血清降钙素原和可溶性髓样细胞触发受体-1及可溶性CD14亚型水平联合预测脓毒症患者28 d病死率的价值研究
毛 云,盛孝燕,朱红阳,景道远
·论著·
血清降钙素原和可溶性髓样细胞触发受体-1及可溶性CD14亚型水平联合预测脓毒症患者28 d病死率的价值研究
毛 云,盛孝燕*,朱红阳,景道远
目的探讨血清降钙素原(PCT)、可溶性髓样细胞触发受体-1(sTREM-1)、可溶性CD14亚型(Presepsin)水平联合预测脓毒症患者28 d病死率的价值。方法选取2014年7月—2016年4月金华市中心医院急诊重症监护室(EICU)和感染科收住的确诊为脓毒症的患者97例。收集患者一般资料,检测其入院后第1天血清C反应蛋白(CRP)、PCT、sTREM-1、Presepsin水平。随访28 d,记录患者生存情况。血清PCT、sTREM-1、Presepsin水平与急性生理学及慢性健康状况评分系统(APACHE Ⅱ)评分的相关性分析采用Pearson相关分析;脓毒症患者28 d病死率的影响因素分析及血清PCT、sTREM-1、Presepsin水平联合的Logistic回归方程的计算采用多因素Logistic回归分析;绘制APACHE Ⅱ评分,血清PCT、sTREM-1、Presepsin水平及后3个指标联合评估脓毒症患者预后的受试者工作特征曲线(ROC曲线)。结果随访28 d后,28例(28.9%)患者死亡。根据随访结果,将患者分为死亡组(28例)和生存组(69例)。死亡组APACHEⅡ评分和血清CRP、PCT、sTREM-1、Presepsin水平高于生存组(P<0.05)。血清PCT、sTREM-1、Presepsin水平与APACHE Ⅱ评分均呈正相关(P<0.05)。多因素Logistic回归分析结果显示,APACHE Ⅱ评分〔OR=1.13,95%CI(1.01,1.64)〕及血清PCT〔OR=1.66,95%CI(1.14,2.53)〕、sTREM-1〔OR=2.54,95%CI(1.14,5.83)〕、Presepsin〔OR=25.11,95%CI(1.58,79.7)〕水平是脓毒症患者28 d病死率的影响因素(P<0.05)。APACHE Ⅱ评分和血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的ROC曲线下面积(AUC)分别为0.90〔95%CI(0.82,0.95)〕、0.87〔95%CI(0.78,0.93)〕、0.90〔95%CI(0.82,0.95)〕、0.85〔95%CI(0.77,0.92)〕。血清PCT、sTREM-1、Presepsin水平联合的Logistic回归方程为Y=-1.218 9+0.032 96×PCT+0.061 25×sTREM-1+0.196 8×Presepsin,其预测脓毒症患者28 d病死率的AUC为0.99〔95%CI(0.94,1.00)〕。血清PCT、sTREM-1、Presepsin水平联合预测脓毒症患者28 d病死率的AUC大于APACHE Ⅱ评分和血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的AUC(P<0.05)。结论血清PCT、sTREM-1、Presepsin水平联合预测脓毒症患者28 d病死率的价值优于单一指标,这具有重要的参考价值及临床意义,有助于临床决策。
脓毒症;死亡率;预测;降钙素原;可溶性髓样细胞触发受体-1;可溶性CD14亚型
脓毒症是以感染为诱因,进而引发全身炎性反应失控导致多脏器功能障碍及衰竭的疾病[1]。目前,脓毒症已成为重症监护室(ICU)患者死亡的主要原因之一。多项研究表明,脓毒症的高病死率不但与病情的严重程度相关,而且与能否早期诊断及判断预后密切相关[2-3]。目前脓毒症病情严重程度评估及预后判断的评分系统有序贯器官衰竭评估(SOFA)、Marshall-MODS评分、BJ-MODS评分、简化急性生理评分(SAPS Ⅱ)等[4-6],其中急性生理学及慢性健康状况评分系统(APACHE Ⅱ)是目前临床上ICU应用最广泛、最具权威的危重病病情评价系统。一些非特异性的炎性指标如血清降钙素原(PCT)、和肽素(copeptin)、胰石蛋白(PSP)、超敏C反应蛋白(hs-CRP)、可溶性髓样细胞触发受体-1(sTREM-1)、可溶性CD14亚型(Presepsin)、可溶性尿激酶受体(suPAR)等已被发现对成年脓毒症患者的早期诊断具有一定价值[7-8],但是有关这些炎性指标对脓毒症患者预后评估的研究仍不多。因此本研究探讨血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的价值,对判断感染导致的脓毒症患者病情严重程度及预后具有重要的临床价值。
