甲状腺、垂体激素在中重型颅脑损伤患者中的检测意义
张 明,魏剑波
(四川省攀枝花市中心医院,攀枝花 617067)
甲状腺、垂体激素在中重型颅脑损伤患者中的检测意义
张 明,魏剑波
(四川省攀枝花市中心医院,攀枝花 617067)
目的:探析甲状腺激素(TH)及垂体激素水平变化在中型颅脑损伤(MHI)、重型颅脑损伤(SHI)患者病情判断及预后情况观察中的临床价值。方法:分析2010年1月~2015年12月在我院接受诊治的50例HI患者的临床资料。根据颅脑损伤(HI)病情严重程度将入选者分成MHI组(22例)和SHI组(28例)。根据预后情况将入选者分成存活组(S组,40例)和死亡组(D组,10例)。另外选取同期在我院接受健康体检的45例健康者作为本次研究的对照组。比较MHI组、SHI组、对照组及S组和D组患者的TH(总三碘甲腺原氨酸TT3、总甲状腺素TT4、游离三碘甲腺原氨酸FT3和游离甲状腺素FT4)、促甲状腺激素(TSH)、血清泌乳素(PRL)及促卵泡生成素(FSH)等指标的表达水平。结果:MHI组、SHI组与对照组的一般资料无显著差异。MHI组患者的TT3、FT3明显较SHI组患者高,PRL及FSH明显较SHI组低,而TT4、FT4及TSH水平无显著差异。MHI组、SHI组患者的TT3、FT3明显较对照组低,PRL及FSH明显较对照组高,而TT4、FT4及TSH水平无显著差异。S组患者的TT3、FT3、PRL及FSH水平明显优于D组,而TT4、FT4及TSH水平无显著差异。结论:HI患者的预后情况随着其病情的加重而变差,且血清TT3、FT3、PRL及FSH可作为HI患者病情判断及其预后观察的重要指标。
颅脑损伤;甲状腺激素;垂体激素;预后
临床上,下丘脑-垂体系统作用主要是对人体的代谢和内分泌功能进行有效调控,从而影响人体的多系统及多脏器功能,是完整的神经内分泌中枢系统之一。据报道,颅脑损伤(HI)会使下丘脑-垂体-甲状腺轴系统功能在一定程度上出现异常现象[1,2]。相关研究资料结果证实,HI会扰乱患者的神经内分泌功能,致使患者的代谢功能发生异常,最终引发神经源性多脏器受障[3]。目前有学者发现,重型颅脑损伤(SHI)者的病情越严重,其体内血清胃泌素及血糖水平则越高,且高浓度的胃泌素及血糖反之也会对患者的病情及其预后产生影响[4,5]。本研究旨在通过对中型颅脑损伤(MHI)、SHI者的甲状腺激素(TH)及垂体激素浓度的变化与其预后情况的相关性的研究,以期为临床判断HI患者病情及其预后观察提供一定的理论参考依据。
1 资料与方法
1.1 研究对象
分析2010年1月~2015年12月在我院接受诊治的50例HI患者的临床资料。其中男40例,女10例,平均年龄(37.5±4.1)岁。根据格拉斯哥(GCS)计分情况对患者的病情给予准确判断:MHI者(9~12分)22例,SHI者(3~8分)28例。另外选取同期在我院接受健康体检的45例健康者作为本次研究的对照组。根据HI病情严重程度将入选者分成MHI组(22例)和SHI组(28例)。MHI组、SHI组及对照组的一般资料无显著差异(P>0.05),详见表1。根据预后情况将入选者分成存活组(S组,40例)和死亡组(D组,10例)。

表1 MHI组和SHI组患者的一般资料比较
1.2 研究方法
血样的采集:采集受试者入院2h内 8mL静脉血,将血清分离并冷冻保存在-45℃的冰箱内待测。采用由芬兰Wallac Oy公司生产的仪器与试剂,以时间分辨荧光免疫法进行检测,重复2次检测每份血清标本并计算其平均值。
观察指标:所有入选者的TH(总三碘甲腺原氨酸TT3、总甲状腺素TT4、游离三碘甲腺原氨酸FT3和游离甲状腺素FT4)、促甲状腺激素(TSH)、血清泌乳素(PRL)及促卵泡生成素(FSH)等指标的表达水平。
1.3 统计学方法
本研究中的数据均采用SPSS19.0软件进行分析。数据计量以均数±标准差形式表示,比较采用t检验和卡方(χ2)检验。我们定义P<0.05为差异具有统计学意义。
2 结果
2.1 MHI组和SHI组的各项指标水平
