Recent progress on nanoparticle-based drug delivery systems for cancer therapy
Yanru Xin, Mingming Yin, Liyuan Zhao, Fanling Meng, Liang Luo
College of Life Science and Technology, National Engineering Research Center for Nanomedicine, Huazhong University of Science and Technology, Wuhan 430074, China
Recent progress on nanoparticle-based drug delivery systems for cancer therapy
Yanru Xin, Mingming Yin, Liyuan Zhao, Fanling Meng, Liang Luo
College of Life Science and Technology, National Engineering Research Center for Nanomedicine, Huazhong University of Science and Technology, Wuhan 430074, China
The development of cancer nanotherapeutics has attracted great interest in the recent decade. Cancer nanotherapeutics have overcome several limitations of conventional therapies, such as nonspecific biodistribution, poor water solubility, and limited bioavailability. Nanoparticles with tuned size and surface characteristics are the key components of nanotherapeutics, and are designed to passively or actively deliver anti-cancer drugs to tumor cells. We provide an overview of nanoparticle-based drug delivery methods and cancer therapies based on tumor-targeting delivery strategies that have been developed in recent years.
Nanoparticles; nanomedicine; drug delivery; tumor targeting; cancer therapy
Introduction
Nanomedicine involves the development and application of nanometer-scaled materials in the diagnosis, treatment, and prevention of diseases. Its indications range from the medical applications of nanomaterials and biological devices to nanometer-scaled electronic biosensors. Nanoparticles are the key components of nanomedicine and have received extensive interest as promising drug-delivery systems for cancer diagnosis and treatment.1-3Nanoparticles applied as drug delivery systems are submicron-sized (100–1,000 nm) particles, devices, or systems synthesized from various materials, including polymers (e.g., polymeric nanoparticles, micelles, vesicles, or dendrimers),4lipids (liposomes),5viruses (viral nanoparticles),6and even inorganics.7,8By using either passive or active targeting strategies, nanoparticles can increase the intracellular concentration of drugs in cancer cells while preventing toxicity to normal cells. Nanoparticles are usually enveloped by endosomes via receptor-mediated endocytosis after entering tumor cells, therefore escaping P-glycoprotein recognition,9one of the main mechanisms of drug resistance.
However, although nanoparticles are promising drug carrier systems, their poor oral bioavailability, instability in circulation, inadequate tissue distribution, and toxicity are some limitations to practical application that remain unresolved. In 2016, Wilhelm et al.10surveyed the literature from the past 10 years on nanoparticle-based drug carriers; their review showed that only 0.7% (median) of the administered nanoparticle dose was delivered to a solid tumor. This low delivery efficiency negatively affects the translation of nanotechnology to clinical applications.
To overcome these concerns and to satisfy safety, regulatory, and ethical requirements, researchers have continued to develop nanomedicine with improved characteristics. A more recent review by a group of pioneers in nanomedicine has provided a comprehensive overview of developments and current challenges in the field. The review also highlighted the upcoming opportunities in the field and clinical applications11of nanomedicine for in vivo diagnosis, in vitro diagnosis, in vivo therapeutics, and implantable materials.
Despite of all the problems associated with nanomedicine, nanoparticle-based drug delivery systems remain as a potential strategy for cancer therapy. Some nanoparticle formulations for cancer treatment have been already approved by regulatory agencies. These formulations exert fewer adverse effects than unmodified or bare drugs. Considerable effort has been expended to develop systems with precisely controlled functions and material properties. In this review, we will focus on the recent progress in the development of novel responsive nanoparticle systems withhigh sensitivity to tumor microenvironments for improved cancer diagnosis and treatment, as well as on combined nanoparticle-assisted cancer therapies.
Tumor targeting by nanoparticles
The basis of tumor-targeting drug delivery systems is the ability of nanoparticles to passively or actively accumulate in the desired tissues or cells. In passive targeting, nanoparticles are designed for transport through leaky vessels and the unique intra-organ pressures of tumors. In active targeting, nanoparticles are designed to adhere to specific biological structures in tumors via the molecular recognition of surfacebound ligands. The nanoparticles and loaded drugs thus escape immune clearance, avoid nonspecific cell uptake, and specifically accumulate in the targeted tumor cells and tissues.
Enhanced permeability and retention (EPR) effect
EPR effect is the property by which molecules of certain sizes (normally 100–1,000 nm) preferentially accumulate in tumor tissues instead of in normal tissues. Given their vigorous activity, tumor cells require more nutrients than normal cells, thus leading to the secretion of vascular endothelial growth factor and other growth factors that promote angiogenesis in tumors. Compared with that of normal vessels, the endothelial gap of new blood vessels is larger, thus facilitating the transport of macromolecular substances through blood vessels to tumor tissue. In addition, the lack of lymphatic vessels causes lymph circumfluence to suffocate. Under these double circumstances, macromolecular substances, or nanoparticles, accumulate in tumor tissues. EPR-passive targeting is the basis of tumor drug delivery. By stimulating tumor vasodilation, reducing lymphocytes, and extending circulation time, we can maximize the EPR effect of tumortargeting delivery systems.
Park et al.12developed a new type of porous silicon nanoparticle to decrease the metabolic rate and increase the circulation time of loaded drugs in the body. To allow the nanomaterials to accumulate in the tumor site, the group used silicon and silicon dioxide as the core of the nanoparticles and packed dextran outside of the nanoparticles after drug loading. After loading on the formed luminescent porous silicon nanoparticles (LPSiNPs), the circulation time of the drugs in the body was extended. The fluorescence emitted by the LPSiNPs under near-infrared (NIR) excitation can be used to trace the metabolism of the drug in the body. Low toxicity metabolism, extended circulation time, and fluorescence tracing make LPSiNPs a unique nanomaterial with broad prospective applications.
Mundra et al.13covalently conjugated indocyanine green (ICG)-NH2to the pendant carboxyl groups of poly (ethylene glycol)-block-poly(2-methyl-2-carboxyl-propylene carbonate) copolymer via carbodiimide coupling. The system self-assembles into micelles with a particle size of 30–50 nm and high ICG loading. In vivo NIR imaging demonstrated that ICG-conjugated micelles have prolonged circulation time and increased tumor accumulation through the EPR effect. Compared with the control ICG solution, the NIR-irradiated ICG-conjugated micelles have improved therapeutic efficacy with complete tumor regression in an A375 human melanoma tumor model in athymic nude mice.
pH response
The abnormal metabolism and protein regulation of tumor tissues form an acidic microenvironment that favors the proliferation of tumor cells. This pH abnormality is widely exploited in tumor-targeted delivery. In the acidic microenvironment of tumors, nanocarrier structures can be changed by chemical bond dissociation or charge reversal for specific drug release.
To overcome the resistance of breast cancer to doxorubicin (DOX), which is currently the most widely used anti-cancer drug, Yu et al.14constructed pH-sensitive microspheres that encapsulate DOX. The microspheres are formed by the selfassembly of polyethylene glycol (PEG)-block-poly[2-(diisopropylamino)ethyl methacrylate (PEG-b-PDPA)], and D-a-tocopheryl PEG 1000 succinate (TPGS). DOX is encapsulated in the cores of the microspheres. The microspheres are stable under the normal pH level of 7.4 but are degraded after cellular absorption. The early endosome and dissolved enzyme in tumor cells provide an acidic environment, which transforms the protonated PDPA/ TPGS@DOX microspheres into micelles and releases DOX in the cells. At the same time, TPGS greatly reduces the toxicity of mitochondria, thus leading to the synergistic effect of the treatment.
Lee et al.15designed pH-responsive intelligent microspheres Doxorubicin (DOX) loaded P(Asp-g-Im)-PEG micelles (DPHAIM, Figure 1) for the weakly acidic tumor microenvironment. With aspartic acid imidazole as the hydrophobic group and ethylene glycol as the hydrophilic group, the formed copolymer P(Aspg-Im)-PEG can load up to 28% DOX. In the pH<7 acid conditions of the tumor microenvironment, the microspheres are protonated and dissolved, thus releasing DOX and achieving the goal oftargeted DOX delivery with reduced toxicity.
