脐带过短与母儿结局的临床分析
陈溶鑫
脐带过短与母儿结局的临床分析
陈溶鑫
目的 探讨脐带过短对母儿结局的影响。方法 回顾性分析2016年1月—2017年1月在福建省妇幼保健院产科分娩的848例单胎活产孕妇临床资料,根据脐带长度分为4组: 脐带长度<第5百分位数为组1(脐带过短组);≥第5百分位数,<第10百分位数为组2;≥第10百分位数,≤第25百分位数为组3;>第25百分位数,≤第75百分位数为组4(对照组)。采取单因素方差分析、χ2检验分析脐带过短对母儿的影响。结果 女胎脐带较男胎短,早产儿脐带较足月儿短。脐带过短组妊娠期高血压疾病、胎儿生长受限、羊水过少的发生率,剖宫产率,脐带绕颈、脐带扭转发生率,NICU入住率均高于对照组。结论 脐带过短增加了剖宫产率及母儿不良结局的发生。孕晚期、产程中应加强胎心监护。
脐带过短;母儿结局;临床分析
脐带是连接胎儿与胎盘之间的纽带。脐带过短与胎儿生长受限、分娩期并发症相关,使胎儿死亡率增加2倍[1]。脐带过短在临产前常无征象,临产后由于胎先露下降时脐带牵拉过紧,使胎儿血循环受阻出现胎儿窘迫[2]。本研究回顾性分析脐带过短对母亲及围产儿结局的影响,为孕晚期和产时的母儿监测提供参考。
1 资料与方法
1.1 研究对象
2016年1月—2017年1月在福建省妇幼保健院产科产检分娩的单胎活产产妇,排除胎儿畸形、双胎或多胎妊娠者,共848例。
1.2 研究方法
本研究中脐带平均长度(61.91±13.66)cm,第5、10、25、75百分位分别为45、48、50、70 cm,根据脐带长度分为4组:<45 cm(脐带过短组),≥45、<48 cm,≥48、≤50 cm,>50、≤70 cm(对照组)。组1组34例,组2组50例,组3组137例,组4即对照组504例。比较4组的临床特征。其中脐带长度>70 cm共123例不纳入研究。
1.3 统计学处理
采用SPSS 22.0软件进行统计分析。正态分布计量资料组间比较采用单因素方差分析;定性资料组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结果
2.1 不同母儿情况的脐带长度比较
女胎脐带长度短于男胎,早产儿脐带长度短于足月儿,差异均有统计学意义(P<0.05)。初、经产妇脐带长度差异无统计学意义(P>0.05)(见表1)。
2.2 不同脐带长度妊娠合并症、并发症发生率比较
脐带过短组妊娠期高血压发生率(14.7%)、胎儿生长受限(FGR)发生率(8.8%)、羊水过少发生率(11.8%),均高于对照组(4.2%、3.3%、3.2%),差异有统计学意义(P<0.05)。4组妊娠期糖尿病、羊水过多、胎盘早剥发生率均差异无统计学意义(P>0.05)(见表2)。
2.3 不同脐带长度母儿结局的比较
脐带过短组剖宫产率(41.2%)、NICU入院率(14.7%)均高于对照组(30.0%、4.6%),脐带扭转发生率(44.1%)、脐带绕颈发生率(11.8%)均低于对照组(64.9%、23.6%),脐带过短组小于胎龄儿发生率(8.8%)高于对照组(2.8%),差异均有统计学意义(P<0.05)。4组的胎儿窘迫发生率差异无统计学意义(P>0.05)(见表3)。
3 讨论
3.1 脐带过短与母儿不良结局
本研究中脐带过短组剖宫产率高于对照组,剖宫产率随着脐带长度的减少而增加。这与之前许多研究结果一致。Yuriko Y等[3]认为脐带越短,不良妊娠结局发生率越高,剖宫产率增加。Balkawade NU等[4]认为正常脐带长度的孕妇阴道分娩率更高。脐带过短容易发生脐带过度牵拉,导致脐血管痉挛、胎盘早剥。Georgiadis L等[5]也认为脐带越短,胎盘早剥发生率越高。本研究中4组胎盘早剥发生率无差异,妊娠期高血压疾病、感染等原因都可能引起胎盘早剥。本研究中脐带过短组新生儿NICU入住率显著高于对照组,与Krakowiak P等[6]研究一致。他认为脐带过短与小于胎龄儿、胎儿低氧血症、胎儿窘迫相关。本研究还发现随着脐带长度的增长,脐带扭转及脐带绕颈的发生率增加。这可能与脐带长度增加胎儿活动范围更大有关。
