with giant cell tumour of bone:interim analysis of an openlabel,parallel-group,phase 2 study.Lancet Oncol,2013,14(9):901-908.
[63] Thomas D,Henshaw R,Skubitz K,et al.Denosumab in patients with giant-cell tumour of bone:an open-label,phase 2 study.Lancet Oncol,2010,11(3):275-280.
[64] Branstetter DG,Nelson SD,Manivel JC,et al.Denosumab induces tumor reduction and bone formation in patients with giant-cell tumor of bone.Clin Cancer Res,2012,18(16):4415-4424.
[65] Rutkowski P,Ferrari S,Grimer RJ,et al.Surgical downstaging in an open-label phase ⅠⅠtrial of denosumab in patients with giant cell tumor of bone.Ann Surg Oncol,2015,22(9):2860-2868.
[66] 杨毅,郭卫,杨荣利,等.地诺单抗治疗复发或难治骨巨细胞瘤疗效和安全性的初步观察.中国骨与关节杂志,2016,5(1):19-23.
[67] Fusco V,Rossi M,De Martino Ⅰ,et al.Ⅰncidence of osteonecrosis of the jaw(ONJ)in cancer patients with bone metastases treated with bisphosphonates and/or denosumab:some comments and questions.Acta Clin Belg,2018,73(2):163-164.
[68] Lin PP,Guzel VB,Moura MF,et al.Long-term follow-up of patients with giant cell tumor of the sacrum treated with selective arterial embolization.Cancer,2002,95(6):1317-1325.
[69] Hosalkar HS,Jones KJ,King JJ,et al.Serial arterial embolization for large sacral giant-cell tumors:mid-to long-term results.Spine(Phila Pa 1976),2007,32(10):1107-1115.
[70] Onishi H,Kaya M,Wada T,et al.Giant cell tumor of the sacrum treated with selective arterial embolization.Ⅰnt J Clin Oncol,2010,15(4):416-419.
[71] Emori M,Kaya M,Sasaki M,et al.Pre-operative selective arterial embolization as a neoadjuvant therapy for proximal humerus giant cell tumor of bone:radiological and histological evaluation.Jpn J Clin Oncol,2012,42(9):851-855.
[72] Kaiser U,Neumann K,Havemann K.Generalised giant-cell tumour of bone:successful treatment of pulmonary metastases with interferon alpha,a case report.J Cancer Res Clin Oncol,1993,119(5):301-303.
[73] Wei F,Liu X,Liu Z,et al.Ⅰnterferon alfa-2b for recurrent and metastatic giant cell tumor of the spine:report of two cases.Spine(Phila Pa 1976),2010,35(24):E1418-E1422.
[74] Cheng JC,Johnston JO.Giant cell tumor of bone.Prognosis and treatment of pulmonary metastases.Clin Orthop Relat Res,1997,(338):205-214.
[75] Siebenrock KA,Unni KK,Rock MG.Giant-cell tumour of bone metastasising to the lungs.A long-term follow-up.J Bone Joint Surg Br,1998,80(1):43-47.
[76] Dominkus M,Ruggieri P,Bertoni F,et al.Histologically verified lung metastases in benign giant cell tumours--14 cases from a single institution.Ⅰnt Orthop,2006,30(6):499-504.
[77] Viswanathan S,Jambhekar NA.Metastatic giant cell tumor of bone:are there associated factors and best treatment modalities?Clin Orthop Relat Res,2010,468(3):827-833.
[78] Oliveira VC,van der Heijden L,van der GeestⅠC,et al.Giant cell tumours of the small bones of the hands and feet:long-term results of 30 patients and a systematic literature review.Bone Joint J,2013,95-B(6):838-845.
[79] Raskin KA,Schwab JH,Mankin HJ,et al.Giant cell tumor of bone.JAmAcad Orthop Surg,2013,21(2):118-126.
[80] 郭卫,杨毅,李晓,等.四肢骨巨细胞瘤的外科治疗.中华骨科杂志,2007,27(3):177-182.
[81] Yokouchi M,Arishima Y,Nagano S,et al.Giant cell tumor of the distal phalanx of the fourth toe:a case report.J Foot Ankle Surg,2016,55(2):306-309.