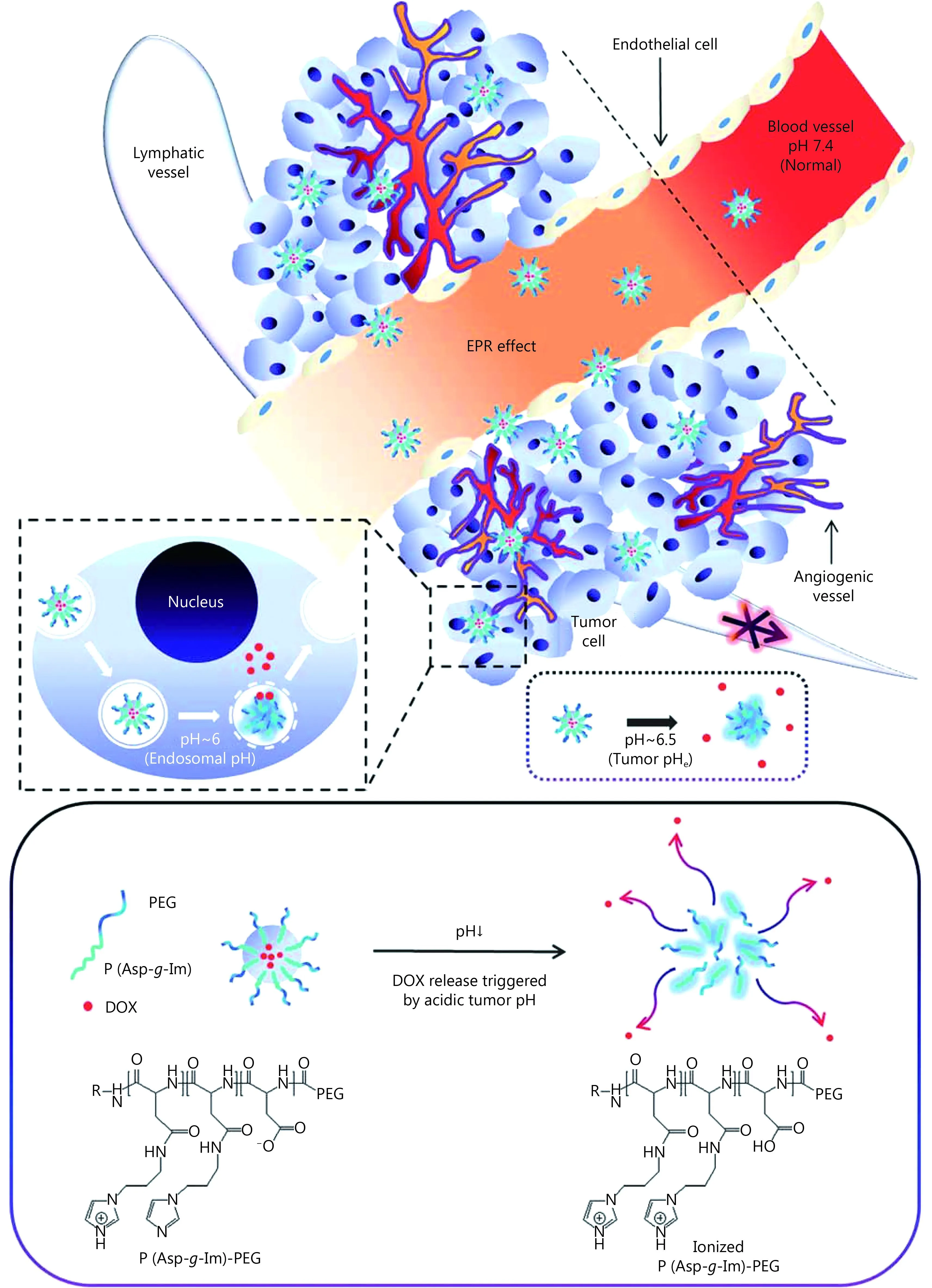
Figure 1 Schematic for the proposed in vivo behavior of DPHAIM. Reproduced with permission from Ref. 15.
Talelli et al.16developed a multi-layer package for the targeted delivery of DOX and to overcome its serious side effects. DOX derivatives are introduced into the core of the polymer micelles by covalent coupling. Under weak acidic conditions, such as the tumor microenvironment and theendosome, covalent bonds are broken and free DOX derivatives are released. Experiments showed that only approximately 5% of the drug is released under pH 7.4 but is fully released within the same duration at pH 5 and 37°C. This result indicated the good characteristics of targeted drug delivery and reduced damage to normal tissues.
Numerous pH-responsive, intelligent nanoparticle delivery examples have been developed. A double-strand pH-sensitive DNA has been developed to release DOX to the tumor17. Jia et al.18also designed a nanovehicle with hydrophilic methoxy poly(ethylene glycol) (mPEG)-PBA and hydrophobic HEHDO, which has a pH-labile profile. Torres et al.19developed a pH-sensitive liposome system that accelerates cytosolic release at pH values of 5.5–6.0. Seib et al.20synthesized silk nanoparticles with pH-dependent release (pH 4.5>6.0>7.4). Battogtokh et al.21reported an acidcleavable nanocarrier with enhanced cellular delivery at pH 6.5 compared with that at pH 7.4; by contrast, the cellular delivery of drugs by noncleavable nanocarriers showed no difference at pH 5.5 and pH 7.4. Tail vein injections enhance the intracellular uptake of the acid-cleavable nanocarrier relative to the noncleavable nanocarrier into the tumor cells of tumor-bearing mice, although total tumor accumulation is not significantly different. Van Butsele et al.22reported the preparation and the aqueous solution properties of hybrid polymeric micelles that consist of a hydrophobic poly (εcaprolactone) (PCL) core and a mixed shell of hydrophilic poly(ethylene oxide) and pH-sensitive poly (2-vinylpyridine).
Temperature response
The temperature of tumor tissues is slightly higher than that of surrounding normal tissues. This temperature difference can be applied in temperature-responsive drug delivery to tumors. Lv et al.23developed a novel polymer system for intelligent drug release; the developed system is based on molecular recognition and phase transition temperature response (Figure 2). In their nanoparticle drug delivery system, magnetic Fe3O4colloidal nanocrystal clusters (MCNCs) are used as the core, and poly (N-isopropylacrylamide) is used as a communication bridge between MCNCs and β-cyclodextrin (β-CD). β-CD can incorporate a number of hydrophobic groups and can easily load hydrophobic 8-anilino-1-naphthalenesulfonic acid ammonium salt (ANS) drugs. The conformation of MCNCs changes with the change in external magnetic field and temperature, thus decreasing the drug loadings of the whole system and consequently releasing ANS. The release rate of ANS from a drug nanoparticle system is easily controlled by simply adjusting external temperature. These nanoparticles have great potential for targeted delivery.
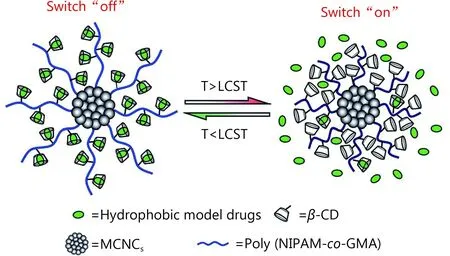
Figure 2 Schematic of the temperature-switched Fe3O4@PNGCD nanosystem for controlled drug release. Reproduced with permission from Ref. 23.
Talelli et al.24developed biodegradable thermosensitive polymeric micelles for the stable encapsulation of hydrophobic oleic-acid-coated superparamagnetic iron oxide nanoparticles (diameter 5-10 nm). The micelles are composed of amphiphilic, thermosensitive, and biodegradable block copolymers of poly (ethylene glycol)-bpoly[N-(2-hydroxypropyl) methacrylamide dilactate] [mPEGb-p(HPMAm-Lac2)]. Liu et al.25developed a precision cancer nanomedicine based on Bi2S3nanorods (NRs) designed specifically for multispectral optoacoustic tomography (MSOT)/X-ray computed tomography (CT). The as-prepared Bi2S3NRs exhibit an ideal photothermal effect and contrast enhancement in MSOT/CT bimodal imaging.
Enzymatic response
Some enzymes are only present or are highly concentrated in tumor cells. Their specific binding with enzyme substrates can be employed to achieve the intelligent response of targeting drugs. Mi et al.26constructed a multistage complex targeted drug delivery nanosystem enzyme-stimulated multistage vector (ESMSV) based on the special recognition between the enzyme and the appropriate substrate. A metalloproteinases-2 (MMP-2) enzyme substrate is modified on a polymer poly (lactic-co-glycolic acid) (PLGA)-PEG nanoparticle surface, followed by loading onto porous silicon. When ESMSV accumulates in pulmonary tumor tissues because of MMP2 enzymatic activity, the connecting structure between polymeric nanoparticles and porous silicon nanoparticles (SiNP) is destroyed, thus releasing polynanoparticles from porous silicon. These processes have been validated both in vivo and in vitro. The results indicated that ESMSV showed noticeable efficacy in the treatment of metastatic lung melanoma.