表2结果提示MHI组患者的TT3、FT3明显较SHI组患者高,PRL及FSH明显较SHI组低(P<0.05),而TT4、FT4及TSH水平无显著差异(P>0.05)。MHI组、SHI组患者的TT3、FT3明显较对照组低,PRL及FSH明显较对照组高(P<0.05),而TT4、FT4及TSH水平无显著差异(P>0.05)。
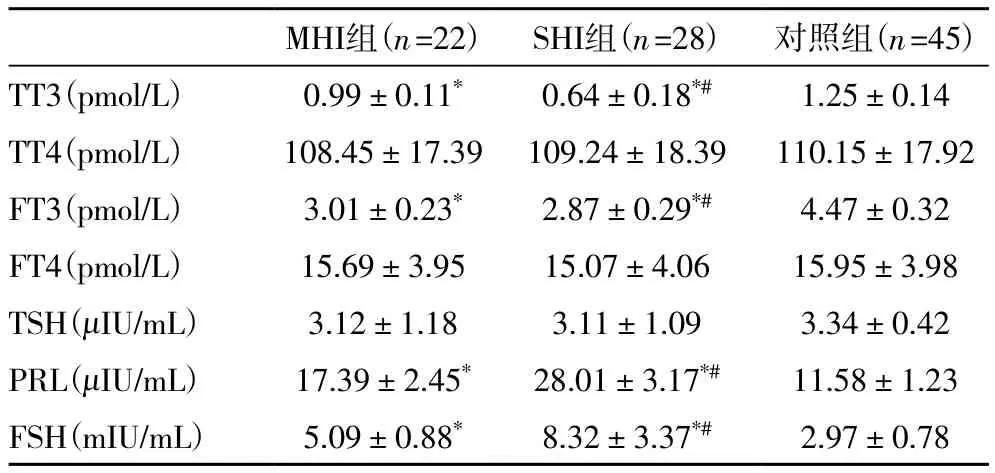
表2 MHI组和SHI组各项指标的水平比较
2.2 S组和D组患者的各项指标水平
表3结果提示S组患者的TT3、FT3、PRL及FSH明显较D组患者优秀(P<0.01),而TT4、FT4及TSH水平无显著差异(P>0.05)。

表3 S组和D组患者各项指标的水平比较
3 讨论
目前,我国创伤性颅脑损伤(TBI)发病率呈逐年上升趋势,致残率、致死率均较高,其中中、重型颅脑损伤(MHI、SHI)患者居多。而甲状腺与垂体激素出现异常变化是TBI的常见并发症,发病率较高,其中垂体激素变化异常的主要发病机制是TBI后出现的垂体功能低下并发症所致,其不仅会导致患者内分泌紊乱,还会引发抑郁、认知受损等神经症状,此症状又极易与颅脑损伤的后遗症混淆,故常常会导致误诊或漏诊。
临床上,急性颅脑损伤(HI)者体内血清总三碘甲腺原氨酸(TT3)及游离三碘甲腺原氨酸(FT3)水平显著下降,而血清泌乳素(PRL)及促卵泡生成素(FSH)水平却显著增加,即FT3及FSH等水平的检测对HI患者病情的判断及其预后的评估、疗效的评估等均具有极其重要的临床意义[6]。本研究结果显示,中型颅脑损伤(MHI)者的血清TT3、FT3浓度均显著高于重型颅脑损伤(SHI)者,血清PRL、FSH水平则显著低于SHI者,且MHI组、SHI组患者的TT3、FT3明显较对照组低,PRL及FSH明显较对照组高,提示HI患者激素水平明显发生了变化,且HI病情程度越重,这种变化越显著。
HI往往会引发下丘脑与垂体的直接(或间接)受损:直接暴力致使颅腔内脑组织剧烈运动,导致神经垂体、垂体柄及腺垂体受损,严重时会引发垂体前叶及下丘脑梗死,对垂体功能造成不良影响;外伤导致颅内压陡然上升等引发下丘脑、垂体直接遭受压力,从而导致垂体激素分泌受到很大地影响;外伤导致细胞本身与垂体柄受损,内分泌功能失调或坏死[7],HI患者体内血清FSH和PRL浓度大幅增加[8]。患者下丘脑受损,垂体前叶对促甲状腺激素(TSH)的分泌功能会受到影响,TSH释放激素的分泌量大幅下降,同时还会影响甲状腺激素(TH)的分泌,导致三碘甲腺原氨酸(T3)、甲状腺素(T4)水平降低[9]。患者的颅内压由于HI的影响而显著上升,脑部呈缺血缺氧状,5’-脱碘酶(5’-D)和神经细胞酶活性减弱,合成还原型辅酶II(NADPH)和谷胱甘肽(GSH)的能力降低且数量减少,T4转化为T3的数目亦减少,同时组织自身所摄取的T4数量也不断降低,最终导致活性T3的产生量大幅下降[10,11]。
目前学者们国内外对HI患者体内血清TT4水平的变化趋势观点不一[12]。有些学者发现HI患者的病情程度越严重,血清TT4水平会越低,但无统计学差异[13];还有学者认为HI患者病情程度越高,血清TT4水平也明显增加,且差异显著[14]。本研究结果显示,HI患者的病情加重时,尽管血清TT4水平确实稍有增加,但两者间无显著差异,即SHI患者的血清TT4水平略高于MHI患者,提示患者体内T4分泌量虽然有所下降,但T4转化成T3的量也在减少,故患者体内的血清T4水平未发现显著改变。
总之,垂体激素及TH水平的变化可以作为HI患者病情判断及预后情况观察的重要指标,其均与HI患者病情关系密切,临床上值得大力推广。
[1] Miljic D, Miljic P, Doknic M, et al. Adipsic diabetes insipidus and venous thromboembolism (VTE): recommendations for addressing its hypercoagulability[J]. Hormones (Athens), 2014, 13(3): 420-3.