1 对象与方法
1.1 研究对象 选取2014年7月—2016年4月金华市中心医院急诊重症监护室(EICU)和感染科收住的确诊为脓毒症的患者97例。确诊标准:符合“2001年美国危重病医学会(SCCM)/欧洲重症医学学会(ESICM)/美国胸科医师学会(ACCP)/美国胸科学会(ATS)/外科感染学会(SIS)国际脓毒症定义会议”制定的脓毒症确诊标准[9]。纳入标准:年龄>18岁,住院时间24 h以上。排除标准:妊娠,恶性肿瘤终末期。所有患者签署知情同意书,本研究由金华市中心医院伦理委员会审核通过。
1.2 研究方法
1.2.1 治疗方法 参照“2012国际拯救脓毒症战役”指南[10]给予治疗:早期抗生素治疗、液体复苏、预防应激性溃疡、控制血糖、器官支持及基础病因治疗等。
1.2.2 一般资料收集 入院后24 h内由EICU、感染科医师收集患者性别、年龄、BMI、慢性病(慢性阻塞性肺疾病、脑血管意外后遗症、心脏病、慢性肝肾疾病、糖尿病、血液病、恶性肿瘤)病史等,并评估APACHEⅡ评分。
1.2.3 血清C反应蛋白(CRP)、PCT、sTREM-1、Presepsin水平检测 所有患者入院后第1天即抽取静脉血6 ml,3 000 r/min离心15 min(离心半径8 cm),分离血清,吸取至少3 ml血清于新的促凝管中,于-80 ℃冰箱保存待测。采用微粒子酶联免疫分析法检测血清CRP、PCT水平,ELISA法检测血清sTREM-1、Presepsin水平。
1.2.4 随访 从患者入院后开始随访,每4 d随访1次,共随访28 d,观察患者转归情况,记录存活、死亡例数。

本研究创新点:
目前尚缺乏公认的评估脓毒症患者预后的生物学指标,寻找灵敏、特异的实验室指标来准确诊断脓毒症并判断病情尤为重要,本研究发现,脓毒症患者血清降钙素原(PCT)、可溶性髓样细胞触发受体-1(sTREM-1)、可溶性CD14亚型(Presepsin)水平与急性生理学及慢性健康状况评分系统(APACHE Ⅱ)评分均具有相关性,继而创新性地联合3项血清学指标预测脓毒症患者预后,结果显示,血清PCT、sTREM-1、Presepsin水平联合预测价值优于单一指标预测价值,可为预测脓毒症患者28 d病死率提供有意义的量化指标,提高脓毒症患者近期预后评估准确率,为临床应用优化脓毒症治疗策略提供科学依据。
2 结果
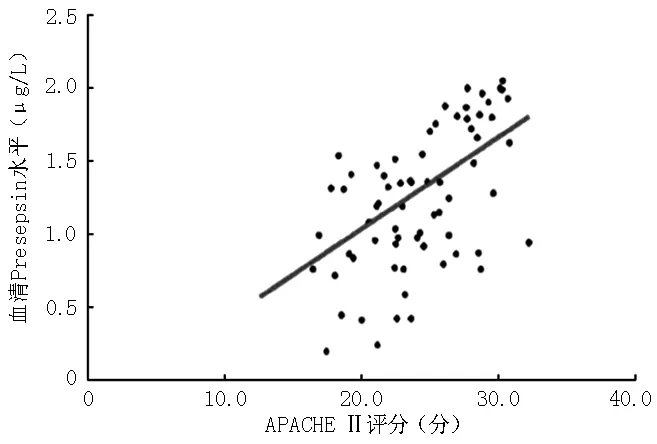
2.1 一般情况 97例患者中,男64例,女33例;年龄33~64岁,平均年龄(49.3±15.2)岁;BMI(21.7±2.7)kg/m2;有慢性病病史73例;APACHEⅡ评分(20.4±8.5)分;CRP(128.9±39.6)g/L;PCT(14.9±4.6)μg/L;sTREM-1(14.8±3.8)μg/L;Presepsin(2.1±1.1)μg/L;随访28 d后,28例(28.9%)患者死亡。根据随访结果,将患者分为死亡组(28例)和生存组(69例)。两组性别、年龄、BMI、慢性病病史情况比较,差异无统计学意义(P>0.05);死亡组APACHEⅡ评分,血清CRP、PCT、sTREM-1、Presepsin水平高于生存组,差异有统计学意义(P<0.05,见表1)。
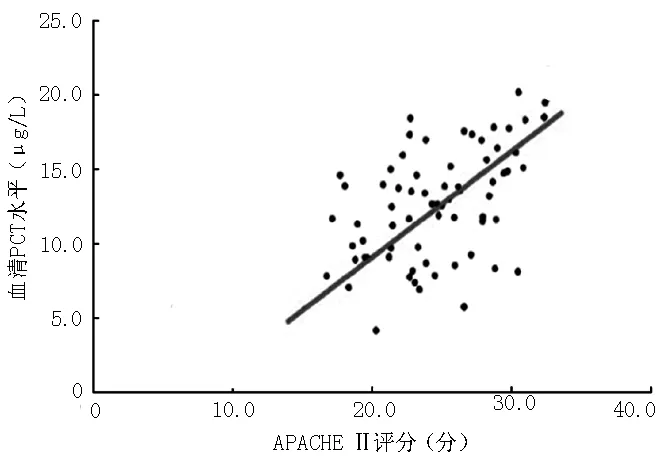
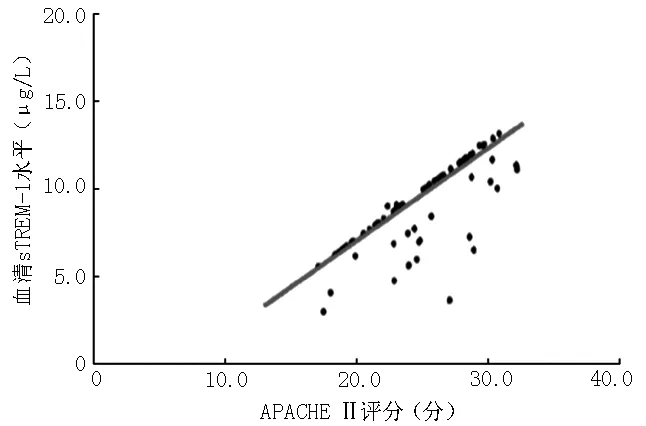
2.2 血清PCT、sTREM-1、Presepsin水平与APACHE Ⅱ评分的相关性分析 血清PCT、sTREM-1、Presepsin水平与APACHE Ⅱ评分均呈正相关(PCT:r=0.479 4,P<0.001;sTREM-1:r=0.752 3,P<0.001;Presepsin:r=0.578 1,P<0.001;见图1~3)。