Tang et al.27reported a general strategy for the direct delivery of functional proteins to the cytosol by nanoparticlestabilized capsules (NPSCs). The effectiveness of these NPSCs as therapeutic protein carriers has been demonstrated through the delivery of fully functionalized caspase-3 to HeLa cells with concomitant apoptosis. The similar delivery of green fluorescent protein confirmed the cytosolic delivery and intracellular targeting of the delivered protein, thus demonstrating the utility of the system for both therapeutic and imaging applications.
Barve et al.28developed an enzyme-responsive peptide drug conjugate for TGX-D1, a promising PI3K inhibitor for prostate cancer. In this system, the LNCaP-specific KYL peptide is used as the targeting ligand and the prostatespecific antigen (PSA)-cleavable peptide (SSKYQSL) is used as the enzyme-responsive linker. Ruan et al.29experimentally proved that pre-incubating G-AuNP-DOX-PEG with MMP-2 can significantly enhance the penetrating efficiency of the drug. Yu et al.30developed surface-engineering nanoparticles with programmable extended circulation and targeting ability. The nanoparticles, which are structured with a targeting middle layer and a hydrophobic internal core, are constructed by mixing matrix metalloproteinase MMP2, MMP9-sensitive copolymers (mPEG-Pep-PCL), and folate receptor targeted copolymers (FA-PEG-PCL). The results showed the successful combination between enzymatic stimulus and surface-engineered technology for tumor targeting.
Antigen response
Similar to enzymes, the special identification and connection between antigens and antibodies can be exploited for the design of active targeting drug delivery. Ding et al.31utilized the specific binding between a receptor and a ligand to realize targeted drug delivery. The authors combined immune nanoparticles containing the death receptor 5 monoclonal antibody (DR5 mAb) and nanoparticles carrying kappa oxazine (DTIC) to form the composite nanoparticle DTIC NP-DR5 mAb. The drug-loading nanoparticles accumulate in tumor cells due to the specificity of the monoclonal antibody and DR5 recognition effect in the body. This system is also a good example of the combined therapy of immune therapy and chemotherapy. The authors demonstrated that DTIC-PLA-DR5 mAb nanoparticles are an active targeting drug delivery system that can specifically target DR5-overexpressing malignant melanoma cells and can be efficiently internalized. Most strikingly, compared with conventional DTIC-NPs, DTIC-NP-DR5 mAb showed significantly enhanced cytotoxicity and increased cell apoptosis in DR5-positive malignant melanoma cells.
Saraf et al.32synthesized cyclic Arg-Gly-Asp (RGD) micelles, which exhibit better targeting efficacy than linear RGD micelles as drug delivery vehicles. This improved targeting efficacy is attributed to the low drug solubilization and kinetic stability of the micelles. The results from the study proved the effectiveness of self-assembling lowmolecular-weight RGD amphiphiles as carriers for the targeted delivery of paclitaxel (PTX).
Nanoparticle-based cancer therapy
Magnetic therapy
Tissues rarely absorb magnetic waves, which penetrate deeper than visible light and infrared without side effects. Therefore, magnetic nanomaterials are good candidates for disease treatment. Magnetic nanoparticles, which mainly contain iron oxide, can be used for localized heating when triggered by a magnetic field. Carregal-Romero et al.33synthesized multilayer-assembled polyelectrolyte microcapsules with diameters of 4.6 µm. The walls of the microcapsules are integrated with 18 nm-diameter iron oxide nanotubes to supply a magnetic trigger for the release of molecules with low absorption and deep permeability. An organic fluorescent polymer (Cascade-Blue-labeled dextran) is then loaded onto the microcapsules as a model molecular cargo. Under an alternating magnetic field, the magnetic nanotubes can heat their surroundings and destroy the walls of the microcapsules, thus releasing the embedded cargo into the surrounding solution. The use of magnetic nanoparticles with high heating properties allows the release of the magnetic properties of the encapsulated material; moreover, this use provides the possibility of applying new and exciting materials in the body.
Fang et al.34employed core-shell magnetoresponsive virusmimetic nanocapsules (VNs) anchored with iron oxide nanoparticles for rapid and simultaneous drug release. The VNs produce a strong heating effect under an external high frequency magnetic field. Furthermore, the VNs can subsequently infect adjacent cancer cells and deliver sufficient therapeutic agents to the next target. Kuo et al.35used Fe3O4nanoparticles to encapsulate anticancer drugs and to immobilize the antibody-targeting peptide AP-1 (MPVA-AP1) to form multifunctional magnetic nanovehicles. The magnetic nanovehicles can be stably stored and exert thermotherapeutic (i.e., hyperthermia) and chemotherapeutic (i.e., anti-cancer drug) effects on tumor tissues under a high-frequency magnetic field. Lee et al.36used magnetoretic-responsive DOX-encapsulated supramolecular magnetic nanoparticles (DOX-SMNPs) as a unique onedemand drug release system to enhance therapeutic effects and attenuate systematic toxicity to the tumor. The SMNPs self-assemble from four different molecular building blocks: Ad-grafted polyamidoamine dendrimers, β-CD-grafted branched polyethylenimine, Ad-PEG, and 6-nm Ad-grafted Zn0.4Fe2.6O4superparamagnetic nanoparticles. Li and coworkers37designed a magnetothermally responsive nanocarrier, in which NIPAAm and HMAAm are composed of thermosensitive copolymers and Mn-Zn ferrite nanoparticles are embedded in the polymer matrix. Under an alternating magnetic field, this system demonstrated efficient therapeutic effects and good biocompatibility.
Photodynamic therapy (PDT)
PDT can kill tumor cells through the transformation of tumor oxygen into cytotoxic reactive singlet oxygen (1O2) under light irradiation. PDT is a safe and selective treatment method for various cancer types. However, the efficacy of PDT in tumor therapy is limited due to the hypoxic microenvironment of tumors and oxygen consumption during PDT. To overcome this problem, Cheng et al.38developed a novel oxygen self-enriched photodynamic therapy system by loading IR780 on perfluorohexane (PFH) nanodroplets. PFH can maintain a high oxygen content and extend1O2lifetime because of its high oxygen capacity. The photosensitizer IR780 is dispersed in a lipid monolayer composed of lecithin, cholesterol, and DSPE-PEG2000. Under irradiation by a NIR 808-nm laser, IR780 transfers energy to the oxygen enriched in the PFH, thus producing singlet oxygen and exerting a cytotoxic effect, which significantly improves the photodynamic effect. After intratumoral injection into tumors, tumor growth is inhibited in Oxy-PDT-treated mice. Later, Gong et al.39used PEGylated chlorine e6 (Ce6)-coupled poly (maleic anhydridealt-1-octadecene) to form Ce6-containing nanomicelles in an aqueous solution (Figure 3) and discovered that hyaluronidase resolves hyaluronan, a major component of extracellular matrix in tumors. The complex enhances the efficacy of nanoparticle-based PDT for in vivo cancer treatment.
