鼻咽癌T分期累及舌骨上颈部筋膜间隙规律的MRl探讨
王蔚凌,周瑶,王荣品,何玺,刘昌杰
鼻咽癌T分期累及舌骨上颈部筋膜间隙规律的MRl探讨
王蔚凌,周瑶,王荣品*,何玺,刘昌杰
作者单位:贵州省人民医院放射科,贵阳 550002
目的 应用MRI探讨鼻咽癌侵犯舌骨上颈部筋膜间隙的规律及其与肿瘤T分期的关系。材料与方法 回顾性分析2013年7月至2016年3月贵州省人民医院经病理学证实的鼻咽癌初诊患者200例,在治疗前行MRI平扫及增强检查。由2名有经验的影像诊断医师结合中国鼻咽癌临床分期工作委员会新修订形成的“鼻咽癌2008分期”,观察鼻咽癌对舌骨上颈部各筋膜间隙的侵犯情况及其与T分期的关系,进一步了解鼻咽癌的生长规律。结果 (1)鼻咽癌对舌骨上各筋膜间隙的侵犯率依次为:咽黏膜间隙(200例)、咽旁间隙(180例)、咀嚼间隙(139例)、咽后间隙(125例)、椎周间隙(119例)、颈动脉间隙(57例)、腮腺间隙(14例)、下颌下间隙(2例)、面颊间隙(1例)。(2)鼻咽癌T1期8例(4.0%)肿瘤仅局限于咽黏膜间隙; T2期34例,其中64.7% (22/34)肿瘤突破咽颅底筋膜侵犯咽旁间隙;T3期61例(30.5%)肿瘤对舌骨上各筋膜间隙的侵犯率依次为咽黏膜间隙(100%,61/61)、咽旁间隙(100%,61/61)、咽后间隙(77.0%,47/61)、咀嚼间隙(68.9%,42/61)、椎周间隙(67.2%,41/61)及颈动脉间隙(37.7%,23/61),下颌下间隙、腮腺间隙、面颊间隙及颈后间隙均未见侵犯征象;T4期97例(48.5%)肿瘤对舌骨上各筋膜间隙的侵犯率依次为咽黏膜间隙(100%,97/97)、咽旁间隙(100%,97/97)、咀嚼间隙(100%,97/97)、咽后间隙(80.4%,78/97)、椎周间隙(76.3%,74/97)、颈动脉间隙(35.1%,34/97)、腮腺间隙(14.4%,14/97)、下颌下间隙(2.1%,2/97)及面颊间隙(1.0%,1/97),颈后间隙未见受侵征象。(3)鼻咽癌向单侧及双侧侵犯率分别为30.2% (58/192)和69.8%(134/192)。结论 鼻咽癌对于周围的舌骨上筋膜间隙侵犯中,以咽旁间隙侵犯率最高。颈后间隙是唯一未受侵犯的舌骨上筋膜间隙。肿瘤向周围生长的模式为:向侧方浸润多于向后方,向后方浸润多于向侧后方,向双侧浸润明显多于向单侧浸润。
舌骨上颈部筋膜间隙;鼻咽肿瘤;磁共振成像
鼻咽癌(nasopharyngeal carcinoma)是发生在鼻咽顶后壁和侧壁黏膜的一种恶性肿瘤,是华南地区的常见恶性肿瘤之一,国内外应用MRI进行鼻咽癌及其周围组织结构侵犯的研究已有较多报道,但多局限于鼻咽癌周围个别或部分间隙的单一研究探讨,对与其密切相关的舌骨上筋膜间隙尚缺乏一个全面的叙述。笔者回顾性研究鼻咽癌初诊患者的MR图像,结合中国鼻咽癌临床分期工作委员会新修订形成的“鼻咽癌2008分期”[1],探讨鼻咽癌对舌骨上颈部各筋膜间隙的侵犯规律,并为放疗靶区的确定提供依据。
1 材料与方法
1.1 病例入选
2013年7月至2016年3月诊治于贵州省人民医院经病理学证实的鼻咽癌初诊患者200例[为了避免不同病理类型可能存在的统计学差异,故均选用非角化性(未分化)癌],男127例,女73例,年龄15~81岁,中位年龄46岁。在治疗前均行MR平扫及增强检查。已知有头颈部其他疾病者不纳入本组资料。