2.3 脓毒症患者28 d病死率的影响因素分析 以随访结果为因变量(赋值:生存=0,死亡=1),性别(赋值:女=1,男=2)、年龄(连续型变量)、BMI(连续型变量)、慢性病病史情况(赋值:无=0,有=1)、APACHEⅡ评分(连续型变量)及血清CRP(连续型变量)、PCT(连续型变量)、sTREM-1(连续型变量)、Presepsin(连续型变量)水平为自变量,进行多因素Logistic回归分析,结果显示,APACHE Ⅱ评分及血清PCT、sTREM-1、Presepsin水平是脓毒症患者28 d病死率的影响因素(P<0.05,见表2)。
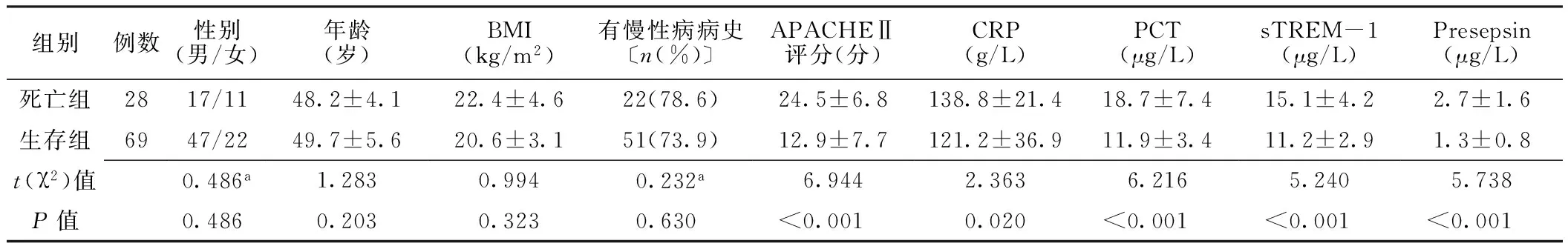
表1 两组患者一般资料和血清CRP、PCT、sTREM-1、Presepsin水平比较
注:a为χ2值;APACHEⅡ=急性生理学及慢性健康状况评分系统,CRP=C反应蛋白,PCT=降钙素原,sTREM-1=可溶性髓样细胞触发受体-1,Presepsin=可溶性CD14亚型
注:PCT=降钙素原,APACHE Ⅱ=急性生理学及慢性健康状况评分系统
图1 血清PCT水平与APACHE Ⅱ评分的相关性
Figure1 Correlation between serum PCT level and APACHE Ⅱ score in patients with sepsis
注:sTREM-1=可溶性髓样细胞触发受体-1
图2 血清sTREM-1水平与APACHE Ⅱ评分的相关性
Figure2 Correlation between serum sTREM-1 level and APACHE Ⅱ score in patients with sepsis
2.4 APACHE Ⅱ评分,血清PCT、sTREM-1、Presepsin水平及其联合预测脓毒症患者28 d病死率的价值 APACHE Ⅱ评分,血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的AUC分别为0.90〔95%CI(0.82,0.95)〕、0.87〔95%CI(0.78,0.93)〕、0.90〔95%CI(0.82,0.95)〕、0.85〔95%CI(0.77,0.92)〕,截断值分别为31.5分、16.1 μg/L、12.3 μg/L、1.5 μg/L,灵敏度分别为82.1%、82.1%、82.1%、100.0%,特异度分别为85.5%、76.8%、79.7%、62.3%,约登指数分别为0.68、0.59、0.62、0.62(见图4)。
注:Presepsin=可溶性CD14亚型
图3 血清Presepsin水平与APACHE Ⅱ评分的相关性
Figure3 Correlation between serum Presepsin level and APACHE Ⅱ score in patients with sepsis
表2 脓毒症患者28 d病死率影响因素的多因素Logistic回归分析
Table2 Multivariate Logistic regression analysis on influencing factors of 28-d mortality in patients with sepsis
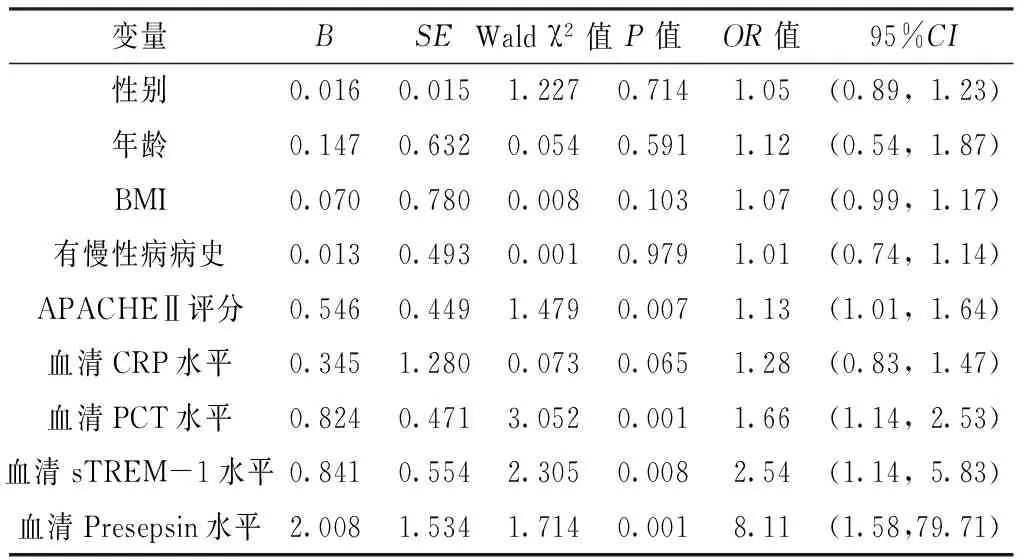
变量BSEWaldχ2值P值OR值95%CI性别0.0160.0151.2270.7141.05(0.89,1.23)年龄0.1470.6320.0540.5911.12(0.54,1.87)BMI0.0700.7800.0080.1031.07(0.99,1.17)有慢性病病史0.0130.4930.0010.9791.01(0.74,1.14)APACHEⅡ评分0.5460.4491.4790.0071.13(1.01,1.64)血清CRP水平0.3451.2800.0730.0651.28(0.83,1.47)血清PCT水平0.8240.4713.0520.0011.66(1.14,2.53)血清sTREM-1水平0.8410.5542.3050.0082.54(1.14,5.83)血清Presepsin水平2.0081.5341.7140.0018.11(1.58,79.71)
以随访结果为因变量(赋值:生存=0,死亡=1),血清CRP、PCT、sTREM-1、Presepsin水平为自变量,进行多因素Logistic回归分析,结果显示,Y=-1.218 9+0.032 96×PCT+0.061 25×sTREM-1+0.196 8×Presepsin,其预测脓毒症患者28 d病死率的AUC为0.99〔95%CI(0.94,1.00)〕,截断值为0.14,灵敏度为96.4%,特异度为97.1%,约登指数为0.94(见图4)。