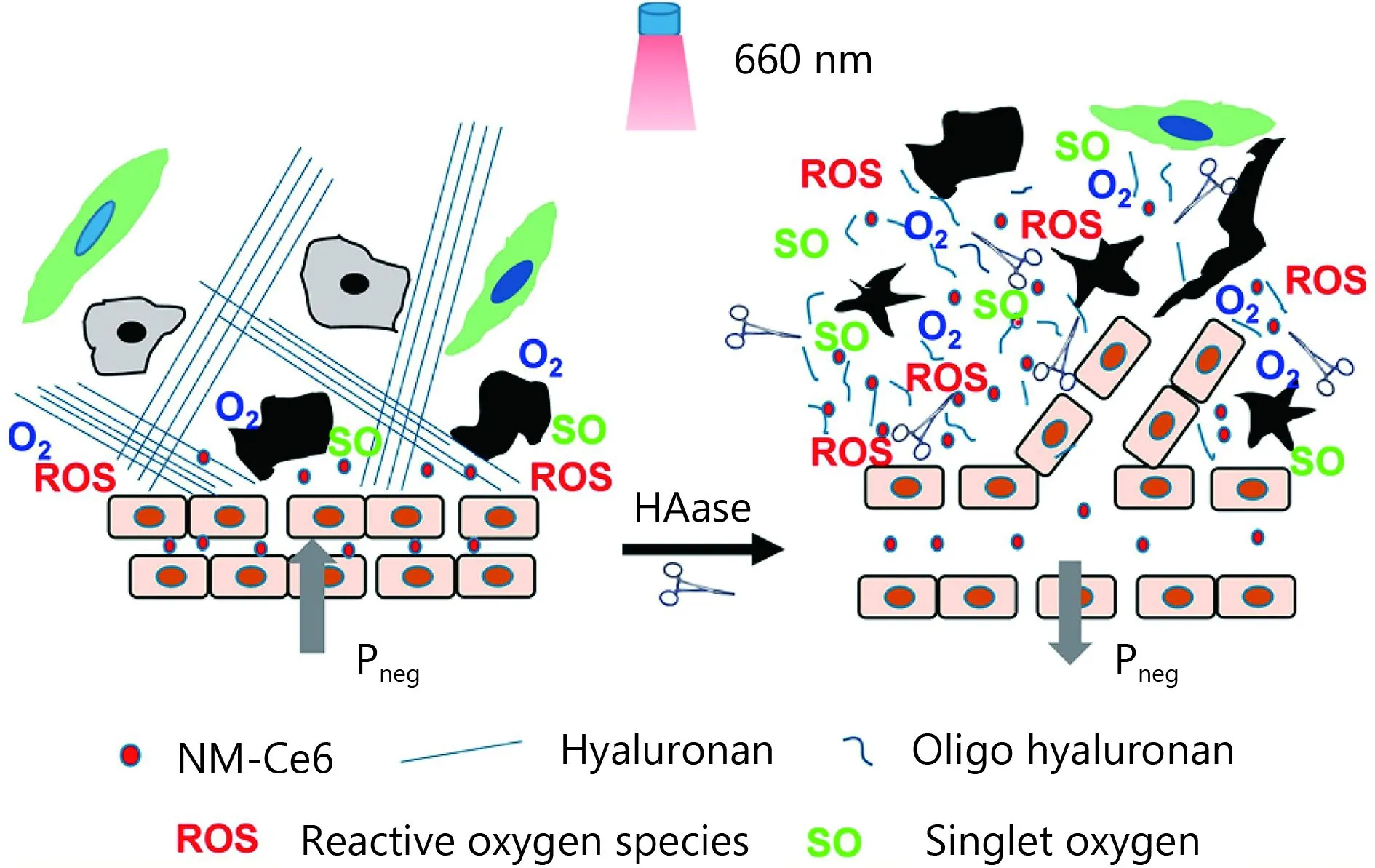
Figure 3 Scheme showing the effects of HAase on the modulation of the tumor microenvironment. By improving tumor oxygenation and promoting the EPR effect, HAase enhances the efficacy of in vivo PDT cancer treatment. Reproduced with permission from Ref. 39.
Hou et al.40developed a nanodumbbell model, which consists of a hydrophobic upconversion nanoparticle (UCN) core and a hydrophilic polymersome shell. UCN NaYF4:Yb:Er nanocrystals, which were synthesized via the thermal decomposition method, can be used as transducers to convert NIR light to visible light to activate the photosensitizers zinc (II) phthalocyanine (ZnPc) in photodynamic therapy. The polymersome lipid shell is used to load ZnPc and to avoid non-specific absorbance or corrosion during transportation. In addition, folic acid may combine with hybrid Fe3O4-ZnO (FZ-SFA) nanoparticles in therapeutic applications associated with PDT41. The photokilling effect and photo-induced toxicity are significantly enhanced under UV irradiation. To increase the production of reactive oxygen species (ROS) under normoxic and hypoxic conditions, Usacheva et al.42used a polymersurfactant nanoparticle system to load the photosensitizer methylene blue. Nanoparticles loaded with methylene blue can remove cancer stem cells under hypoxic conditions, therefore providing a novel route for cancer treatment.
Photothermal therapy (PTT)
In PTT, cancer tissues are irradiated with electromagnetic radiation, which elevates temperature to kill targeted cells. In this method, the careful selection of laser parameters and illumination can enable local light penetration for specific targeting.
One of the most promising directions for PTT is the use of plasma nanostructures, particularly gold nanostructures, such as gold nanoparticles (AuNPs) and gold nanoshells, to take the advantage of localized surface plasmon resonance. In addition, visible light with a longer wavelength or NIR can beused in PTT since they have a deep tissue permeation and low energy, which causes limited damage to other cells and tissues.
Chen et al.43combined NaYF4:Yb3+/Er3+nanoparticles with AuNPs and gold NRs (GNRs) coated with silica shells. The surfaces of the nanocomposites were then decorated with folic acid through multiple steps to form UCP@SiO2-NP-FA and UCP@SiO2-NR-FA (Figure 4). NaYF4:Yb3+/Er3+nanoparticles act as light converters and emit green and red light under 980 nm laser excitation. The silica shell increases biocompatibility and connects the nanoparticles and Au nanomaterials. This system exhibits significantly enhanced therapeutic efficacy.
Many other nanomaterials have been applied in PPT. Yang et al.44developed a double-shelled hollow sphere structure with luminescent Y2O3:Yb, Er as the inner shell and mesoporous silica as the outer shell. The surface of Y2O3:Yb, Er@mSiO2was then decorated with ultra small CuxS (semiconductor) nanoparticles (photothermal agents) and DOX to form a DOX-DSHS-CuxS composite. When irradiated with 980 nm NIR light, the composite showed high anti-cancer efficacy and biocompatibility in vitro and in vivo. AuNPs may also specifically conjugate with a thermally sensitive elastin-like polypeptide (ELP) to form ELPAuNPs45. The ELP-AuNPs, which contain short-necked gold nanostructures formed in situ at high temperatures by AuNP assemblies, exhibit strong NIR absorption and high light-heat effect, therefore enhancing therapeutic effect. Prussian blue nanoparticles are utilized as PTT agents in combination with MEK inhibitor and PD-032590146. This combined system inhibits tumor growth and increases survival rate by blocking MEK activity under NIR irradiation.
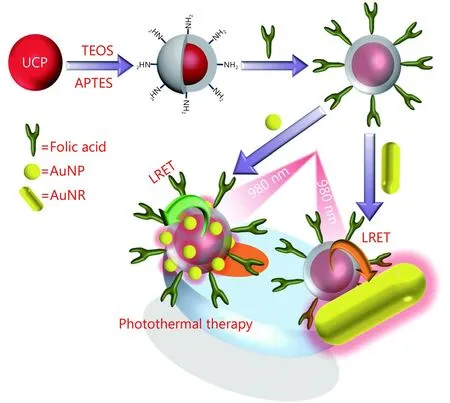
Figure 4 Schematic of the synthetic process of UCP@SiO2-NPs and UCP@SiO2-NRs and application in the PTT of oral cancer. Reproduced with permission from Ref. 43.
Radiotherapy (RT)
RT is a popular remote cancer treatment method that induces DNA damage or free radical damage in tumor sites. However, it causes severe side effects in patients. Protecting normal tissue adjacent to the tumor site from radiation damage remains challenging. Many approaches have been recently developed to improve the effect of RT and to decrease its side effects.
Yu and coworkers[47]used MPEG-PCL to prepare PTXNPs via the solid dispersion method. Although PTX is one of the most common antineoplastic drugs, its therapeutic effect is limited because of its short circulation half-life, poor water solubility, and serious side effects. With the rapid development of nanotechnology, nanoscale drug delivery systems now offer an alternative solution for drug transport to tumor tissues. Yu et al.47demonstrated that PTX-NPs inhibit tumor growth by acting on Ki-67 and inhibit angiogenesis in tumor tissues through RT. PTX-NPs combined with RT exhibit higher efficiency in cancer therapy than PTX-NPs or RT alone. Satterlee et al.48used lipidcalcium-phosphate nanoparticles in combination with177Lutetium (177Lu) for RT. Combretastatin A-4 phosphate was loaded onto nanoparticles to increase the enrichment of nanoparticles. Through the beta decay of177Lu, the combined system exerts significant inhibitory effects on tumor cell growth, as well as increases tumor EPR effect and nanoparticle uptake.