1.2 扫描方法
使用Siemens 3.0 T超导型MR成像仪。扫描范围轴面从颞叶至C3椎体,冠状面及矢状面从颞叶至T1椎体。MR平扫均采用轴面T1WI (TR 385 ms,TE 15 ms),轴面T2WI (TR 4532 ms,TE 100 ms),矢状面T1WI (TR 350 ms,TE 15 ms),冠状面T2WI (TR 4120 ms,TE 100 ms),层厚均为5 mm,层间距均为1 mm;轴面DWI (TR 6000 ms,TE 58 ms,层厚4 mm,层间距1 mm)。增强检查对比剂Gd-DTPA,总量0.2 mmol/kg体重,流率2.0 ml/s,使用高压注射器经肘静脉注入。行FSE序列T1WI+Fs轴面、冠状面及矢状面扫描,扫描参数为TR 460 ms,TE 15 ms,层厚5 mm,层间距1 mm。然后将采集数据传入图像后处理工作站。
1.3 舌骨上颈部筋膜间隙的解剖定义
(1)下颌下间隙(SMS):位于口底,以下颌舌骨肌为界,将口底分为内上的舌下间隙和外下的颌下间隙。(2)咽黏膜间隙(PMS):主要结构为鼻咽及口咽,值得注意的是,腭帆提肌位于咽颅底筋膜内侧,故也属于咽黏膜间隙。(3)咽后间隙(RPS):为咽缩肌与椎前肌之间的脂肪间隙,上起颅底,下达纵隔。(4)椎周间隙(PVS):椎体周围的肌群共同构成椎周间隙,上起颅底,下达纵隔。(5)颈动脉间隙(CS):颈动脉间隙又称颈动脉鞘,上达颈静脉孔,下达主动脉弓。(6)咽旁间隙(PPS):也称为茎突前间隙,严格地说,它并非由颈深筋膜围绕而成,而是位于这几层筋膜之间的脂肪充填间隙,范围自颅底延伸至舌骨。(7)腮腺间隙(PS):位于下颌骨后缘,浅层筋膜分裂包绕腮腺,形成腮腺间隙。(8)咀嚼间隙(MS):位于下颌骨下缘,其内包括下颌骨升支、翼内肌、翼外肌、咬肌和颞肌。(9)颈后间隙(PCS):由外侧包绕胸锁乳突肌的颈深筋膜浅层和内侧的椎前筋膜构成,从颅底向下延伸至锁骨。(10)面颊间隙(BS):其内界是上颌骨牙槽外缘的颊肌,后缘是咀嚼间隙[2]。
1.4 诊断标准
MR平扫T1WI呈稍低信号,T2WI呈稍高信号,增强后呈不均匀或(和)均匀强化,DWI高b值图像呈高信号且ADC图呈低信号视为肿瘤侵犯。颅底骨质在T1WI上脂肪高信号消失,增强后有明显强化为骨质侵犯的诊断标准[3]。
根据Li等[4]的标准,将鼻咽部周围舌骨上筋膜间隙鼻咽癌的侵犯率划分为高危组(≥35)、中危组(≥5~<35 )和低危组(<5) 3个等级。高危组为PPS、MS、RPS、PVS受侵;中危组为:CS、PS受侵;低危组为:SMS、BS受侵。
1.5 MR图像分析
由2名有经验的影像诊断医师结合中国鼻咽癌临床分期工作委员会新修订形成的“鼻咽癌2008分期”[1],观察鼻咽癌对舌骨上颈部各筋膜间隙的侵犯情况及其与T分期的关系。对不一致的征象与至少一名副主任医师共同讨论,并取得一致意见后确定,将仍有分歧意见的病例剔除病例观察组。
1.6 统计学处理
采用Epidate软件进行双份录入,通过统计软件SPSS 13.0对鼻咽癌各舌骨上筋膜间隙的侵犯率、与鼻咽部紧邻的三个舌骨上筋膜间隙的侵犯率、向周围间隙单侧及双侧侵犯率、T2、T3、T4期不同舌骨上筋膜间隙侵犯率相互比较,均采用卡方检验,以P<0.05为差异有统计学意义。
2 结果
2.1 舌骨上筋膜间隙的侵犯率
