Perspectives on “the biology of spinal cord regeneration success and failure”
In our recently co‐authoredPhysiological Reviewsmanuscript entitled “The biology of regeneration failure and success after spinal cord injury” (Tran et al., 2018b), we sought to provide a comprehensive and up‐to‐date de‐scription of how the glial scar develops following spinal cord injury (SCI)to chronically inhibit axon regeneration. Our additional intention was to clarify some of the confusion in the field relating to an oversimpli fied view of the glial scar. We would like to take this opportunity to reiterate how the current body of literature, expounding details of the glial scar, has progressed beyond a simpli fied and outdated understanding of this struc‐ture as a mono‐cellular arrangement consisting only of astrocytes that solely limit axon regeneration. Instead, our perception of the glial scar has evolved to acknowledge the nuances of this multi‐cellular structure to one that is able to limit the expansion of in flammatory processes shortly following SCI and that also persists chronically to limit axon regeneration.Further, we would like to expand upon some of the details presented in the review by offering an outlook on the current state of the field and avenues for progression. This includes the specific role of chondroitin sulphate proteoglycan components in axonal growth and plasticity, and the current assessment of SCI at different stages post injury. As such, this perspective should be considered a companion piece to our original work,adding new insights from across the field from recent publications.
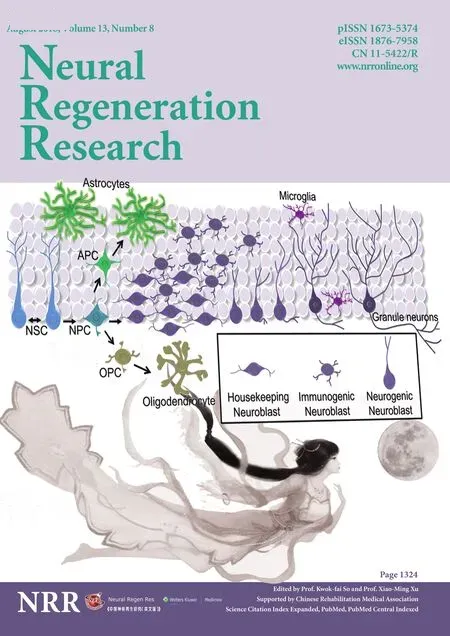
A multicellular view of the glial scar:While astrocytes have been the most prevalently studied component of the glial scar, and are undoubtedly an important functional component, this tissue additionally comprises many other glial and cellular constituents including oligodendrocyte pro‐genitor cells, microglia, macrophages, and fibroblasts/pericytes. Together,these various cell types respond to the in flammatory milieu initiated by injury by becoming “reactive.” Often, this stereotyped response includes such cellular changes as hypertrophy, increased motility, self‐proliferation,and a great production of pro‐in flammatory factors. Reactive astrocytes,for example, exhibit increased upregulation of intermediate filament pro‐teins such as glial fibrillary acidic protein (GFAP), hypertrophy, and other changes in morphology when exposed to a pro‐inflammatory environ‐ment (Hara et al., 2017). It is this reactive glial response that provides an inhibitory environment to axonal regeneration chronically. This is further contrasted by the remarkable regenerative properties of invertebrates such as zebrafish which, in addition to displaying extensive neurogenesis in adulthood, show limited in flammatory responses that avoid scar forma‐tion chronically (Baumgart et al., 2012; Becker et al., 2018). The capacity for regeneration following SCI in the adult has been lost in warm‐blooded species during the processes of development and evolution. Subsequent‐ly, the difference in cellular and molecular responses to trauma between mammals, anurans, birds, and marsupials requires substantial investiga‐tion to inform novel treatment strategies.