Zhang et al.49developed dual functional mesoporous silica nanoparticles (MSNs), by dissolving MSNs in valproic acid sodium salt solution to form VPA-MSNs. The developed VPA-MSNs enhance tumor cell death and decrease damage to healthy adjacent tissues by targeting cancer cells with overexpressed folic acid and by conditionally releasing VPA in an acidic turmeric microenvironment. Song et al.50developed epidermal growth factor (EGF)-AuNPs that consist of AuNPs as radiosensitizers and EGF. EGF was modified with diethylenetriaminepentaacetic dianhydride (DTPA) to form DTPA-EGF, which was further labeled with111In.111In-EGF-Au NPs specifically target EGFR-positive cancer cells and enhance cell death by increasing radiotoxicity with a high111In payload. Song et al.51prepared PEG-stabilized perfluorocarbon (PFC) nanodroplets decorated with TaOx nanoparticles as a multifunctional RT sensitizer. The complex improved in vivo RT treatment byconcentrating radiation energy and improving tumor oxygenation.
Ultrasound (US)
US is a conventional method for cancer diagnosis and treatment. It can form cavitation bubbles, heat local tissues, and produce radiation force, which are used to release drugs from nanocomposites, to purify drugs and/or nanoparticles from blood vessels in tumors, and to improve drug penetration to the tumor. Wang et al.52developed an efficient strategy to overcome multi-drug resistance (MDR) by combining negatively charged nanoparticles with US. In their study, cells are exposed to US with microbubbles prior to treatment with negatively charged Heparin-Folate-Tat-Taxol nanoparticles. This work reported that the optimal reversal of the MDR effect occurs through the enhancement of cell membrane permeability, the inhibition of cell proliferation rate, and the downregulation of the genes and proteins associated with MDR. Furthermore, US enhances the accumulation of nanoparticles by indirectly inducing the endosomal escape of negatively charged nanoparticles. The combined strategy can potentially overcome the MDR problem in cancer therapy. Sviridov et al.53prepared SiNPs by mechanically grinding luminescent porous silicon decorated with dextran. They found that dextran-coated SiNPs could significantly decrease cytotoxicity. After SiNP uptake, cells were treated with therapeutic US for 5–20 min. The living cells decreased whereas the total cells was almost unchanged, indicating the potential of the system as a mild cancer therapy. Brazzale et al.54used folic acid to decorate AuNPs surface-coated with PEG to stabilize the colloid and prevent opsonization in vivo. The nanoparticles, as US sensitizers, can specifically act on KB and HCT-116 cells and inhibit cell growth by generating reactive oxygen and increasing cell necrosis.
Combined cancer therapy
Although nanoparticle-based cancer therapies have already demonstrated intriguing therapeutic efficacies, researchers continue to pursue an ideal synergistic effect by combining two or more treatment methods. Significantly enhanced antitumor efficacy has been achieved by combined treatment strategies.
PTT and PDT combined therapy
Qiu et al.55devised a GNR-activated, cell-penetrating peptide-protoporphyrin (GNR-ACPP-PpIX) nanoplatform that can be applied for dual imaging and combined activatable PDT/PTT therapy (Figure 5A). In GNR-ACPI, GNRs are conjugated with a protoporphyrin (PpIX, a PDT agent) combined with ACPP. The ACPP comprises a matrix of the MMP-2-sensitive peptide sequence GPLGLAG. First, the special “U-type” structure of ACPP facilitates close contact between PpIX and GNR. As tumor cells can overexpress MMP-2, the GPLGLAG sequence is hydrolyzed by MMP-2 as soon as it arrives at the tumor site, leading to the release of residual CPP bound to PpIX (CPP-PpIX) and the recovery of the optical activity of PpIX. Moreover, with the help of CPP, the cellular uptake of PpIX by tumor cells can be more efficient, greatly enhancing PDT efficacy. GNR can also be used for photothermal imaging and PTT in the treatment of tumors. Experimental results show that the combination of PTT and PDT can greatly enhance the antitumor effect with negligible systemic toxicity.
Other PDT/PTT combined cancer therapy strategies and applied nanoparticle systems include: cyanine dye-integrated micelles loaded on photosensitizers as potential theranostic micelles56; Cit/CuS@Fe3O4-based nanoparticles for PDT/PTT therapy with magnetic-targeting capability57; collagen-gold hybrid hydrogels58; Au NR-capped and Ce6-doped mesoporous silica NRs; and Au NR-capped and Ce6-doped mesoporous silica nanorods59.
Chemotherapy and PTT combined therapy
In malignant glioma, treatment effect and patient compliance are unsatisfactory due to low efficiency and systemic side effects of treatment methods. Wang et al.60combined the chemo-photothermal targeted therapy of glioma with a novel multifunctional drug delivery system. A targeting peptidemodified graphene nanosheet coated with mesoporous silica (GSPI) was successfully synthesized. The developed DOX-loaded GSPI system (GSPID) showed good heat-stimulative, pH-responsive, and sustained release properties. Based on the results of cytotoxicity experiments, glioma cells treated with the combined therapy showed higher mortality rates than those treated with single chemotherapy or PTT alone. In addition, peptide modification significantly enhanced GSPID accumulation in glioma cells. GSPID demonstrated advanced chemo-photothermal synergistic targeted therapy and good drug release properties, providing an excellent drug delivery system for the combined therapy of glioma. In addition, this therapy can effectively avoid frequent and invasive dosing and improve patient compliance.

Figure 5 (A) Construction of the GNR-ACPI nanoplatform. (B) Dual-mode imaging and combined PTT/PDT therapy in vivo after the intravenous injection of GNR-ACPI. (B1) Accumulation of GNR-ACPI in the tumor site through the EPR effect. (B2) Enhanced internalization of activated CPP-PpIX by tumor cells via the help of CPP and triggered by the combination of PTT/PDT therapy upon laser irradiation. Reproduced with permission from Ref. 55.
Shao et al.61constructed a polydopamine-functionalized reduced graphene oxide (pRGO) with mesoporous silica (MS) coating. pRGO was further modified with hyaluronic acid (HA) to form pRGO@MS (DOX)-HA nanocomposites, a multimodal therapy system and a multifunctional drug delivery system. These nanoparticles exhibit efficient synergistic targeted chemo-PTT. With mussel-inspired dopamine as the reducing reagent, the functionalized biomolecule was prepared as biocompatible biopolymercoated RGO nanosheets in one step. Mesoporous silica (MS) was then coated with pRGO to enhance DOX loading and to provide an active interface for modification with HA, the targeting moiety. The pRGO@MS (DOX)-HA showed excellent photothermal properties and good dispersibility under NIR laser irradiation. Gao et al.62developed a thermal/pH dual-sensitive nanocarrier for the treatment of bladder cancer. Their results revealed that chemo/ photothermal targeted therapy might be more advantageous than conventional therapeutics for bladder cancer. Meng et al.63designed and synthesized a “smart” MEO2MA@ MEO2MA-co-OEGMA-CuS-DOX composite (abbreviated as G-CuS-DOX). The nanoparticles consisted of thermosensitive MEO2MA@MEO2MA-co-OEGMA nanogels, with a low critical solution temperature of 42°C, CuS as the photothermal component, and DOX as the anticancer drug. Upon the injection of the nanocapsule solution into tumors in mice, DOX is released and temperature elevation in the tumor can be switched on/off by an ex vivo NIR laser, thus exhibiting an efficient synergistic photothermal/chemotherapy for tumors. Shen et al.64studied the in vivo and in vitro ablation of the tumor via combined chemotherapy and PTT with DOX-loaded GNRs@mSiO2. Feng et al.65designed a magnetic tumor-targeting and NIR-responsive drug delivery system. This nanoplatform can generate improved photothermal transduction efficiency in a short time, and DOX is spontaneously released due to photohyperthermia with the spatiotemporal control of NIR irradiation.
Chemo-photodynamic combined therapy
Advanced colorectal cancer is one of the deadliest cancers. Traditional treatments, such as the inhibition of the PD-1/PD-L1 axis by antibodies, remain the most promising immunotherapies, but the sustained response rate of these therapies is very low. He et al.66developed nanoscale coordination polymer (NCP) core-shell nanoparticles, which carry oxaliplatin in the core and the photosensitizer pyropheophorbide-lipid conjugate (pyrolipid) in the shell (NCP@pyrolipid), for PDT, chemotherapy, and PD-L1 checkpoint blockade cancer therapy. NCP@pyrolipid has high drug loading and long circulation. It can also avoid being salvaged in the body; hence, it can be enriched in the tumor site. Research showed that upon subcutaneous injection in CT26 and HT29 mouse models, the PDT effect of NCP@pyrolipid effectively inhibits tumor growth. Moreover, the combination of oxaliplatin and PDT creates an immune microenvironment in the tumor site, significantly increasing the efficacy of the PD-L1 checkpoint blockade therapy. This strategy greatly increases the curative effect of tumor treatment strategies.