200例鼻咽癌各舌骨上筋膜间隙的侵犯率见表1,侵犯间隙分别为:咽黏膜间隙(PMS)、咽旁间隙(PPS)、咀嚼间隙(MS)、咽后间隙(RPS)、椎周间隙(PVS)、颈动脉间隙(CS)、腮腺间隙(PS)、下颌下间隙(SMS)、面颊间隙(BS)。其中颈后间隙(PCS)是唯一未受侵的间隙。鼻咽癌侵犯各间隙的MRI表现见图1~9。
2.2 舌骨上筋膜间隙的侵犯率对比分析
鼻咽部紧邻的三个舌骨上筋膜间隙的侵犯率进行两两对比分析,结果显示肿瘤向侧方的咽旁间隙浸润多于向后方的咽后间隙,两两比较差异具有统计学意义(表2);向后方的咽后间隙浸润多于向侧后方的颈动脉间隙,两者之间差异具有统计学意义(表3)。鼻咽癌向周围间隙单侧及双侧侵犯率进行对比分析,结果显示,鼻咽癌向双侧浸润明显多于向单侧浸润,两者之间差异具有统计学意义(表4)。

表1 200例非角化性(未分化)鼻咽癌对各舌骨上筋膜间隙的侵犯率比较Tab. 1 Comparison of the invasion rates of the 200 cases of non-keratinizing nasopharyngeal carcinoma (undifferentiated)invasion to all suprahyoid fascial spaces

表2 咽旁间隙与咽后间隙的侵犯率比较Tab. 2 Comparison of the invasion rates between the PPS and the RPS
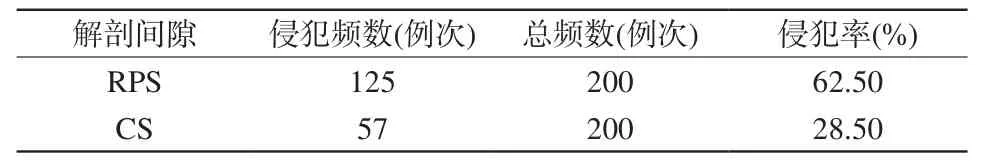
表3 咽后间隙与颈动脉间隙的侵犯率比较Tab. 3 Comparison of the invasion rates between RPS and CS

表4 鼻咽癌向周围间隙单侧及双侧侵犯率比较Tab. 4 Comparison of the invasion rates of between the unilateral and bilateral invasion of the nasopharyngeal carcinoma to the surrounding space

表5 鼻咽癌各T分期侵犯舌骨上筋膜间隙的结果(例)Tab. 5 Results of all T stages of nasopharyngeal carcinoma invasion to the suprahyoid fascial spaces (n)
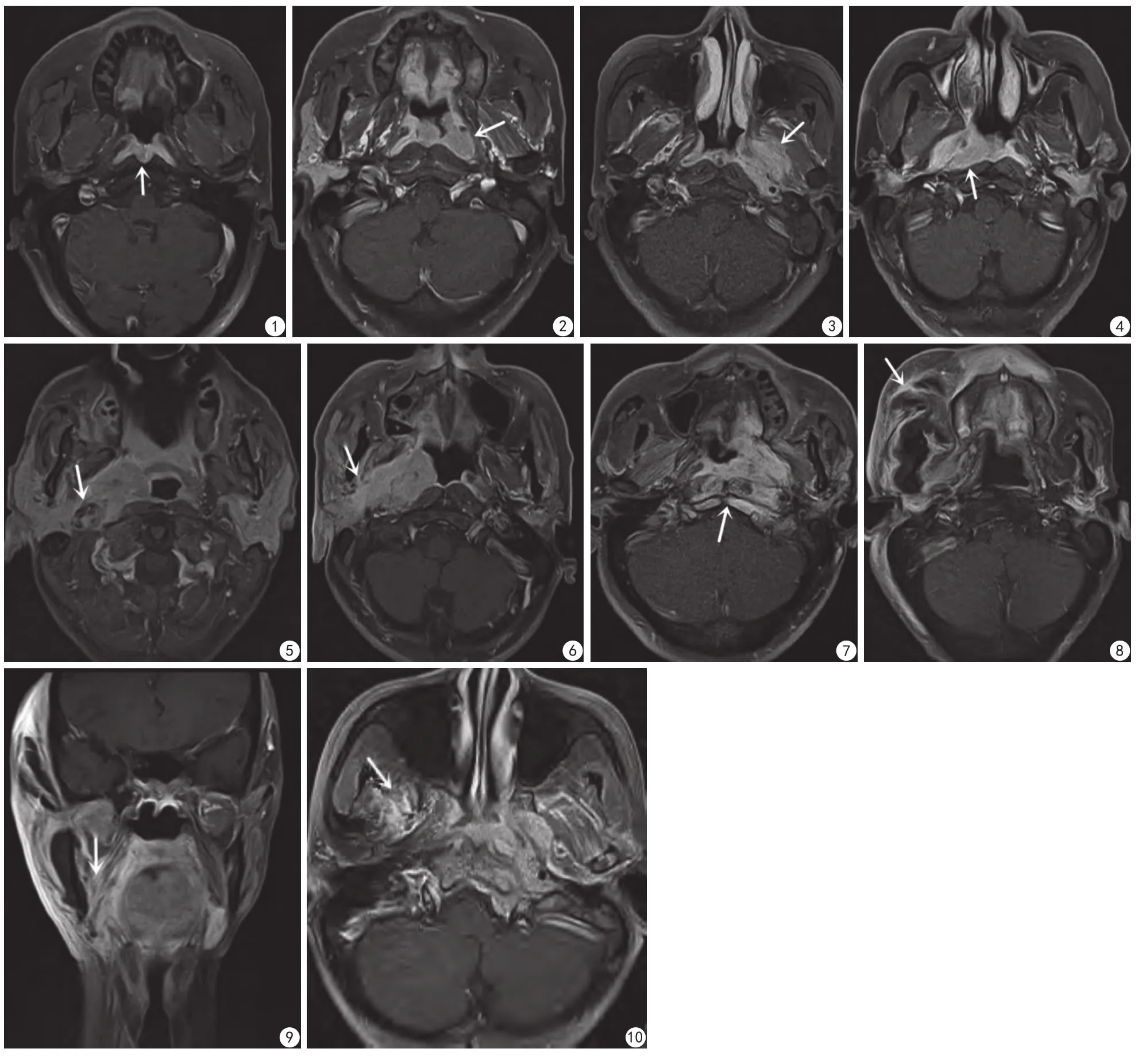
图1 FSE序列轴面T1WI增强示肿瘤仅局限于咽黏膜间隙,未突破咽颅底筋膜 图2 FSE序列轴面T1WI增强示左侧腭帆张肌明显强化,提示病灶突破咽颅底筋膜侵及左侧咽旁间隙 图3 FSE序列轴面T1WI增强示左侧翼内外肌明显强化,提示病灶侵及左侧咀嚼间隙 图4 FSE序列轴面T1WI增强,咽上缩肌及椎前肌间脂肪间隙消失,提示咽后间隙受侵 图5,6 FSE序列轴面T1WI增强示病灶包绕右侧颈动脉,并与腮腺分界不清,呈明显强化,提示右侧颈动脉间隙及腮腺间隙受侵 图7 FSE序列轴面T1WI增强示双侧头长肌呈明显不均匀强化,提示椎周间隙受侵图8 FSE序列轴面T1WI增强示右侧上颌骨牙槽外方的脂肪间隙内明显不均匀强化,提示面颊间隙受侵 图9 FSE序列轴面T1WI增强示右侧颌下腺及周围脂肪间隙内见明显强化灶,提示下颌下间隙受侵 图10 FSE序列轴面T1WI增强示右侧翼外肌明显不均匀强化,其内侧翼内肌信号尚均匀,未见异常强化灶Fig. 