3.2 脐带过短发生机制
Miller ME等[7]认为胎儿运动对脐带的适当牵拉使得脐带增长(伸展假说)。动物实验发现当孕中期胎儿运动和羊水量达整个孕期的峰值时,脐带的生长速度最快。Calvano CJ[8]等用氨酰心安、酒精、箭毒等药物减少鼠胎在宫腔内的运动,脐带生长减慢。本研究中脐带过短组羊水过少发生率显著高于对照组,说明羊水过少时胎儿运动减少,脐带生长减慢。
3.3 脐带过短母儿特征
本研究中女胎脐带短于男胎,与Georgiadis L等[5]、Krakowiak P等[6]、Yuriko Y等[3]研究一致。本研究中经产妇与初产妇的脐带长度差异无统计学意义,但Georgiadis L等[5]发现随着产次的增加,子宫增大,胎儿活动空间增大,脐带更长。本研究中早产儿的脐带比足月儿短,说明脐带的生长贯穿整个孕期。
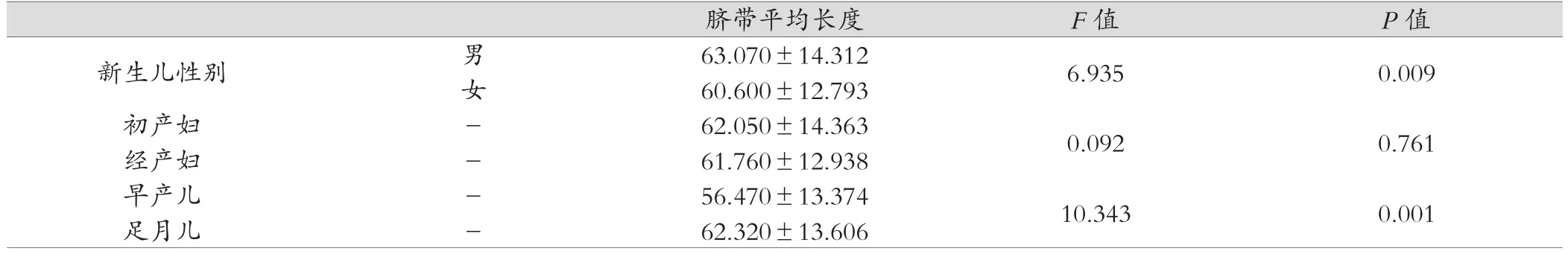
表1 不同母儿情况的脐带长度比较
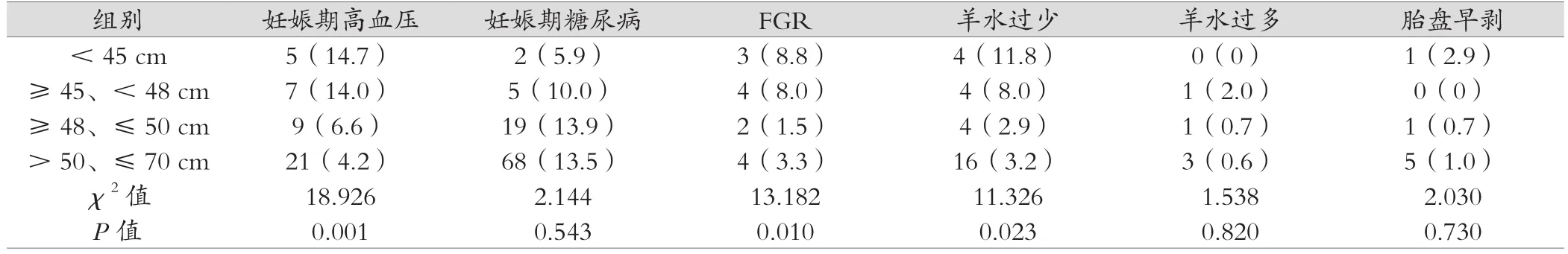
表2 不同脐带长度妊娠合并症、并发症发生率比较[例(%)]
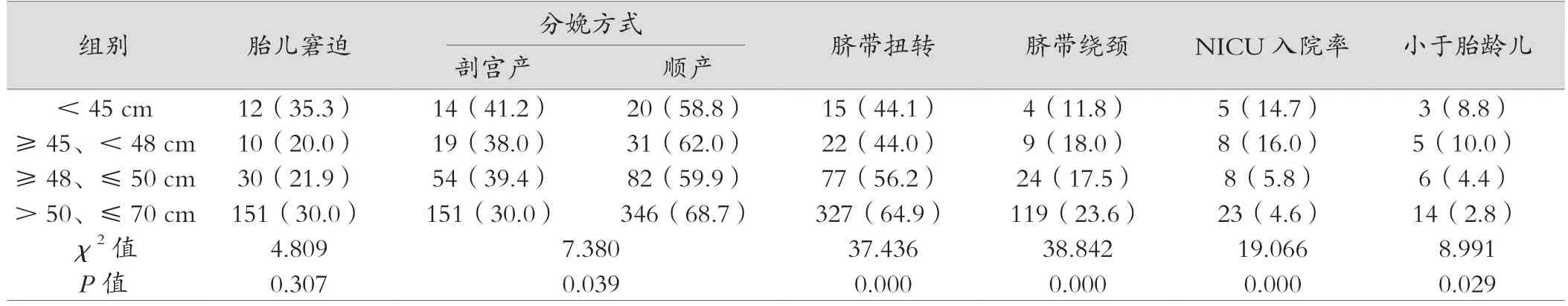
表3 不同脐带长度母儿结局比较[例(%)]
脐带过短是引起母儿不良结局的重要原因之一。胎心监护是比较方便的监测方法,故产程中应加强胎心监护,早发现早处理,减少母儿并发症的发生。
[1] F. Gary Cunningham. Williams Obstetrics[M]. 24 th edition. New York:McGraw-Hill Education,2014:121
[2] 张为远. 中华围产医学[M]. 1版.北京:人民卫生出版社,2012:477
[3] Yuriko Y,Shigeru A,Mari S,et al. Relationship between short umbilical cord length and adverse pregnancy outcomes[J]. Fetal and Pediatric Pathology,2016,35(2):81-87.
[4] Balkawade NU,Shinde MA. Study of length of umbilical cord and fetal outcome:a study of 1 000 deliveries[J]. Journal of Obstetrics and Gynecology of India,2012,62(5):520-525.
[5] Georgiadis L,Keski-Nisula L,Harju M,et al. Umbilical cord length in singleton gestations:a Finnish population-based retrospective register study[J]. Placenta ,2014,35(4):275-280.
[6] Krakowiak P, Smith EN,de Bruyn G,et al. Risk factors and outcomes associated with a short umbilical cord[J]. Obstet Gynecol,2004,103(1):119-127.
[7] Miller ME,Jones MC,Smith DW,et al. Tension:the basis of umbilical cord growth[J]. J Pediatr,1982,101(5):844.
[8] Calvano CJ,Hoar RM,Mankes RF,et al. Experimental study of umbilical cord length as a marker of fetal alcohol syndrome[J].Teratology,2000,61(3):184-188.