Dong et al.67introduced UCNs that were surface modified with bovine serum albumin-poly (ε-caprolactone) BSA-PCL, and achieved a combined system of tumor cell imaging, photodynamic therapy, and chemotherapy. The UCN core comprises a protein-polymer bioconjugate-coated multifunctional upconversion nanosystem. The antitumor drugs DOX and ZnPc are co-loaded in the tailored amphiphilic protein-polymer bioconjugate shell. In this structure, the UCN core converts NIR light to visible light, thus allowing for cell fluorescence imaging, whereas activated ZnPc generates cytotoxic ROS to achieve photodynamic therapy. The BSA-PCL system exhibits good stability, water solubility, and low cytotoxicity. Similarly, Ai et al.68assembled biocompatible core-shell-shell UCNs (NaGdF4:Yb/Nd@NaGdF4:Yb/Er@NaGdF4) loaded with photosensitizers and Pt (IV) prodrugs for simultaneous PDT and Pt chemotherapy. Chen et al.69developed a type of theranostic micelle based on multifunctional UCN, which combines chemotherapy and PDT for NIR-controlled and neuroendocrine tumor targeting. Feng et al.70prepared a nanovehicle that can co-deliver the photosensitizer pyropheophorbide-a (PPa) and the drug PTX through the synthesis of PPa-conjugated amphiphilic copolymer PPa-PLA-PEG-PLA-PPa. The nanovehicle has a high drugloading capacity for both drugs. Decorating the obtained nanoparticles with the tumor-targeting and penetrating peptide F3 achieved tumor-targeting therapy.
Immunotherapy and photothermal combined therapy
The immunotherapy and PTT bined therapeutic strategy can inhibit tumor metastasis and eliminate primary tumors through the combination of adjuvant nanoparticle-based PTT with checkpoint-blockade immunotherapy. Chen et al.71developed a class of PLGA-ICG-R837 nanoparticles, in which PLGA co-encapsulated imiquimod (R837) serves as a Tolllike-receptor-7 agonist and ICG serves as a photothermal agent. When excited by NIR light, the nanoparticles can generate a photothermal effect to eliminate the main tumor, and the contained R837 produces tumor-associated antigens and behaves as a vaccine. Anti-cytotoxic T-lymphocyte antigen-4 has been used as the checkpoint-blockade, which produces an immune response in mice to eliminate remaining tumor cells and to inhibit metastases. Moreover, this strategy is suitable for various kinds of tumor models and has the advantage of immune memory (Figure 6).
Whole tumor cell lysate (TCL) has been used as a tumor antigen for the development of cancer vaccines. Shi et al.72designed chitosan nanoparticles (CTS NPs) with surface mannose (Man) moieties (Man-CTS NPs) for the specific targeting of dendritic cells. The Man-CTS NPs were then loaded with TCL generated from B16 melanoma cells (Man-CTS-TCL NPs). TCL improves the efficacy of TCL-based vaccines as a result of the effective activation of humoral and cellular immunity. The traditional anti-fibroblast-activation protein (FAP) treatment is associated with numerous side effects. Studies have shown that FAP is excessively expressed on the surface of carcinoma-associated fibroblasts (CAFs); therefore, FAP can be used as a target antigen in tumor cells. Zhen et al.73reported a photoimmunotherapy (PIT) approach based on nanoparticles. The author applied ferritin, a compact nanoparticle protein cage, as the photosensitizer carrier connected with a FAP-specificity single-variable region (scFv). Under photoirradiation, nanoPIT can effectively eliminate CAFs in tumors but not harm healthy tissues due to localized targeting. The nanoPIT effectively suppresses tumor growth by inhibiting the secretion of C-XC motif chemokine ligand (CXCL12), thus enhancing T cell infiltration and in turn decreasing the number of tumor cells. Cano-Mejia et al.74combined Prussian-blue-nanoparticlebased PTT and anti-CTLA-4 checkpoint inhibition for neuroblastoma treatment. The strategy can lead to an immune response and decrease tumor burden. Huo et al.75proposed a PLGA-PEG-MBA micelle system for the implementation of the tumor-targeted delivery of a low dose of sunitinib. The therapy can decrease the number of MCSCs and Tregs in the tumor microenvironment, increase T-cell infiltration in the tumor site, and eliminate immunosuppression in the tumor site.
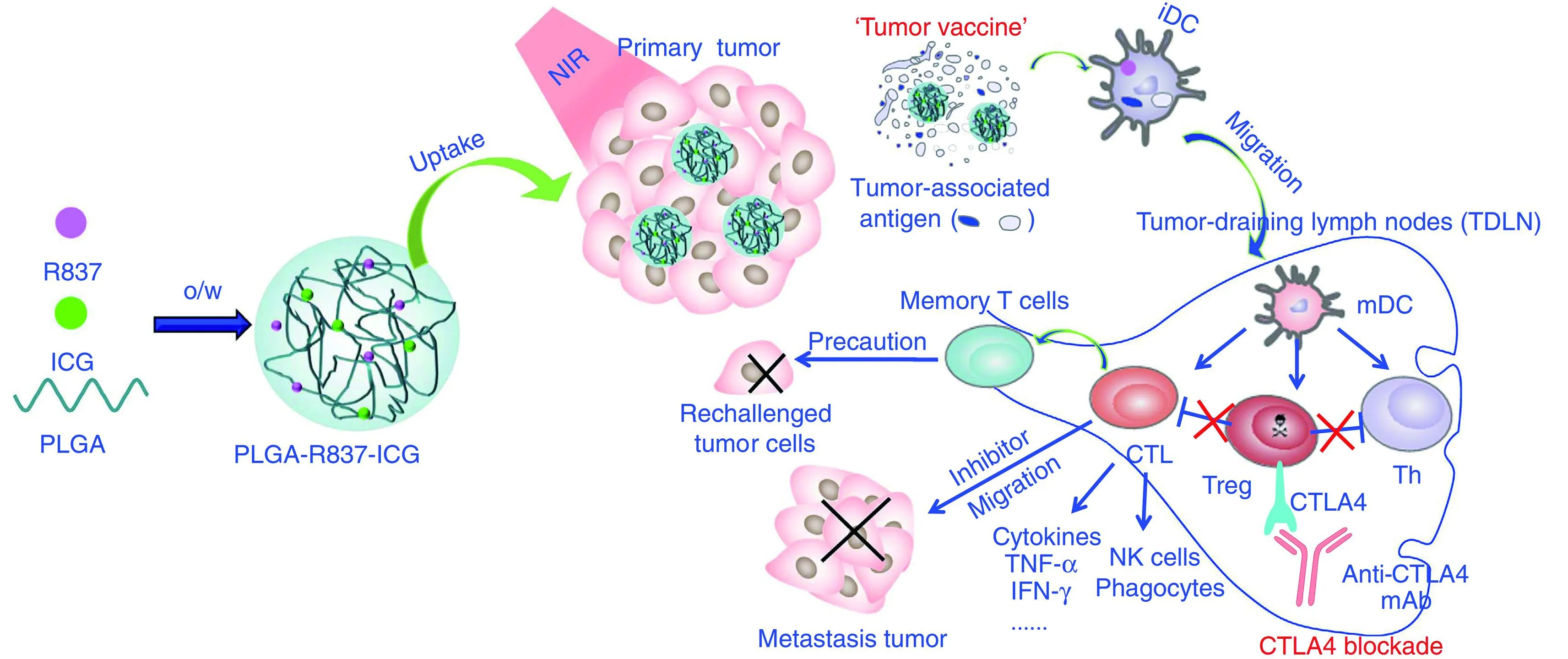
Figure 6 Mechanism of anti-tumor immune responses induced by PLGA-ICG-R837-based PTT in combination with checkpoint-blockade. Reproduced with permission from Ref. 71.
Diagnosis and PTT
The early detection or diagnosis of disease and the precise monitoring of therapeutic effects on lesions after treatment are critical to improve the effectiveness of cancer treatment. Combined diagnosis and treatment has become an important cancer therapy strategy. Liu et al.76prepared ultrasmall Cu3BiS3nanodots (NDs), single-phased ternary bimetal sulfide nanomaterials that are powerful, degradable, and safe nanomedicine for PTT-guided MSOT and X-ray CT. The authors demonstrated that Cu3BiS3NDs could be quickly degraded through renal clearance. The metabolic behavior of NDs, which have low toxicity, from biological and chemical aspects was monitored through CT and X-ray absorption near-edge spectroscopy. Moon et al.77reported a system of reduced graphene oxide-coated gold nanorods (r-GOAuNRs) which has a strongly amplified photoacoustic (PA) performance provided by the excellent NIR light absorption and photothermal stability of the reduced graphene oxide layer. Chen et al.78proposed a nanosystem composed of human serum albumin (HSA), PTX, and ICG; this system can self-assemble into stable nanoparticles. ICG acts as a photothermal agent and a fluorescence imaging probe. The obtained HSA-ICG-PTX nanoparticles have good stability and long circulation. The heat generated by ICG under NIR laser irradiation promotes the uptake of HSA-ICG-PTX nanoparticles and tumor cell death.