1 FSE sequence axial surface T1WI enhancement showed the tumor only confined to the PMS, without breaking the pharyngobasilar fascia.Fig. 2 FSE sequence axial surface T1WI enhanced showed on the left ensor palatinimuscle obvious reinforcement, suggesting the lesion broke through the pharyngeal fascia and the left PPS. Fig. 3 FSE sequence axial surface T1WI enhancement showed in the left medial pterygoid muscle strengthen,suggesting lesion invaded the left MS. Fig. 4 FSE sequence axial T1WI enhancement, pharyngeal muscle and intercostal muscle fat gap disappeared,suggesting the RPS invasion. Fig. 5, 6 FSE sequence axial surface T1WI enhancment showed lesions surrounded the right carotid artery, and had no clear boundary between parotid gland, was significantly enhanced, suggesting that the right CS and PS invasion. Fig. 7 FSE sequence axial surface T1WI enhancement in double side musculus longus capitis was obviously uneven reinforced, suggesting the PVS invasion. Fig. 8 FSE sequence axial surface T1WI enhancement showed signi ficant nonuniform reinforcement in the fat gap outside the right maxillary alveolar, suggesting the BS invasion.Fig. 9 FSE sequence axial surface T1WI enhanement showed the right side of the submandibular gland and the surrounding fat gap saw signi ficant enhancement lesions, the SMS was invaded. Fig. 10 FSE sequence axial surface T1WI enhancment showed on the right lateral pterygoid muscle obvious uneven reinforcement, its medial pterygoid was uniform, no abnormal strengthening.