[2] 彭东海. 早期机械通气在重型颅脑损伤中的临床应用价值[J]. 湖南师范大学学报 (医学版), 2008, 5(4): 40-43.
[3] Wiechecka J, Krzewska A, Droń I, et al. Panhypopituitarism after multisystem trauma[J]. Pediatr Endocrinol Diabetes Metab, 2013, 20(1):27-9.
[4] Ciancia S. Pituitary insufficiency after traumatic brain injury: consequences? Screening? [J]. Ann Fr Anesth Reanim, 2012, 31(6): e117-24.
[5] 郑超, 乔陈财, 唐红军, 等. 重型颅脑损伤患者血清 NSE 和 MMPs的动态变化及临床意义[J]. 湖南师范大学学报 (医学版), 2016, 13(4): 107-109, 110.
[6] Widmayer MA, Browning JL, Gopinath SP, et al. Increased intracranial pressure is associated with elevated cerebrospinal fluid ADH levels in closed-head injury[J]. Neurol Res, 2010, 32(10): 1021-6.
[7] Nemes O, Kovacs N, Czeiter E, et al. Predictors of post-traumatic pituitary failure during long-term follow-up[J]. Hormones (Athens), 2015, 14(3): 383-91.
[8] Brod M, Pohlman B, Højbjerre L, et al. Impact of adult growth hormone deficiency on daily functioning and well-being[J]. BMC Res Notes, 2014, 7: 813.
[9] KhKh S, Savin IA, Tenedieva VD, et al. [Analysis of thyroid homeostasis disorders in patients with severe traumatic brain injury][J]. Zh Vopr Neirokhir Im N N Burdenko, 2012, 76(4): 26-30; discussion 30-1.
[10] Tritos NA, Byrne TN, Wu CL, et al. A patient with diabetes insipidus, anterior hypopituitarism and pituitary stalk thickening[J]. Nat Rev Endocrinol, 2011, 7(1): 54-9.
[11] Malekpour B, Mehrafshan A, Saki F, et al. Effect of posttraumatic serum thyroid hormone levels on severity and mortality of patients with severe traumatic brain injury[J]. Acta Med Iran, 2012, 50(2): 113-6.
[12] Karaca Z, Tanrıverdi F, Ünlühızarcı K, et al. GH and Pituitary Hormone Alterations After Traumatic Brain Injury[J]. Prog Mol Biol Transl Sci, 2016, 138: 167-91.
[13] Melmed S. Idiopathic adult growth hormone deficiency[J]. J Clin Endocrinol Metab, 2013, 98(6): 2187-97.
[14] Villasana LE, Westbrook GL, Schnell E. Neurologic impairment following closed head injury predicts post-traumatic neurogenesis[J]. Exp Neurol, 2014, 261: 156-62.
The detective value of TH and pituitary hormones in patients with MHI and SHI
Zhang Ming, Wei Jian-bo
(The Central Hospital of Panzhihua City, Panzhihua 617067, China)
ObjectiveOur retrospective study was aimed to analyze the clinical value of the changes of the levels of TH and pituitary hormones in the illness evaluation and prognosis observation of MHI, SHI patients.MethodsClinical data of 50 patients with HI
treatment at our hospital from January, 2010 to December, 2015 was retrospectively analyzed. Patients included were divided into two groups according to the severity of HI patients, MHI group (22 cases) and SHI group (28 cases). Patients included were divided into two groups according to the prognosis of HI patients, survival group (S group, 40 cases) and death group (D group, 10 cases).45 healthy persons checked at the same time at our hospital were chosen as the control group. The levels of TH (TT3, FT3, TT4, FT4), TSH, PRL, FSH of patients on MHI group, SHI group and control group, S group and D group were respectively compared.ResultsThe general information in MHI group, SHI group and control group had no statistical difference. The levels of TT3, FT3 in MHI group were obviously higher than those in SHI group, and the levels of PRL and FSH in MHI group were obviously lower than those in SHI group, but the levels of TT4, FT4, TSH in MHI group and SHI group had no statistical difference. The levels of TT3, FT3 in MHI group, SHI group were obviously lower than those in control group, and the levels of PRL and FSH in MHI group, SHI group were obviously higher than those in control group, but the levels of TT4, FT4, TSH in MHI group, SHI group and control group had no statistical difference. The levels of TT3, FT3, PRL and FSH in S group were obviously better than those in D group, but the levels of TT4, FT4, TSH in S group and D group had no statistical difference.ConclusionThe prognosis of HI patients is worse as the degree of injury is more severe. The serum TT3, FT3, PRL and FSH could be regarded as the important indexes in determining the severity and prognosis of HI patients.
head injury (HI); thyroid hormone (TH); pituitary hormones; prognosis
R651.1
A
1673-016X(2017)05-0080-03
2017-04-10
张明,E-mail:714580176@qq.com