Wang et al.79designed a Gd-hybridized plasmonic Aunanocomposite system, where citrate-Gd complexes and DOX are co-loaded on mesoporous silica-coated AuNR. Under NIR laser irradiation, the mild heat produced by nanoparticles enhances circulation and targets drug delivery to the tumor site. The nanocomposite materials promote five imaging or analysis techniques: tumor diagnosis by CT and MRI, therapeutic responses by PA imaging, synchrotron radiation (SR), X-ray fluorescence mapping, and SR scanning-transmission X-ray microscopy imaging. Yang et al.80developed a polymer micelle system for dual NIR fluorescence imaging and the PTT of tumors. The copolymers, which consist of monomethoxy poly (ethylene glycol) and alkylamine-grafted poly (L-aspartic acid), form theranostic micelles by assembly with carbocyanine dyes. Given their small size, high loading capacity, good stability, and sustained release, the micelles can enhance the cellular uptake of micelles and achieve better biological distribution and the long-term retention of cyanine dye in the tumor site, thus enhancing NIR fluorescence imaging. In addition, the stability of subcellular organelles is destroyed under photoirradiation, resulting in severe photothermal damage to cancer cells.
Conclusions and perspectives
More and more nanoparticles tuned for diverse nanomedicine applications have emerged, thus suggesting the potential development of multifunctional “smart”nanoparticle drug delivery systems that may facilitate individualized cancer therapy. Various types of nanoparticles have been evaluated for their suitability for simultaneous in vivo imaging and the treatment of cancers with improved efficacy.
Although nanoparticles have raised exciting expectations for cancer diagnosis and treatment, challenges continue to exist and arise, especially in achieving practical application inliving organisms. Nevertheless, current research studies are closer than ever to solving these issues and achieving practical nanotherapy for cancer. Prospective directions for the development in this field include the specific accumulation of nanoparticles solely in malignant cells; the real-time imaging and monitoring of treatment effects in vivo; and killing the cancer cells with minimal side effects by sparing normal cells.
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Panyam J, Labhasetwar V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv Drug Deliv Rev. 2003; 55: 329-47.
2.Davis ME, Chen Z, Shin DM. Nanoparticle therapeutics: An emerging treatment modality for cancer. Nat Rev Drug Discovery. 2008; 7: 771-82.
3.Brannon-Peppas L, Blanchette JO. Nanoparticle and targeted systems for cancer therapy. Adv Drug Deliv Rev. 2004; 56: 1649-59.
4.Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf B Biointerfaces. 2010; 75: 1-18.
5.Rivera E. Current status of liposomal anthracycline therapy in metastatic breast cancer. Clin Breast Cancer. 2003; 4 Suppl 2: S76-83.
6.Manchester M, Singh P. Virus-based nanoparticles (VNPs): Platform technologies for diagnostic imaging. Adv Drug Deliv Rev. 2006; 58: 1505-22.
7.Ghosh P, Han G, De M, Kim CK, Rotello VM. Gold nanoparticles in delivery applications. Adv Drug Deliv Rev. 2008; 60: 1307-15.
8.Mornet S, Vasseur S, Grasset F, Duguet E. Magnetic nanoparticle design for medical diagnosis and therapy. J Mater Chem. 2004; 14: 2161-75.
9.Larsen AK, Escargueil AE, Skladanowski A. Resistance mechanisms associated with altered intracellular distribution of anticancer agents. Pharmaco Ther. 2000; 85: 217-29.
10.Wilhelm S, Tavares AJ, Dai Q, Ohta S, Audet J, Dvorak HF, et al. Analysis of nanoparticle delivery to tumours. Nat Rev Mater. 2016; 1: 16014
11.Pelaz B, Alexiou C, Alvarez-Puebla RA, Alves F, Andrews AM, Ashraf S, et al. Diverse applications of nanomedicine. ACS Nano. 2017; 11: 2313-81.
12.Park JH, Gu L, Von Maltzahn G, Ruoslahti E, Bhatia SN, Sailor MJ. Biodegradable luminescent porous silicon nanoparticles for in vivo applications. Nat Mat. 2009; 8: 331-6.
13.Mundra V, Peng Y, Rana S, Natarajan A, Mahato RI. Micellar formulation of indocyanine green for phototherapy of melanoma. J Control Release. 2015; 220: 130-40.
14.Yu PC, Yu HJ, Guo CY, Cui ZR, Chen XZ, Yin Q, et al. Reversal of doxorubicin resistance in breast cancer by mitochondria-targeted pH-responsive micelles. Acta Biomater. 2015; 14: 115-24.
15.Lee ES, Kim JH, Sim T, Youn YS, Lee BJ, Oh YT, et al. A feasibility study of a ph sensitive nanomedicine using doxorubicin loaded poly (aspartic acid-graft-imidazole)-block-poly (ethylene glycol) micelles. J Mater Chem B. 2014; 2: 1152-9.
16.Talelli M, Iman M, Varkouhi AK, Rijcken CJ, Schiffelers RM, Etrych T, et al. Core-crosslinked polymeric micelles with controlled release of covalently entrapped doxorubicin. Biomaterials. 2010; 31: 7797-804.
17.Zhang WJ, Wang FH, Wang Y, Wang JN, Yu YN, Guo SR, et al. Ph and near-infrared light dual-stimuli responsive drug delivery using DNA-conjugated gold nanorods for effective treatment of multidrug resistant cancer cells. J Control Release. 2016; 232: 9-19.
18.Jia HZ, Zhu JY, Wang XL, Cheng H, Chen G, Zhao YF, et al. A boronate-linked linear-hyperbranched polymeric nanovehicle for pH-dependent tumor-targeted drug delivery. Biomaterials. 2014; 35: 5240-9.
19.Torres E, Mainini F, Napolitano R, Fedeli F, Cavalli R, Aime S, et al. Improved paramagnetic liposomes for MRI visualization of pH triggered release. J Control Release. 2011; 154: 196-202.
20.Seib FP, Jones GT, Rnjak-Kovacina J, Lin YN, Kaplan DL. pH-dependent anticancer drug release from silk nanoparticles. Adv Healthc Mater. 2013; 2: 1606-11.
21.Battogtokh G, Ko YT. Self-assembling micelle-like nanoparticles with detachable envelopes for enhanced delivery of nucleic acid therapeutics. Mol Pharmaceutics. 2014; 11: 904-12.
22.Van Butsele K, Sibret P, Fustin CA, Gohy JF, Passirani C, Benoit JP, et al. Synthesis and pH-dependent micellization of diblock copolymer mixtures. J Colloid Interf Sci. 2009; 329: 235-43.
23.Lv SN, Cheng CJ, Song YY, Zhao ZG. Temperature-switched controlled release nanosystems based on molecular recognition and polymer phase transition. RSC Adv. 2015; 5: 3248-59.
24.Talelli M, Rijcken CJF, Lammers T, Seevinck PR, Storm G, Van Nostrum CF, et al. Superparamagnetic iron oxide nanoparticles encapsulated in biodegradable thermosensitive polymeric micelles: Toward a targeted nanomedicine suitable for image-guided drug delivery. Langmuir. 2009; 25: 2060-7.
25.Liu J, Zheng XP, Yan L, Zhou LJ, Tian G, Yin WY, et al. Bismuth sulfide nanorods as a precision nanomedicine for in vivo multimodal imaging-guided photothermal therapy of tumor. ACS Nano. 2015; 9: 696-707.
26.Mi Y, Wolfram J, Mu CF, Liu XW, Blanco E, Shen HF, et al. Enzyme-responsive multistage vector for drug delivery to tumor tissue. Pharmacol Res. 2016; 113: 92-9.
27.Tang R, Kim CS, Solfiell DJ, Rana S, Mout R, Velázquez-Delgado EM, et al. Direct delivery of functional proteins and enzymes to the cytosol using nanoparticle-stabilized nanocapsules. ACS Nano. 2013; 7: 6667-73.