2.3 本组鼻咽癌舌骨上颈部间隙侵犯程度
根据“鼻咽癌2008年分期标准”中T分期的各项标准,200例鼻咽非角化性(未分化)癌中T1期8例(4.0%),T2期34例(17.0%),T3期61例(30.5%),T4期97例(48.5%)。
MRI显示鼻咽癌各T分期侵犯舌骨上筋膜间隙的结果见表5。
T1期8例,肿瘤均局限于咽黏膜间隙。T2期34例, 其中22例(64.7%)肿瘤突破咽颅底筋膜侵犯咽旁间隙,经χ2检验,咽黏膜间隙侵犯率与咽旁间隙侵犯率之间的差异具有统计学意义(χ2=4.753,P=0.029)。T3期61例,肿瘤各舌骨上颈部筋膜间隙的侵犯率由高到低依次为咽黏膜间隙(100%,61/61)、咽旁间隙(100%,61/61)、咽后间隙(77.0%,47/61)、咀嚼间隙(68.9%,42/61)、椎周间隙(67.2%,41/61)、颈动脉间隙(37.7%,23/61),其相互之间的差异,具有统计学意义(χ2=89.506,P<0.01)。腮腺间隙、下颌下间隙、面颊间隙以及颈后间隙均未见侵犯征象。T4期97例,肿瘤对舌骨上各筋膜间隙的侵犯率依次为咽黏膜间隙(100%,97/97)、咽旁间隙(100%,97/97)、咀嚼间隙(100%,97/97)、咽后间隙(80.4%,78/97)、椎周间隙(76.3%,74/97)、颈动脉间隙(35.1%,34/97)、腮腺间隙(14.4%,14/97)、下颌下间隙(2.1%,2/97)及面颊间隙(1.0%,1/97),其相互之间的差异,具有统计学意义(χ2=588.727,P<0.01)。颈后间隙未见受侵征象。
3 讨论
3.1 鼻咽癌向周围侵犯的特点
从各个间隙的解剖分布可以看出,高危组毗邻于鼻咽腔或位于颅底中线上,而中危组和低危组与鼻咽腔距离较远或与鼻咽腔间隔解剖屏障,由此表明鼻咽癌遵循从近到远逐步进行局部侵犯,跳跃性扩散较少见,与文献报道一致[5]。
而在高危组间隙中,咽旁间隙侵犯率最高,这与其特殊的解剖关系密不可分,虽然其内侧的咽颅底筋膜是一个有效的屏障,但在咽颅底筋膜的上部分,紧靠咽隐窝处有一个Morgagni窦开口于鼻咽腔[6],这是肿瘤进入咽旁间隙的薄弱点,而咽隐窝又是鼻咽癌最好发部位,因此咽旁间隙较其他间隙早期更容易受侵。
本研究定义鼻咽癌向双侧侵犯是基于肿瘤侵犯超过鼻咽中线,结果显示肿瘤向双侧侵犯明显多于单侧侵犯。Sham等[7]研究247例患者鼻咽多点活检病理确诊单侧鼻咽癌的发生率只有2.8%,与本研究结果一致。原因可能是因为鼻咽癌起源于鼻咽腔内表面的黏膜上皮,该黏膜上皮部位表浅、左右连续,没有自然分界,使肿瘤极易跨过中线侵犯对侧,也可能是黏膜多处起源。
通过对紧邻鼻咽部的舌骨上三个筋膜间隙侵犯率两两对比分析,得出鼻咽部侧方的咽旁间隙侵犯率大于后方的咽后间隙、咽后间隙侵犯率大于侧后方的颈动脉间隙,因此笔者可以认为鼻咽癌向周围生长的大致规律为:向侧方浸润多于向后方,而向后方浸润又多于向侧后方。