The ultimate effect of reactive glia is to produce an orchestrated restruc‐turing of the tissue at the lesion site to culminate in a complex arrange‐ment of cells and extracellular components we call the glial scar. Along with astrocytes overlaid to form a wall‐like formation at the scar border,the glial scar penumbra also includes neural/glial antigen 2 positive (NG2+)oligodendrocyte progenitor cells. The extracellular components emanat‐ing from the lesion penumbra include chondroitin sulfate proteoglycans(CSPGs) including NG2 and other lecticans that contribute to potently inhibiting axon regeneration chronically. Further cellular dissection of the mature glial scar will reveal a stereotyped cellular organization beginning with a fibrotic epicenter consisting of fibroblasts, macrophages, and extra‐cellular matrix proteins such as laminin, collagen type I and fibronectin.Arising from this organization is the reformation of a glial limitans initiat‐ed through cell‐to‐cell contact from fibroblasts/pericytes and astrocytes of the surrounding penumbra. Importantly, this structure serves to segregate inflammatory cells and other elements (e.g., newly forming blood ves‐sels) at the lesion epicenter. Recent studies are beginning to highlight the potently pro‐in flammatory effects of the fibrotic components of the scar.Collagen type I alone has, for example, been shown to activate astrocytes,propelling them to form a tight, wall‐like scar (Hara et al., 2017). Work from Dias et al. (2018) additionally highlights the contribution of type‐A pericytes, which differentiate into fibroblasts to further restrict axon out‐growth following injury to the cord. These recent findings further empha‐size that more work will be needed to fully understand the impact of the fibrotic component of the glial scar and whether targeting this structure,along with the astroglial wall, will provide functional recovery following SCI.
Clearly, the glial scar does not exist to only limit axon regeneration chronically. Inherent in this complicated meshwork of cells is the effec‐tive ability to stabilize rampant in flammatory processes shortly following injury as seen in the reformation of the glia limitans as the scar matures.Ablating the ability of astrocytes to become reactive, for example, through genetically ablating GFAP or Vimentin has been reported to increase le‐sion volume and exacerbate in flammation‐induced injury in some cases.Work from the Sofroniew lab has additionally shown the importance of a reactive astrocyte response following stab injuries to the spinal cord.Genetically ablating signal transducer and activator of transcription 3(STAT3), for example, and preventing astrocytes from forming a wall around the injury epicenter induced worse functional recovery than wild type controls (Wanner et al., 2013). Our current understanding of the glial scar should, therefore, resist oversimplification of this structure to encompass a more nuanced understanding of the remarkable plasticity of astrocytes based on the extent of in flammation within the injured en‐vironment. This is in contrast to interpretations made by Anderson et al.(2016), which claim that reactive astrocytes have only one state and that“contrary to the prevailing dogma, astrocyte scar formation aids rather than prevents central nervous system axon regeneration”. The in fluence of the in flammatory context in which astrocytes find themselves can be fur‐ther exempli fied by recent work from the Okada group, which highlights the malleability of reactive astrocytes by implanting them in naïve or in‐jured spinal cords. Reactive astrocytes, for example, implanted into naïve cords became non‐reactive while those implanted into injured cords ad‐opted scar‐like morphological changes (Hara et al., 2017). Inhibiting the wall‐like state sub‐acutely rather than immediately after injury promoted axonal regeneration (Hara et al., 2017). Thus, the extent of the inflam‐matory milieu following injury induces cellular reactivity to bene ficially limit the spread of in flammation. The chronic persistence of the glial scar including its fibrotic and CSPG components, however, ultimately hinders axon regeneration and restoration of function. While there are several strategies that are in pre‐clinical assessment including intracellular sigma peptide (ISP; a CSPG receptor blocking molecule) and viral delivery of chondroitinase ABC (Bartus et al., 2014; Lang et al., 2015), there currently exists no treatment for SCI scar modi fication that is ready to be assessed in the human patient. This may limit the success of strategies for SCI treatment currently under clinical trial, such as the implantation of au‐tologous Schwann cells. Continued development and assessment of such new treatments may be key for future success in clinical trials.