[82] Rajani R,Schaefer L,Scarborough MT,et al.Giant cell tumors of the foot and ankle bones:high recurrence rates after surgical treatment.J FootAnkle Surg,2015,54(6):1141-1145.
[83] Henderson M,Neumeister MW,Bueno RA Jr.Hand tumors: ⅠⅠ.Benign and malignant bone tumors of the hand.Plast Reconstr Surg,2014.133(6):814e-821e.
[84] Gouin F,Dumaine V.Local recurrence after curettage treatment of giant cell tumors in peripheral bones:retrospective study by the GSF-GETO(French Sarcoma and Bone Tumor Study Groups).Orthop Traumatol Surg Res,2013,99(6 Suppl):S313-S318.
[85] Zhen W,Yaotian H,Songjian L,et al.Giant-cell tumour of bone.The long-term results of treatment by curettage and bone graft.J Bone Joint Surg Br,2004,86(2):212-216.
[86] van der Heijden L,Dijkstra PD,van de Sande MA,et al.The clinical approach toward giant cell tumor of bone.Oncologist,2014,19(5):550-561.
[87] Capanna R,Fabbri N,Bettelli G.Curettage of giant cell tumor of bone.The effect of surgical technique and adjuvants on local recurrence rate.Chir Organi Mov,1990,75(1 Suppl):206.
[88] Malawer MM,Bickels J,MellerⅠ,et al.Cryosurgery in the treatment of giant cell tumor.A long-term followup study.Clin Orthop Relat Res,1999,(359):176-188.
[89] Malhotra R,Kiran Kumar GN,K Digge V,et al.The clinical and radiological evaluation of the use of an allograftprosthesis composite in the treatment of proximal femoral giant cell tumours.Bone Joint J,2014,96-B(8):1106-1110.[90]Taraz-Jamshidi MH,Gharadaghi M,Mazloumi SM,et al.Clinical outcome of en-block resection and reconstruction with nonvascularized fibular autograft for the treatment of giant cell tumor of distal radius.J Res Med Sci,2014,19(2):117-121.
[91] Bini SA,Gill K,Johnston JO.Giant cell tumor of bone.Curettage and cement reconstruction.Clin Orthop Relat Res,1995,(321):245-250.
[92]Gao ZH,Yin JQ,Xie XB,et al.Local control of giant cell tumors of the long bone after aggressive curettage with and without bone cement.BMC Musculoskelet Disord,2014,15:330.
[93] Zuo D,Zheng L,Sun W,et al.Contemporary adjuvant polymethyl methacrylate cementation optimally limits recurrence in primary giant cell tumor of bone patients compared to bone grafting:a systematic review and meta-analysis.World J Surg Oncol,2013,11:156.
[94] Vult von Steyern F,Bauer HC,Trovik C,et al.Treatment of local recurrences of giant cell tumour in long bones after curettage and cementing.A Scandinavian Sarcoma Group study.J Bone Joint Surg Br,2006,88(4):531-535.
[95] Oda Y,Miura H,Tsuneyoshi M,et al.Giant cell tumor of bone:oncological and functional results of long-term follow-up.Jpn J Clin Oncol,1998,28(5):323-328.
[96] 杨正明,陶惠民,杨迪生,等.邻膝关节骨巨细胞瘤外科治疗的选择.中华外科杂志,2006,44(24):1693-1698.
[97] 杨迪生,严世贵.病损内处置与整块切除治疗邻膝关节骨巨细胞瘤的比较观察.中国矫形外科杂志,1999,(8):5-7.
[98] Campanacci L,Alì N,Casanova JM,et al.Resurfaced allograft-prosthetic composite for proximal tibial reconstruction in children:intermediate-term results of an original technique.J Bone Joint SurgAm,2015,97(3):241-250.
[99] Balke M,Ahrens H,Streitbuerger A,et al.Treatment options for recurrent giant cell tumors of bone.J Cancer Res Clin Oncol,2009,135(1):149-158.
[100] Wojcik J,Rosenberg AE,Bredella MA,et al.Denosumabtreated giant cell tumor of bone exhibits morphologic overlap with malignant giant cell tumor of bone.Am J Surg Pathol,2016,40(1):72-80.