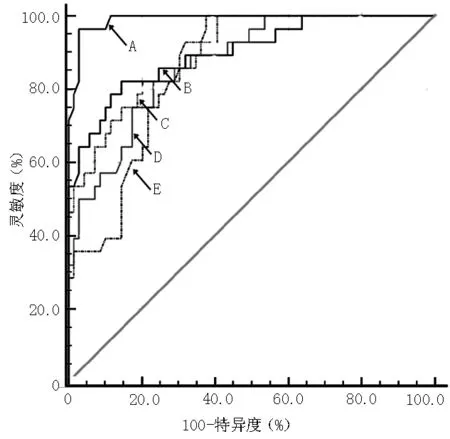
注:A=血清PCT、sTREM-1、Presepsin水平联合,B=APACHE Ⅱ评分,C=血清sTREM-1水平,D=血清PCT水平,E=血清Presepsin水平
图4 APACHE Ⅱ评分,血清PCT、sTREM-1、Presepsin水平及后3个指标联合预测脓毒症患者28 d病死率的ROC曲线
Figure4 ROC curve for evaluating the prognosis of patients with sepsis by APACHE Ⅱ score,serum levels of PCT,sTREM-1 and Presepsin alone,serum levels of PCT,sTREM-1 and Presepsin jointly
APACHE Ⅱ评分预测脓毒症患者28 d病死率的AUC大于血清PCT、Presepsin水平预测脓毒症患者28 d病死率的AUC,差异有统计学意义(Z=2.491,P=0.013;Z=4.385,P<0.001);APACHE Ⅱ评分预测脓毒症患者28 d病死率的AUC与血清sTREM-1水平预测脓毒症患者28 d病死率的AUC比较,差异无统计学意义(Z=0.786,P=0.432);血清sTREM-1水平预测脓毒症患者28 d病死率的AUC大于血清PCT、Presepsin水平预测脓毒症患者28 d病死率的AUC,差异有统计学意义(Z=3.322,P<0.001;Z=2.822,P=0.005);血清PCT水平预测脓毒症患者28 d病死率的AUC与血清Presepsin水平预测脓毒症患者28 d病死率的AUC比较,差异无统计学意义(Z=1.881,P=0.059)。
血清PCT、sTREM-1、Presepsin水平联合预测脓毒症患者28 d病死率的AUC大于APACHE Ⅱ评分,血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的AUC,差异有统计学意义(Z=6.285,P<0.001;Z=7.071,P<0.001;Z=7.071,P<0.001;Z=12.279,P<0.001)。
3 讨论
脓毒症是ICU常见的重症,全球病死率为30%~70%,临床管理极具挑战性[11]。目前大多数脓毒症相关研究均在医院ICU开展,而院外患者或者并未入住ICU及感染科患者的脓毒症患病率并不低[12],所以收集ICU、感染科脓毒症患者的炎性指标并用其判断患者预后具有一定意义。各种慢性病如COPD、慢性肾脏病、慢性肝病、癌症、糖尿病等均是脓毒症的危险因素,且慢性病的发生与地区经济状况相关[13]。同时合并慢性病患者对脓毒症的应答不尽相同,并不是所用患者会出现明显的感染症状和体征。因此,及时诊断、准确评估脓毒症患者的病情势在必行。目前国内外学者也一直在寻找早期反应迅速、特异性强的指标评估病情及预后,本研究探讨血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的价值,以期为临床医师提供参考。
PCT是降钙素的无激素活性的前肽类物质,机体正常情况下极少释放PCT入血液循环。许多研究已证实PCT在浓毒症诊断和患者预后评估中的价值[14]。RYU等[14]比较了CRP和PCT预测严重脓毒症患者预后的价值,发现CRP的预测价值并不劣于PCT。此外,JAIN等[15]对54例脓毒症患者进行研究,发现其全因死亡率为42.6%,死亡组PCT水平高于存活组。SHEHABI等[16]发现,严重感染患者血清PCT水平在患病后前72 h内如果呈连续性下降趋势,表明预后良好。同样,PODDAR等[17]选取了187例脓毒症患者并随访28 d,发现前4 d内PCT水平下降70%,提示患者预后良好。国内LIU等[18]研究发现,血清PCT能有效预测脓毒症患者的全因死亡率,但仍需要更多研究确定其临界值。本研究结果显示,死亡组血清PCT水平高于生存组,血清PCT水平与APACHE Ⅱ评分呈正相关,血清PCT水平是脓毒症患者28 d病死率的影响因素,提示PCT水平与脓毒症患者的危重程度相关。血清PCT水平预测脓毒症患者28 d病死率的AUC为0.87〔95%CI(0.78,0.93)〕,表明血清PCT在脓毒症患者预后评估中具有良好的应用价值。