3.2 T分期肿瘤对舌骨上颈部筋膜间隙侵犯的特点(按照“2008鼻咽癌分期标准”)
(1) T1期:肿瘤局限于鼻咽腔,向前不超过双侧上颌窦后壁连线;向下不超过C2椎体下缘,向侧及向后肿瘤未突破咽颅底筋膜[3]。鼻咽癌早期发病隐匿,自行就诊的患者只有10%~20%属早期,绝大多数属中晚期[8],所以虽然MRI诊断鼻咽部病灶的敏感度为100%,特异度和准确度均达到95%[9],但绝大多数患者就诊时已属于中晚期,因此T1期病例搜集困难,仅占全组病例的4%,肿瘤均局限于咽黏膜间隙,而对舌骨上其他筋膜间隙并未累及。(2) T2期:肿瘤侵犯鼻腔、口咽、咽旁间隙[3]。本组病例占全组病例的17%,其中64.7%的肿瘤同时侵犯了咽黏膜间隙及咽旁间隙,而35.3%的肿瘤未突破咽颅底筋膜侵犯咽旁间隙,仅局限于咽黏膜间隙内。有文献报道,1/4的T2期患者肿瘤侵犯仅局限于咽颅底筋膜[10],而本组数据也证明了此观点。2008分期中椎前间隙受侵已被剔除T2分期[5],其原因可能是椎前间隙毗邻于咽后间隙,向上与颅底相通、向下到达口咽、侧方与咽旁间隙相连。椎前间隙受侵导致颅底骨质、口咽及咽旁间隙受侵发生率明显增加,并且可能导致患者预后较差[11]。(3) T3期及T4期:2008新分期将咀嚼间隙中的翼内肌及翼肌间隙侵犯归为T3,咀嚼间隙其他部分侵犯归为T4。笔者发现,大多数病例咀嚼肌间隙的侵犯一般沿翼内肌、翼肌间隙、翼外肌、颞肌、咬肌由内向外循序前进,与文献报道一致[12],但有个别病例仅表现为翼外肌受侵(图10),与肿瘤常规播散途径不同。复习解剖发现翼外肌还有另一个头起自于蝶骨大翼外侧面,该起点高于翼内肌的起点翼内板和舟状窝,当肿瘤突破咽颅底筋膜后可沿颅底外侧面直接侵犯翼外肌。仔细观察发现翼内、外肌由肿大的淋巴结直接侵犯也不少见,肿大淋巴结侵犯咀嚼肌间隙与鼻咽部肿块侵犯咀嚼肌间隙在临床意义上是否不同尚待进一步研究。
另外,极少数病例中,与鼻咽部解剖位置较远的下颌下间隙及面颊间隙出现了受侵征象,原因可能是鼻咽癌除了具有很强的局部侵袭力外,还可以通过黏膜下淋巴管随淋巴引流而扩散到附近器官,而这种潜在、深部发展的浸润,其侵及范围不易估计,致使放射治疗时病灶遗漏而造成鼻咽癌的复发。此外,有学者提出鼻咽癌多中心学说,即鼻咽癌病灶可以存在二个以上癌灶,而且也可以在同一鼻咽腔内出现不同的癌变阶段,一处癌灶治好了,另一处的癌前病变却转变成另一个癌灶,这可能是造成临床复发的另一个原因。
鼻咽癌对于周围舌骨上筋膜间隙的侵犯中,咽旁间隙侵犯率最高,颈后间隙是唯一未受侵犯的舌骨上筋膜间隙;鼻咽癌向双侧浸润明显多于向单侧浸润;向周围生长的模式为:向侧方浸润多于向后方,向后方浸润多于向侧后方。
由于鼻咽癌周围受侵犯组织无法进行病理学检查,所以肿瘤对舌骨上筋膜间隙内结构的浸润并没有金标准可供对照,同时人为因素也不可忽视,因此对于肿瘤侵及范围,有可能存在一定偏差。颈后间隙是唯一未见受侵征象的舌骨上间隙,考虑到其内含丰富的淋巴组织,是否首先发生淋巴转移,有待进一步研究探讨。
[References]
[1] Pan JJ. Revision of the 92 phase of nasopharyngeal carcinoma. Chin J Radiat Oncol, 2009, 18(1): 2-6.潘建基. 鼻咽癌’92分期修订工作报告. 中华放射肿瘤学杂志,2009, 18(1): 2-6.