CSPGs and their component structure:Within our review, we concen‐trated on the traditional role of CSPGs following SCI to inhibit growth, re‐generation and plasticity. These data are well established in the literature,with numerousin vitroandin vivostudies showing how they are upreg‐ulated following SCI within the glial scar initially to aid neuroprotection but ultimately act to limit growth and functional recovery. However, while this class of large macromolecules, in general, upregulate following spinal trauma, there is substantial evidence to show that the different CSPG lec‐ticans up‐ and down‐regulate both mRNA and protein expression at dif‐ferent time points following trauma. This creates a well characterized pat‐tern of CSPG changes that, to some extent, varies depending on the size,location and type of injury (Andrews et al., 2012). Studies have shown that the different CSPG lecticans broadly perform the same functions.However, recent evidence has demonstrated that brevican alone mediates cellular activity through the gating of parvalbumin positive interneurons within the structure of the perineuronal net (Favuzzi et al., 2017). Indeed,this CSPG acts to control α‐amino‐3‐hydroxy‐5‐methyl‐4‐isoxazolepropi‐onic acid (AMPA) receptor input and potassium channel localization, reg‐ulating cellular excitability. This, in turn, was shown to regulate brevican levels. These data are of substantial signi ficance as they demonstrate that the individual CSPGs may act independently and dynamically to modify specific cellular responses in precise ways. These data may signify how alterations in speci fic CSPG levels and expression within the central ner‐vous system are associated with the wide variety of neurological disorders and diseases mentioned within our review (Tran et al., 2018b). As such, it may be of exceptional importance for the success of speci fic SCI treatment strategies, and the recovery of function following injury, to assess which CSPGs are expressed at different times and precisely when we act to mod‐ify their inhibitory in fluence upon regeneration.
The speci fic function of CSPGs following SCI may be further compli‐cated. Within ourPhysiological Reviewsarticle, we brie fly touched upon the notion that the glycosaminoglycan (GAG) chains of the upregulated CSPGs are differently sulfated after SCI with chondroitin sulphate (CS)‐A,‐C, and ‐E predominating. Indeed, Brown et al. (2012) suggest the con‐sequence of CS‐E upregulation following SCI is of particular importance as this residue not only inhibits axon growth post injury, but also acts to bind with the CSPG receptor protein tyrosine phosphatase sigma (RPTPσ).However, this is of exceptional importance to the function of these mac‐romolecules, where subtle differences in sulphation may cause opposing effects on neuronal activity. For example, an increase in the ratio of 4‐sul‐phated GAGs to 6‐sulphated GAGs in perineuronal nets may decrease synaptic plasticity in aged animals (Foscarin et al., 2017), while knockout studies have shown that 6‐sulphation of CS‐C facilitates growth (Lin et al., 2011). Indeed, the effects of speci fic CSPG sulphation patterns upon neuronal activity is likely to be of exceptional importance to the growth and recovery of individuals following SCI as these macromolecules are a prominent feature of the extracellular matrix surrounding all cells of the central nervous system. Similarly, sulphation patterns affect the interac‐tions and binding of CSPGs with receptors such as RPTPσ, the Nogo‐66 receptors 1 and 3 (NgR1 and 3), and (potentially) semaphorins. Indeed,recent investigations have confirmed the affinity of CS‐E for RPTPσ,while CS‐A and ‐E potentially dock with NgR1nd 3 (Griffith et al., 2017).Further, the GAG sulphation affects CSPG association with guidance mol‐ecules (ephrins, Wnts,etc.), growth factors ( fibroblast growth factor, glial cell‐derived neurotrophic factor,etc.), and other molecules of the extracel‐lular matrix (integrins, tenascins,etc.). It is of exceptional importance to both determine the biological function of these speci fic sulphotransferases and the exact mechanism and pathways through which CSPGs bind and mediate their speci fic function to ascertain how they may be best manipu‐lated for the treatment of SCI.
A final complication of CSPG alteration in the treatment of SCI cur‐rently includes that the mechanism of receptor‐mediated inhibition is still largely unknown. Within our recentPhysiological Reviewsarticle we described at length the newly discovered conjugate CSPG receptors RPTPσ and LAR (leukocyte common antigen‐related phosphatase), their relation to intrinsic and extrinsic neuronal growth properties, and their putative signaling cascades (Tran et al., 2018b). Understanding the path‐ways downstream of RPTPσ is also critical to regeneration and treatment strategies in light of a recent publication from our laboratory where we show that Cathepsin B characterizes protease activity in peripheral axons following RPTPσ modulation with the synthetic peptide ISP (Tran et al., 2018a). Further, ISP modulation of RPTPσ in a post‐injury environ‐ment has revealed that local and systemically‐infiltrating immune cells also respond to RPTPσ (Dyck et al., 2018). Collectively these data show that CSPG‐receptor dynamics are not only limited to the leading edge of axons, but to the many components of the glial scar as well, further con‐tributing to the complexity of the post‐injury environment and potential treatment of any SCI.