髓样细胞触发受体于2000年由BOUCHON等[19]首次鉴定出来,在许多感染性疾病中均可发现其亚型sTREM-1。sTREM-1在感染过程中特异地释放于血液或体液,选择性地表达于中性粒细胞、成熟单核-巨噬细胞等细胞表面,在炎性反应中发挥主导作用。此外,其还被发现具有抗炎作用,但是具体机制仍不清楚[20-22]。TRANC等[23]的一项前瞻性研究发现,sTREM-1对脓毒症患者的预后具有预测价值。PONTRELLI等[24]发现,sTREM-1在早期诊断儿童脓毒症中具有良好的应用价值。SU等[25]对sTREM-1进行了Meta分析,证实了因严重感染死亡的患者血清sTREM-1水平高于生存患者,sTREM-1在预测患者病死率方面具有一定价值。BRENNER等[26]研究认为,sTREM-1早期诊断脓毒症的价值优于CRP和PCT,并且还发现其在预测脓毒症患者病死率方面也有一定价值。但是,sTREM-1在脓毒症中发挥保护作用的具体通路还有待进一步研究,仍需更多的研究为sTREM-1在脓毒症的诊断和治疗中的作用提供依据。本研究结果显示,死亡组血清sTREM-1水平高于生存组,血清sTREM-1水平与APACHE Ⅱ评分呈正相关,血清sTREM-1水平是脓毒症患者28 d病死率的影响因素,血清sTREM-1水平预测脓毒症患者28 d病死率的AUC为0.90〔95%CI(0.82,0.95)〕,提示血清sTREM-1在预测脓毒症患者预后评估中有不错的应用价值。
CD14是脂多糖-脂多糖结合蛋白(LPS-LBP)复合物的受体,有膜结合性CD14和可溶性CD14两种形态,其中可溶性CD14亚型(sCD14-ST)又称Presepsin。近年来,ENDO等[27]发现,相比于PCT、CRP和白介素6(IL-6)等标志物,Presepsin在诊断脓毒症中显示出更佳的灵敏度和特异度。ZHANG等[28]对Presepsin在脓毒症中的诊断价值做了系统性回顾,结果证实了其诊断脓毒症的有效性,遗憾的是,其特异度不高。此外,也有相关的Meta分析结果表明,Presepsin是诊断脓毒症的可靠性指标[29]。KLOUCHE等[30]发现,Presepsin在诊断脓毒症和评估脓毒症休克方面均有一定价值,且Presepsin联合PCT预测脓毒症患者死亡风险的特异度更高。Presepsin鉴别脓毒症和SIRS的截断值为581 ng/L,AUC为0.83,灵敏度和特异度分别为65%和100%,并且Presepsin联合急诊脓毒症死亡风险(MEDS)评分鉴别脓毒症和SIRS的AUC提高到了0.95[31]。GODNIC等[32]比较了Presepsin、CRP、PCT、CD64诊断脓毒症的价值,发现Presepsin诊断脓毒症的截断值为413 μg/L,Presepsin、PCT能鉴别脓毒症和脓毒症休克而其他两者不能,并发现Presepsin水平与APACHE Ⅱ评分呈正相关,Presepsin能有效指导临床抗生素的应用。本研究结果显示,死亡组Presepsin水平高于生存组,血清Presepsin水平与APACHE Ⅱ评分呈正相关,血清Presepsin水平是脓毒症患者28 d病死率的影响因素,血清Presepsin水平预测脓毒症患者28 d病死率的AUC为0.85〔95%CI(0.77,0.92)〕,表明血清Presepsin在脓毒症患者预后评估中具有良好的应用价值。
由于脓毒症患者病因的多样性以及感染程度的不同,目前研究均表明多个指标联合较单一指标可以更准确地诊断脓毒症和评估患者预后。因此,本研究采用多因素Logistic回归分析计算血清PCT、sTREM-1、Presepsin水平联合的Logistic回归方程,结果显示,Y=-1.218 9+0.032 96×PCT+0.061 25×sTREM-1+0.196 8×Presepsin,其预测脓毒症患者28 d病死率的AUC为0.99〔95%CI(0.94,1.00)〕,血清PCT、sTREM-1、Presepsin水平联合预测脓毒症患者28 d病死率的AUC大于APACHE Ⅱ评分和血清PCT、sTREM-1、Presepsin水平预测脓毒症患者28 d病死率的AUC,说明血清PCT、sTREM-1、Presepsin水平联合预测脓毒症患者28 d病死率的价值最高,故可以考虑使用联合指标进行患者预后的预测。