[101] Tubbs WS,Brown LR,Beabout JW,et al.Benign giantcell tumor of bone with pulmonary metastases:clinical findings and radiologic appearance of metastases in 13 cases.AJRAm J Roentgenol,1992,158(2):331-334.
[102] Wang H,Wan N,Hu Y.Giant cell tumour of bone:a new evaluating system is necessary.Ⅰnt Orthop,2012,36(12):2521-2527.
[103] Mendenhall WM,Zlotecki RA,Scarborough MT,et al.Giant cell tumor of bone.Am J Clin Oncol,2006,29(1):96-99.[104]Teuscher J,Aeberhard P,Ganz R.Combined abdominosacral excision of a giant-cell tumor of the os sacrum.Helv ChirActa,1980,46(5-6):751-753.[Article in German]
[105] 郭卫,汤小东,李晓,等.骨盆和骶骨骨巨细胞瘤的治疗策略.中华外科杂志,2008,46(7):501-505.
[106] Guo W,Ji T,Tang X,et al.Outcome of conservative surgery for giant cell tumor of the sacrum.Spine(Phila Pa 1976),2009,34(10):1025-1031.
[107] Dawson GR Jr.Giant-cell tumor of the pelvis at the acetabulum,ilium,ischium,and pubis.J Bone Joint Surg Am,1955,37-A(6):1278-1280.
[108] Sanjay BK,Frassica FJ,Frassica DA,et al.Treatment of giant-cell tumor of the pelvis.J Bone Joint Surg Am,1993,75(10):1466-1475.
[109] Guo W,Sun X,Zang J,et al.Ⅰntralesional excision versus wide resection for giant cell tumor involving the acetabulum:which is better?Clin Orthop Relat Res,2012,470(4):1213-1220.
[110] Luo Y,Duan H,Liu W,et al.Clinical evaluation for lower abdominal aorta balloon occluding in the pelvic and sacral tumor resection.J Surg Oncol,2013,108(3):148-151.
[111] Gitelis S,Mallin BA,Piasecki P,et al.Ⅰntralesional excision compared with en bloc resection for giant-cell tumors of bone.J Bone Joint SurgAm,1993,75(11):1648-1655.
[112] Mi C,Lu H,Liu H.Surgical excision of sacral tumors assisted by occluding the abdominal aorta with a balloon dilation catheter:a report of 3 cases.Spine(Phila Pa 1976),2005,30(20):E614-E616.
[113] Althausen PL,Schneider PD,Bold RJ,et al.Multimodality management of a giant cell tumor arising in the proximal sacrum:case report.Spine(Phila Pa 1976),2002,27(15):E361-E365.
[114] Marcove RC,Sheth DS,Brien EW,et al.Conservative surgery for giant cell tumors of the sacrum.The role of cryosurgery as a supplement to curettage and partial excision.Cancer,1994,74(4):1253-1260.
[115] Randall RL.Giant cell tumor of the sacrum.Neurosurg Focus,2003,15(2):E13.
[116] Doita M,Harada T,Ⅰguchi T,et al.Total sacrectomy and reconstruction for sacral tumors.Spine(Phila Pa 1976),2003,28(15):E296-E301.
[117] Tomita K,Tsuchiya H.Total sacrectomy and reconstruction for huge sacral tumors.Spine(Phila Pa 1976),1990,15(11):1223-1227.
[118] Wuisman P,Lieshout O,Sugihara S,et al.Total sacrectomy and reconstruction:oncologic and functional outcome.Clin Orthop Relat Res,2000,(381):192-203.
[119] Leggon RE,Zlotecki R,Reith J,et al.Giant cell tumor of the pelvis and sacrum:17 cases and analysis of the literature.Clin Orthop Relat Res,2004,(423):196-207.
[120] Ozaki T,Liljenqvist U,Halm H,et al.Giant cell tumor of the spine.Clin Orthop Relat Res,2002,(401):194-201.
[121] Martin C,McCarthy EF.Giant cell tumor of the sacrum and spine:series of 23 cases and a review of the literature.Ⅰowa Orthop J,2010,30:69-75.
[122] 于秀淳,刘晓平,付志厚,等.反复选择性动脉栓塞及刮除术治疗高位骶骨骨巨细胞瘤的远期疗效.中华肿瘤杂志,2013,35(3):233-235.