[2] Jiang GH, Zhang ZL, Tian JZ, et al. Suprahyoid neck fascia space MR imaging. Radiol Pract, 2001, 16(1): 23-26.江桂华, 章志霖, 田军章, 等. 舌骨上颈部筋膜间隙MR成像. 放射学实践, 2001, 16(1): 23-26.
[3] Chen L, Liu LZ, Mao YP, et al. Grading of MRI-detected skull-base invasion in nasopharyngeal carcinoma and its prognostic value. Head Neck, 2011, 33(9): 1309-1314.
[4] Li WF, Sun Y, Chen M, et al. Locoregional extension patterns of nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Chin J Cancer, 2012, 31(12): 579-587.
[5] Chen YB, Fang YH, Chen Y, et al. MRI study on the relationship between the invasion of peripheral structures and tumor staging of nasopharyngeal carcinoma. Chin J Radiol, 2010, 44 (10): 1024-1029.陈韵彬, 方燕红, 陈英, 等. 鼻咽癌侵犯周围结构与肿瘤分期关系的MRI研究. 中华放射学杂志, 2010, 44(10): 1024-1029.
[6] Silver AJ, Mawad ME, Hilal SK, et al. Computed tomography of the nasopharynx and related spaces. Part I: Anatomy. Radiology, 1983,147(3): 725-731.
[7] Sham JS, Wei WI, Kwan WH, et al. Fiberoptic endoscopic examination and biopsy in determining the extent of nasopharyngeal carcinoma. Cancer, 1989, 64(9): 1838-1842.
[8] Gu XZ, Yin WB, Xu GZ, et al. Radiation oncology. Beijing: Union Medical College press, 2008: 452.谷铣之, 殷蔚伯, 徐国镇, 等. 肿瘤放射治疗学. 北京: 北京协和医科大学出版社, 2008: 452.
[9] King AD, Vlantis AC, Tsang RK, et al. Magnetic resonance imaging for the detection of nasopharyngeal carcinoma. Am J Neuroradiol,2006, 27(6): 1288-1291.
[10] King AD, Lam WW, Leung SF, et al. MRI of local disease in nasopharyngeal carcinoma: tumour extent vs tumour stage. Br J Radiol, 1999, 72(860): 734-741.
[11] Li SE, Liang SB, Zhang N, et al. MRI evaluation and prognosis of nasopharyngeal carcinoma with anterior intervertebral space invasion. Chin J Radiat Oncol, 2013, 22(4): 295-298李绍恩, 梁少波, 张宁, 等. 鼻咽癌椎前间隙受侵的 MRI 评价及预后价值. 中华放射肿瘤学杂志, 2013, 22(4): 295-298.
[12] Hu WY, Zhou L, Chen XZ, et al. MRI findings of nasopharyngeal carcinoma with involvement of the masticatory muscle space. Radiol Pract, 2010, 25(10): 1103-1106.胡望远, 周玲, 陈晓钟, 等. 鼻咽癌咀嚼肌间隙侵犯的MRI表现. 放射学实践, 2010, 25(10): 1103-1106.