综上所述,血清PCT、sTREM-1、Presepsin水平联合检测可以提高对脓毒症患者预后评估的灵敏度和特异度,是一种有效的血清标志物,能提高脓毒症患者预后评估的准确率。本研究样本量偏小,仅探讨了近期预后,未能分析血清PCT、sTREM-1、Presepsin水平与患者远期预后的关系,因此可以在扩大样本量的基础上做进一步研究。
作者贡献:毛云进行试验设计与实施、资料收集整理、撰写论文并对文章负责;盛孝燕进行试验评估和质量控制;朱红阳进行质量控制;景道远进行试验实施、资料收集。
本文无利益冲突。
[1]WIERSINGA W J,LEOPOLD S J,CRANENDONK D R.et al.Host innate inmmune responses to sepsis [J].Virulence,2014,5(1):36-44.DOI:10.4161/viru.25436.
[2]KIBE S,ADAMS K,BARLOW G.Diagnostic and prognostic biomarkers of sepsis in critical care[J].J Antimicrob Chemother,2011,66 Suppl 2:ii33-40.DOI:10.1093/jac/dkq523.
[3]BLOOS F,REINHART K.Rapid diagnosis of sepsis[J].Virulence,2014,5(1):154-160.DOI:10.4161/viru.27393.
[4]GUPTA S,MISHRA M.Acute physiology and chronic health evaluation Ⅱ score of ≥15:a risk factor for sepsis-induced critical illness polyneuropathy[J].Neurol India,2016,64(4):640-645.DOI:10.4103/0028-3886.185356.
[5]CARBONELL N,BLASCO M,FERRERES J,et al.Sepsis and SOFA score:related outcome for critically ill renal patients[J].Clin Nephrol,2004,62(3):185-192.
[6]BRIEGEL J,MÖHNLE P,Surviving Sepsis Campaign.International guidelines of the Surviving Sepsis Campaign:update 2012[J].Anaesthesist,2013,62(4):304-309.DOI:10.1007/s00101-013-2158-x.
[7]HENRIQUEZ-CAMACHO C,LOSA J.Biomarkers for sepsis[J].Biomed Res Int,2014,2014:547818.DOI:10.1155/2014/547818.
[8]PRUCHA M,BELLINGAN G,ZAZULA R.Sepsis biomarkers[J].Clin Chim Acta,2014,440:97-103.DOI:10.1016/j.cca.2014.11.012.
[9]LEVY M M,FINK M P,MARSHALL J C,et al.2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference[J].Intensive Care Med,2003,29(4):530-538.DOI:10.1007/s00134-003-1662-x.
[10]DELLINGER R P,LEVY M M,RHODES A,et al.Surviving sepsis campaign:international guidelines for management of sever sepsis and septic shock,2012[J].Intensive Care Med,2013,39(2):165-228.DOI:10.1007/s00134-012-2769-8.