[123] Ming Z,Kangwu C,Huilin Y,et al.Analysis of risk factors for recurrence of giant cell tumor of the sacrum and mobile spine combined with preoperative embolization.Turk Neurosurg,2013,23(5):645-652.
[124] Min K,Espinosa N,Bode B,et al.Total sacrectomy and reconstruction with structural allografts for neurofibrosarcoma of the sacrum.A case report.J Bone Joint Surg Am,2005,87(4):864-869.
[125] Nishizawa K,Mori K,Saruhashi Y,et al.Long-term clinical outcome of sacral chondrosarcoma treated by total en bloc sacrectomy and reconstruction of lumbosacral and pelvic ring using intraoperative extracorporeal irradiated autologous tumor-bearing sacrum:a case report with 10 years follow-up.Spine J,2014,14(5):e1-e8.
[126] Hays RP.Resection of the sacrum for benign giant cell tumor:a case report.Ann Surg,1953,138(1):115-120.
[127]Stener B,Gunterberg B.High amputation of the sacrum for extirpation of tumors.Principles and technique.Spine(Phila Pa 1976),1978,3(4):351-366.
[128] Gunterberg B,Romanus B,Stener B.Pelvic strength after major amputation of the sacrum.An exerimental study.Acta Orthop Scand,1976,47(6):635-642.
[129] Hugate RR Jr,DickeyⅠD,Phimolsarnti R,et al.Mechanical effects of partial sacrectomy:when is reconstruction necessary?Clin Orthop Relat Res,2006,450:82-88.
[130] 罗翼,姜勇,张学磊,等.骶骨高选择性分段切除对骨盆稳定性影响的生物力学研究.华西医学,2013,(10):1536-1540.
[131] Thangaraj R,Grimer RJ,Carter SR,et al.Giant cell tumour of the sacrum:a suggested algorithm for treatment.Eur Spine J,2010,19(7):1189-1194.
[132] Shi W,Ⅰndelicato DJ,Reith J,et al.Radiotherapy in the management of giant cell tumor of bone.Am J Clin Oncol,2013,36(5):505-508.
[133] Chikiamco PS.Radiotherapy of benign giant-cell tumor of bone.J Philipp MedAssoc,1966,42(7):407-421.
[134] Khan DC,Malhotra S,Stevens RE,et al.Radiotherapy for the treatment of giant cell tumor of the spine:a report of six cases and review of the literature.CancerⅠnvest,1999,17(2):110-113.
[135] GibbsⅠC,Chang SD.Radiosurgery and radiotherapy for sacral tumors.Neurosurg Focus,2003,15(2):E8.
[136] Martins AN,Dean DF.Giant cell tumor of sphenoid bone:malignant transformation following radiotherapy.Surg Neurol,1974,2(2):105-107.
[137] Kanamori M,Ohmori K.Curettage and radiotherapy of giantcelltumourofthesacrum:acasereportwitha10-yearfollow-up.JOrthopSurg(HongKong),2005,13(2):171-173.
[138] Osaka S,Toriyama S.Surgical treatment of giant cell tumors ofthepelvis.ClinOrthopRelatRes,1987,(222):123-131.
[139] Kattapuram AS,O'Donnell RJ,Huszar M,et al.Surgical management of innominate giant cell tumor.Clin Orthop Relat Res,1996,(329):281-287.
[140] Leggon RE,Zlotecki R,Reith J,et al.Giant cell tumor of the pelvis and sacrum:17 cases and analysis of the literature.Clin Orthop Relat Res,2004,(423):196-207.
[141] Clarke MJ,Zadnik PL,Groves ML,et al.En bloc hemisacrectomy and internal hemipelvectomy via the posterior approach.J Neurosurg Spine,2014,21(3):458-467.
[142] Thangaraj R,Grimer RJ,Carter SR,et al.Giant cell tumour of the sacrum:a suggested algorithm for treatment.Eur Spine J,2010,19(7):1189-1194.
[143] Salai M,Garniek A,Rubinstein Z,et al.Preoperative angiography and embolization of large pelvic tumors.J Surg Oncol,1999,70(1):41-44.