The stages of SCI:Within our review, we discuss the primary and second‐ary stages of SCI, paying particular attention to the biological processes involved in this traumatic progression of damage, inflammation and cellular death. We also describe experimental pre‐clinical injury models as being at acute or chronic stages following trauma. These de finitions are largely subjective. Acute phases of injury are broadly defined as occur‐ring two hours to two weeks following trauma. However, the time point when an injury becomes chronic is typically based upon the idiosyncratic judgement of each investigator grounded upon the literature of the spe‐ci fic discipline in which they are working. As such, ‘chronic’ injuries have been de fined as starting as early as two weeks’ to six months’ post trauma.Indeed, even after this time point, spinal injury can still be defined as dynamic with continued scar development and progressive alterations to neural circuitry (Kwon et al., 2002). Respiratory motor function has been shown to have some degree of spontaneous recovery following chronic SCI (Fuller et al., 2008), although the reason for this remains unclear.Although less explored then acute injuries, there are numerous investi‐gations into SCI and treatment application at early chronic time points.However, largely due to ethical and financial concerns, very few papers are written which examine these issues at extended lengths (six months +)post injury. This represents a gap in the current knowledge base, especially when one considers that clinical SCI ‘chronic’ injuries are typically de‐fined as being over one year post trauma, which is when most individuals experience the greatest degree of functional recovery. Chronic injuries are typically considered a difficult environment in which to mediate function‐al recovery, but this is not necessarily what is observed clinically. Howev‐er, experimental studies have not traditionally assessed spinal tissue long after the initial insult, and thus, there is little data available to assess why this occurs. Greater assessment of alterations to the spinal cord at extend‐ed chronic stages will be essential for the continued understanding of SCI progression and potentially successful treatment, and ultimately recovery,of the current SCI population.
Concluding remarks:Our view of SCI post injury has developed over recent years from a simplistic view of the factors and molecules acting to inhibit growth to something more complex and nuanced involving a large cast of interacting and transforming cells and processes which integrate to prevent functional restoration of activity. However, we believe that the continued understanding and exploration of these processes and the mi‐nutia of the changes which occur holds the key to the successful develop‐ment of combination and strati fied treatment strategies that will facilitate recovery at all stages post injury.
PMW and JS were funded by the International Spinal Research Trust, Wings for Life, and the Craig H. Neilsen Foundation. APT and JS were funded by NINDS NS025713, The Hong Kong Spinal Cord Injury Fund, and The Brumagen/Nelsen Fund.
Philippa Mary Warren#, Amanda Phuong Tran#, Jerry Silver*School of Biomedical Sciences, University of Leeds, Leeds, UK(Warren PM)Department of Neurosciences, Case Western Reserve University, Cleveland,Ohio, USA (Tran AP, Silver J)
*Correspondence to:Jerry Silver, Ph.D., jxs10@case.edu.
#These two authors contributed to the work equally.
orcid:0000-0001-5002-2599 (Jerry Silver)
Accepted:2018-06-02
doi:10.4103/1673-5374.235226
Copyright transfer agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Jennifer L. Seifert, TissueGen, Inc., USA.
- 中国神经再生研究(英文版)的其它文章
- In Memoriam: Ray Grill (1966–2018)
- Reorganization of injured anterior cingulums in a hemorrhagic stroke patient
- A novel chronic nerve compression model in the rat
- Analgesic effect of AG490, a Janus kinase inhibitor, on oxaliplatin-induced acute neuropathic pain
- Three-dimensional visualization of the functional fascicular groups of a long-segment peripheral nerve
- Novel conductive polypyrrole/silk fibroin scaffold for neural tissue repair