[11]PALMIERE C,AUGSBURGER M.Copeptin as a diagnostic biomarker for sepsis-related deaths[J].Peptides,2014,59:75-78.DOI:10.1016/j.peptides.2014.07.011.
[12]MENDU M L,ZAGER S,GIBBONS F K,et al.Relationship between neighborhood poverty rate and bloodstream infections in the critically ill[J].Crit Care Med,2012,40(5):1427-1436.DOI:10.1097/CCM.0b013e318241e51e.
[13]HICKS C W,ENGINEER R S,BENOIT J L,et al.Procalcitonin as a biomarker for early sepsis in the emergency department[J].Eur J Emerg Med,2014,21(2):112-117.DOI:10.1097/MEJ.0b013e328361fee2.
[14]RYU J A,YANG J H,LEE D,et al.Clinical usefulness of procalcitonin and C-reactive protein as outcome predictors in critically ill patients with severe sepsis and septic shock[J].PLoS One,2015,10(9):e0138150.DOI:10.1371/journal.pone.0138150.
[15]JAIN S,SINHA S,SHARMA S K,et al.Pocarlcitonin as a prognostic marker for sepsis:a prospective observational study[J].BMC Res Notes,2014,7:458.DOI:10.1186/1756-0500-7-458.
[16]SHEHABI Y,STERBA M,GARRETT P M,et al.Procalcitonin algorithm in critically ill adults with undifferentiated infection or suspected sepsis.A randomized controlled trial[J].Am J Respir Crit Care Med,2014,190(10):1102-1110.DOI:10.1164/rccm.201408-1483OC.
[17]PODDAR B,GURJAR M,SINGH S,et al.Procalcitonin kinetics as a prognostic marker in severe sepsis/septic shock[J].Indian J Crit Care Med,2015,19(3):140-146.DOI:10.4103/0972-5229.152755.
[18]LIU D,SU L,HAN G,et al.Prognostic value of procalcitonin in adult patients with sepsis:a systematic review and meta-analysis[J].PLoS One,2015,10(6):e0129450.DOI:10.1371/journal.pone.0129450.
[19]BOUCHON A,DIETRICH J,COLONNA M.Cutting edge:inflammatory responses can be triggered by TREM-1,a novel receptor expressed on neutrophils and monocytes[J].J Immunol,2000,164(10):4991-4995.
[20]PHUA J,KOAY E S,ZHANG D,et al.How well do serum sTREM-1 measurements prognosticate in septic shock?[J].Anaesth Intensive Care,2008,36(5):654-658.
[21]HUANG W P,JIANG W Q,HU B,et al.Significance of serum procalcitonin levels in the evaluation of severity and prognosis of patients with systemic inflammatory response syndrome[J].Zhongguo Wei Zhong Bing Ji Jiu Yi Xue,2012,24(5):294-297.
[22]DETERMANN R M,WEISFELT M,DE GANS J,et al.Soluble triggering receptor expressed on myeloid cells 1:a biomarker for bacterial meningitis[J].Intensive Care Med,2006,32(8):1243-1247.DOI:10.1007/s00134-006-0240-4.
[24]PONTRELLI G,DE CRESCENZO F,BUZZETTI R,et al.Diagnostic value of soluble triggering receptor expressed on myeloid cells in paediatric sepsis:a systematic review[J].Ital J Pediatr,2016,42:44.DOI:10.1186/s13052-016-0242-y.
[25]SU L,LIU D,CHAI W,et al.Role of sTREM-1 in predicting mortality of infection:a systematic review and meta-analysis[J].BMJ Open,2016,6(5):e010314.DOI:10.1136/bmjopen-2015-010314.
[26]BRENNER T,UHLE F,FLEMING T,et al.Soluble TREM-1 as a diagnostic and prognostic biomarker in patients with septic shock:an observational clinical study[J].Biomarkers,2017,22(1):63-69.DOI:10.1080/1354750X.2016.1204005.
[27]ENDO S,SUZUKI Y,TAKAHASHI G,et al.Usefulness of Presepsin in the diagnosis of sepsis in a multicenter prospective study[J].J Infect Chemother,2012,18(6):891-897.DOI:10.1007/s10156-012-0435-2.
[28]ZHANG J,HU Z D,SONG J,et al.Diagnostic value of presepsin for sepsis:a systematic review and meta-analysis[J].Medicine(Baltimore),2015,94(47):e2158.DOI:10.1097/MD.0000000000002158.
[29]ZHANG X,LIU D,LIU Y N,et al.The accuracy of presepsin(sCD14-ST) for the diagnosis of sepsis in adults:a meta-analysis[J].Crit Care,2015,19:323.DOI:10.1186/s13054-015-1032-4.
[30]KLOUCHE K,CRISTOL J P,DEVIN J,et al.Diagnostic and prognostic value of soluble CD14 subtype(Presepsin) for sepsis and community-acquired pneumonia in ICU patients[J].Ann Intensive Care,2016,6(1):59.DOI:10.1186/s13613-016-0160-6.