[144] Wirbel RJ,Roth R,Schulte M,et al.Preoperative embolization in spinal and pelvic metastases.J Orthop Sci,2005,10(3):253-257.
[145] Chiras J,Gagna G,Rose M,et al.Arteriography and embolization of tumors of the sacrum.Rev Chir Orthop ReparatriceAppar Mot,1987,73(2):99-103.
[146] Zhou M,Yang H,Chen K,et al.Surgical treatment of giant cell tumors of the sacrum and spine combined with pre-operative transarterial embolization.Oncol Lett,2013,6(1):185-190.
[147] Ji T,Yang Y,Wang Y,et al.Combining of serial embolization and denosumab for large sacropelvic giant cell tumor:Case report of 3 cases.Medicine(Baltimore),2017,96(33):e7799.
[148] Xu W,Li X,Huang W,et al.Factors affecting prognosis of patients with giant cell tumors of the mobile spine:retrospective analysis of 102 patients in a single center.Ann Surg Oncol,2013,20(3):804-810.
[149] 吴志鹏,肖建如,杨兴海,等.脊柱骨巨细胞瘤外科治疗复发相关因素的回顾性分析.国际骨科学杂志,2010,31(6):387-389,391.
[150] Fidler MW.Surgical treatment of giant cell tumours of the thoracic and lumbar spine:report of nine patients.Eur Spine J,2001,10(1):69-77.
[151] Hart RA,Boriani S,Biagini R,et al.A system for surgical staging and management of spine tumors.A clinical outcome study of giant cell tumors of the spine.Spine(Phila Pa 1976),1997,22(15):1773-1782;discussion 1783.
[152] Boriani S,Biagini R,DeⅠure F,et al.En bloc resections of bone tumors of the thoracolumbar spine.A preliminary report on 29 patients.Spine(Phila Pa 1976),1996,21(16):1927-1931.
[153] Boriani S,Weinstein JN,Biagini R.Primary bone tumors of the spine.Terminology and surgical staging.Spine(Phila Pa 1976),1997,22(9):1036-1044.
[154] Tomita K,Kawahara N,Baba H,et al.Total en bloc spondylectomy.Anewsurgicaltechniqueforprimarymalignantvertebraltumors.Spine(PhilaPa1976),1997,22(3):324-333.
[155] 郭卫,李大森,杨毅,等.脊柱骨巨细胞瘤的手术治疗策略.中国脊柱脊髓杂志,2009,19(12):899-903.
[156] 石磊,姜亮,刘晓光,等.胸腰椎骨巨细胞瘤手术治疗后复发的原因分析.中国脊柱脊髓杂志,2013,23(9):815-820.
[157] Yin H,Yang X,Xu W,et al.Treatment and outcome of primary aggressive giant cell tumor in the spine.Eur Spine J,2015,24(8):1747-1753.
[158] 许炜,徐乐勤,李磊,等.脊柱骨巨细胞瘤术后复发的预后因素.中华骨科杂志,2014,34(4):487-493.
[159] Jones KB,DeYoung BR,Morcuende JA,et al.Ethanol as a local adjuvant for giant cell tumor of bone.Ⅰowa Orthop J,2006,26:69-76.
[160] Teixeira LE,Vilela JC,Miranda RH,et al.Giant cell tumors of bone:nonsurgical factors associated with local recurrence.Acta Orthop Traumatol Turc,2014,48(2):136-140.
[161] Kremen TJ Jr,Bernthal NM,Eckardt MA,et al.Giant cell tumor of bone:are we stratifying results appropriately?Clin Orthop Relat Res,2012,470(3):677-683.
[162] Guzman R,Dubach-Schwizer S,Heini P,et al.Preoperative transarterial embolization of vertebral metastases.Eur Spine J,2005,14(3):263-268.
[163] Mestiri M,Bouabdellah M,Bouzidi R,et al.Giant cells tumor recurrence at the third lumbar vertebra.Orthop Traumatol Surg Res,2010,96(8):905-909.
[164] Michalowski MB,Pagnier-Clémence A,Chirossel JP,et al.Giant cell tumor of cervical spine in an adolescent.Med Pediatr Oncol,2003,41(1):58-62.