MRI T staging of nasopharyngeal carcinoma involving the fascial spaces of suprahyoid neck
WANG Wei-ling, ZHOU Yao, WANG Rong-pin*, HE Xi, LIU Chang-jie
Department of Radiology, Guizhou Provincial People's Hospital, Guiyang 550002,China
*Wang RP, E-mail: wangrongpin@126.com
Objective: To investigate the general invasiveness laws of nasopharyngeal carcinoma (NPC) for fascial spaces of suprahyoid neck and its relationship with T staging by using MRI examination. Materials and Methods: A retrospective analysis of 200 cases of newly diagnosed patients with NPC confirmed by pathology was performed at Guizhou Provincial People's Hospital from July 2013 to March 2016. All the patients underwent plain and enhanced MRI examination. Neoplasm involving the fascial spaces of suprahyoid neck and its relationship with T staging were performed by two experienced radiologists according to the newly revised clinical staging form "2008 staging of NPC" by China Work Committee of NPC. Results: (1) The frequency of neoplasm involving the fascial spaces of suprahyoid neck were the following: pharyngeal mucosa gap (200 cases), parapharyngeal space (180 cases),chewing gap (139 cases), retropharyngeal space (125 cases), vertebral round gap(119 cases), carotid space (57 cases), parotid space (14 cases), submandibular space(two cases), cheek gap (1 case). Tumors involving the fascial spaces of suprahyoid neck were found to be: invasiveness of lateral parapharyngeal space was more than that of rear retropharyngeal space, invasiveness of rear retropharyngeal space was more than that of lateral to the rear of the carotid space, and invasiveness of bilateral was more than that of unilateral in filtration. (2) Eight cases(4.0%) of NPC were T1 stage and tumors con fined to the pharyngeal mucosa gap. Thirty-four cases (17.0%) of tumors, among them 64.7% (22/34) were T2 stage and brokethrough the pharyngobasilar fascia and extent to the parapharyngeal space. Sixty-one cases(30.5%) of tumors were T3 stage, and the frequency of neoplasm involving the fascial spaces of suprahyoid neck were found to be:pharyngeal mucosa gap/ parapharyngeal space 100% (61/61), retropharyngeal space 77.0% (47/ 61), chewing gap 68.9% (42/ 61),vertebral week gap 67.2% (41/ 61), carotid space 37.7% (23/ 61). No neoplasm invasiveness was found in the submandibular space,parotid space, cheek and neckgap. Ninety-seven cases (48.5%) of patients were T4 stage and the frequency of neoplasm invasiveness were found to be: pharyngeal mucosa clearance/ swallow next to the gap/chewing gap of 100% (97/97), retropharyngeal space 80.4%(78 /97), vertebral week gap 76.3% (74 /97), carotid space 35.1% (34/97), parotid gap of 14.4% (14/97), lower jaw gap 2.1% (2/97),cheek gap of 1.0% (1/97). No neoplasm invasiveness was found in the rear neck gap. (3) The unilateral and bilateral invasion of the nasopharyngeal carcinoma to the surrounding space: 30.2% (58/192), 69.8% (134/192). Conclusions: Nasopharyngeal carcinoma has an attribute of involving various fascial spaces of suprahyoid neck. Parapharyngeal spaces invasiveness were found to be the highest one, and the posterior cervical space were found to be the only free space of invasiveness. Tumor involving the fascial spaces of suprahyoid neck may be summerized as:invasiveness of lateral spacesis more than that of posterior spaces, and followed by lateral to rear spaces, and bilateral space invasiveness is more than unilateral in filtration.
Fascial spaces of suprahyoid neck; Nasopharyngeal neoplasms; Magnetic resonance imaging
Received 31 Jan 2017, Accepted 26 Mar 2017
王荣品,E-mail:wangrongpin@126.com
2017-01-31
接受日期:2017-03-26
R445.2;R766.4
A
10.12015/issn.1674-8034.2017.05.003
王蔚凌, 周瑶, 王荣品, 等. 鼻咽癌T分期累及舌骨上颈部筋膜间隙规律的MRI探讨. 磁共振成像, 2017, 8(5):331-336.