Relationship Between Short Umbilical Cord Length and Maternal and Perinatal Outcomes
CHEN Rongxin Department of Obstetrics, Fujian Provincial Maternity and Children Hospital, Fuzhou Fujian 350001, China
ObjectiveTo analyze how short umbilical cord length relates to maternal and perinatal outcome.Methods848 cases of single birth pregnancy in obstetrics and gynecology in Fujian Provincial Maternity and Children Hospital from January 2016 to January 2017 were analyzed,according to the length of the umbilical cord, were categorized into four groups: less than the 5thpercentile, from the 5thpercentile to less than the 10thpercentile, from the 10thpercentile to less than 25thpercentile ,and from the 25thpercentile to less than 75thpercentile, which constituted the control group. The single factor analysis of variance andχ2test were used to analyze the effect of too short umbilical cord on the mother and fetus.ResultsFemale gender, preterm delivery were associated with shorter cord lengths. The incidence of hypertensive disorders in pregnancy, fetal growth restriction, oligohydramnios, cesarean delivery, nuchal cords,torsion of cord and NICU admission were significantly higher in short cords as compared to control group.ConclusionThis study shows that shorter cord was associated with higher risk of adverse pregnancy outcomes and cesarean delivery. Additional fetal heart rate monitoring was required during the last phase of pregnancy and labor.
short umbilical cord length; maternal and perinatal outcome;analysis
R714
A
1674-9316(2017)21-0039-03
10.3969/j.issn.1674-9316.2017.21.018
福建省2014年临床重点专科(西医类别)建设项目(闽卫医政函[2015]593号)
福建省妇幼保健院产科,福建 福州 350001