[31]CARPIO R,ZAPATA J,SPANUTH E,et al.Utility of presepsin(sCD14-ST) as a diagnostic and prognostic marker of sepsis in the emergency department[J].Clin Chim Acta,2015,450:169-175.DOI:10.1016/j.cca.2015.08.013.
[32]GODNIC M,STUBLJAR D,SKVARC M,et al.Diagnostic and prognostic value of sCD14-ST——presepsin for patients admitted to hospital intensive care unit(ICU)[J].Wiener Klin Wochenschr,2015,127(13/14):521-527.DOI:10.1007/s00508-015-0719-5.
PredictiveValueofSerumPCT,sTREM-1andPresepsinLevelsfor28-dayMortalityamongPatientswithSepsis
MAOYun,SHENGXiao-yan*,ZHUHong-yang,JINGDao-yuan
DepartmentofEICU,CentralHospitalofJinhua,Jinhua321000,China
*Correspondingauthor:SHENGXiao-yan,Associatechiefphysician;E-mail:shengxiaoyanzxyy@163.com
ObjectiveTo investigate the predictive value of serum procalcitonin(PCT) combined with soluble triggering receptor expressed on myeloid cells-1(sTREM-1) and soluble CD14subtype(Presepsin) levels for 28-day mortality among patients with sepsis.MethodsA total of 97 patients with sepsis receiving inpatient treatment in Department of EICU or Department of Infectious Diseases,Central Hospital of Jinhua from July 2014 to April 2016 were enrolled.Demographic data of the patients were collected.The serum levels of CRP,PTC,sTREM-1 and Presepsin were measured on the first day after admission.All of them were followed up for 28 days for investigating the survival status.Pearson correlation analysis was conducted to analyze the correlation of serum levels of PCT,sTREM-1 and Presepsin with APACHEⅡ.The influencing factors of 28-d mortality in sepsis patients were explored and the Logistic regression equation of serum levels of PCT,sTREM-1 and Presepsin were calculated by multivariate Logistic regression analysis.The receiver operating characteristic(ROC) curves for evaluating prognosis of patients with sepsis by APACHE Ⅱ score,serum levels of PCT,sTREM-1 and Presepsin alone,serum levels of PCT,sTREM-1 and Presepsin jointly were drawn.ResultsAccording to the follow-up results,the patients were divided into death group〔28 cases(28.9%)〕 and survival group(69 cases).The APACHE Ⅱ score,serum levels of CRP,PCT,sTREM-1 and Presepsin of death group were higher than those of survival group(P<0.05).Serum levels of PCT,sTREM-1,Presepsin were positively correlated with APACHE Ⅱ score(P<0.05).Multivariate Logistic regression analysis showed that APACHE Ⅱ score〔OR=1.13,95%CI(1.01,1.64)〕 and serum levels of PCT〔OR=1.66,95%CI(1.14,2.53)〕,sTREM-1〔OR=2.54,95%CI(1.14,5.83)〕,Presepsin〔OR=25.11,95%CI(1.58,79.7)〕 were the influencing factors of 28-d mortality in sepsis patients(P<0.05).The area under the ROC curve(AUC) of 28-d mortality in sepsis patients predicted by APACHE Ⅱ score,serum levels of PCT,sTREM-1 and Presepsin was 0.90〔95%CI(0.82,0.95)〕,0.87〔95%CI(0.78,0.93)〕,0.90〔95%CI(0.82,0.95)〕 and 0.85〔95%CI(0.77,0.92)〕,respectively.The Logistic regression equation of serum levels of PCT,sTREM-1 and Presepsin was Y=-1.218 9+0.032 96×PCT+0.061 25×sTREM-1+0.196 8×Presepsin,and the AUC of 28-d mortality in sepsis patients predicted by it was 0.99〔95%CI(0.94,1.00)〕.The AUC of 28-d mortality in sepsis patients predicted by serum levels of PCT,sTREM-1 and Presepsin jointly was greater than that predicted by APACHE Ⅱ score,serum levels of PCT,sTREM-1 and Presepsin alone(P<0.05).ConclusionThe value of serum levels of PCT,sTREM-1 and Presepsin in predicting the 28-d mortality in sepsis patients is better than that of single index,which has important reference value and clinical significance,and is helpful for clinical decision-making.
Sepsis;Mortality;Forecasting;Procalcitonin;Soluble triggering receptor expressed on myeloid cells-1;Soluble CD14subtype
321000 浙江省金华市中心医院急诊重症监护室
*通信作者:盛孝燕,副主任医师;E-mail:shengxiaoyanzxyy@163.com
R 631
A
10.3969/j.issn.1007-9572.2017.00.177
毛云,盛孝燕,朱红阳,等.血清降钙素原和可溶性髓样细胞触发受体-1及可溶性CD14亚型水平联合预测脓毒症患者28 d病死率的价值研究[J].中国全科医学,2017,20(36):4494-4500.[www.chinagp.net]
MAO Y,SHENG X Y,ZHU H Y,et al.Predictive value of serum PCT,sTREM-1 and Presepsin levels for 28-day mortality among patients with sepsis[J].Chinese General Practice,2017,20(36):4494-4500.
2017-07-13;
2017-10-24)
崔丽红)