28.Barve A, Jain A, Liu H, Jin W, Cheng K. An enzyme-responsive conjugate improves the delivery of a pi3k inhibitor to prostate cancer. Nanomed: Nanotechnol, Biol Med. 2016; 12: 2373-81.
29.Ruan SB, Cao X, Cun XL, Hu GL, Zhou Y, Zhang YJ, et al. Matrixmetalloproteinase-sensitive size-shrinkable nanoparticles for deep tumor penetration and ph triggered doxorubicin release. Biomaterials. 2015; 60: 100-10.
30.Yu HL, Chen J, Liu S, Lu Q, He J, Zhou ZY, et al. Enzyme sensitive, surface engineered nanoparticles for enhanced delivery of camptothecin. J Control Release. 2015; 216: 111-20.
31.Ding BY, Zhang W, Wu X, Wang J, Xie C, Huang X, et al. Dr5 mab-conjugated, dtic-loaded immuno-nanoparticles effectively and specifically kill malignant melanoma cells in vivo. Oncotarget. 2016; 7: 57160-70.
32.Saraf P, Li XL, Wrischnik L, Jasti B. In vitro and in vivo efficacy of self-assembling rgd peptide amphiphiles for targeted delivery of paclitaxel. Pharm Res. 2015; 32: 3087-101.
33.Carregal-Romero S, Guardia P, Yu X, Hartmann R, Pellegrino T, Parak WJ. Magnetically triggered release of molecular cargo from iron oxide nanoparticle loaded microcapsules. Nanoscale. 2015; 7: 570-6.
34.Fang JH, Lee YT, Chiang WH, Hu SH. Magnetoresponsive virusmimetic nanocapsules with dual heat-triggered sequential-infected multiple drug-delivery approach for combinatorial tumor therapy. Small. 2015; 11: 2417-28.
35.Kuo CY, Liu TY, Chan TY, Tsai SC, Hardiansyah A, Huang LY, et al. Magnetically triggered nanovehicles for controlled drug release as a colorectal cancer therapy. Colloids Surf B Biointerf. 2016; 140: 567-73.
36.Lee JH, Chen KJ, Noh SH, Garcia MA, Wang H, Lin WY, et al. Ondemand drug release system for in vivo cancer treatment through self-assembled magnetic nanoparticles. Angew Chem Int Ed Engl. 2013; 52: 4384-8.
37.Li JB, Qu Y, Ren J, Yuan WZ, Shi DH. Magnetocaloric effect in magnetothermally-responsive nanocarriers for hyperthermiatriggered drug release. Nanotechnology. 2012; 23: 505706
38.Cheng YH, Cheng H, Jiang CX, Qiu XF, Wang KK, Huan W, et al. Perfluorocarbon nanoparticles enhance reactive oxygen levels and tumour growth inhibition in photodynamic therapy. Nat Commun. 2015; 6: 8785
39.Gong H, Chao Y, Xiang J, Han X, Song GS, Feng LZ, et al. Hyaluronidase to enhance nanoparticle-based photodynamic tumor therapy. Nano Lett. 2016; 16: 2512-21.
40.Hou BB, Zheng B, Yang WT, Dong CH, Wang HJ, Chang J. Construction of near infrared light triggered nanodumbbell for cancer photodynamic therapy. J Colloid Interface Sci. 2017; 494: 363-72.
41.Patel K, Raj BS, Chen Y, Lou X. Novel folic acid conjugated Fe3O4-zno hybrid nanoparticles for targeted photodynamic therapy. Colloids Surf B Biointerf. 2017; 150: 317-25.
42.Usacheva M, Swaminathan SK, Kirtane AR, Panyam J. Enhanced photodynamic therapy and effective elimination of cancer stem cells using surfactant-polymer nanoparticles. Mol Pharmceutics. 2014; 11: 3186-95.
43.Chen CW, Lee PH, Chan YC, Hsiao M, Chen CH, Wu PC, et al. Plasmon-induced hyperthermia: Hybrid upconversion NaYF4: Yb/er and gold nanomaterials for oral cancer photothermal therapy. J Mater Chem B. 2015; 3: 8293-302.
44.Yang D, Yang GX, Wang XM, Lv RC, Gai SL, He F, et al. Y2O3: Yb, Er@mSiO2-CuxS double-shelled hollow spheres for enhanced chemo-/photothermal anti-cancer therapy and dual-modal imaging. Nanoscale. 2015; 7: 12180-91.
45.Sun MM, Peng D, Hao HJ, Hu J, Wang DL, Wang K, et al. Thermally triggered in situ assembly of gold nanoparticles for cancer multimodal imaging and photothermal therapy. ACS Appl Mater Interfaces. 2017; 9: 10453-60.
46.Sweeney EE, Burga RA, Li CY, Zhu Y, Fernandes R. Photothermal therapy improves the efficacy of a mek inhibitor in neurofibromatosis type 1-associated malignant peripheral nerve sheath tumors. Sci Rep. 2016; 6: 37035
47.Yu YX, Xu S, You H, Zhang YJ, Yang B, Sun XY, et al. In vivo synergistic anti-tumor effect of paclitaxel nanoparticles combined with radiotherapy on human cervical carcinoma. Drug Deliv. 2017; 24: 75-82.
48.Satterlee AB, Rojas JD, Dayton PA, Huang L. Enhancing nanoparticle accumulation and retention in desmoplastic tumors via vascular disruption for internal radiation therapy. Theranostics. 2017; 7: 253-69.
49.Zhang HL, Zhang W, Zhou Y, Jiang YH, Li SP. Dual functional mesoporous silicon nanoparticles enhance the radiosensitivity of vpa in glioblastoma. Transl Oncol. 2017; 10: 229-40.
50.Song L, Falzone N, Vallis KA. Egf-coated gold nanoparticles provide an efficient nano-scale delivery system for the molecular radiotherapy of egfr-positive cancer. Int J Radiat Biol. 2016; 92: 716-23.
51.Song GS, Ji CH, Liang C, Song XJ, Yi X, Dong ZL, et al. Taox decorated perfluorocarbon nanodroplets as oxygen reservoirs to overcome tumor hypoxia and enhance cancer radiotherapy. Biomaterials. 2017; 112: 257-63.
52.Wang DX, Luo WX, Wen G, Yang L, Hong SF, Zhang SY, et al. Synergistic effects of negative-charged nanoparticles assisted by ultrasound on the reversal multidrug resistance phenotype in breast cancer cells. Ultrason Sonochem. 2017; 34: 448-57.
53.Sviridov AP, Osminkina LA, Kharin AY, Gongansky MB, Kargina JV, Kudryavtsev AA, et al. Cytotoxicity control of silicon nanoparticles by biopolymer coating and ultrasound irradiation for cancer theranostic applications. Nanotechnology. 2017; 28: 105102
54.Brazzale C, Canaparo R, Racca L, Foglietta F, Durando G, Fantozzi R, et al. Enhanced selective sonosensitizing efficacy of ultrasoundbased anticancer treatment by targeted gold nanoparticles. Nanomedicine. 2016; 11: 3053-70.
55.Qiu WX, Liu LH, Li SY, Lei Q, Luo GF, Zhang XZ. Acpi conjugated gold nanorods as nanoplatform for dual image guided activatable photodynamic and photothermal combined therapy in vivo. Small. 2017; doi: 10.1002/smll.201603956.
56.Guo M, Mao HJ, Li YL, Zhu AJ, He H, Yang H, et al. Dual imagingguided photothermal/photodynamic therapy using micelles. Biomaterials. 2014; 35: 4656-66.
57.Zhu XL, Huang HQ, Zhang YJ, Zhang HJ, Hou L, Zhang ZZ. Cit/CuS@Fe3O4-based and enzyme-responsive magneticnanoparticles for tumor chemotherapy, photothermal, and photodynamic therapy. J Biomater Appl. 2017; 31: 1010-25.
58.Sun JJ, Guo Y, Xing RR, Jiao TF, Zou QL, Yan XH. Synergistic in vivo photodynamic and photothermal antitumor therapy based on collagen-gold hybrid hydrogels with inclusion of photosensitive drugs. Colloids Surf A: Physicochem and Eng Asp. 2017; 514: 155-60.
59.Sun Q, You Q, Pang XJ, Tan XX, Wang JP, Liu L, et al. A photoresponsive and rod-shape nanocarrier: Single wavelength of light triggered photothermal and photodynamic therapy based on AuNRs-capped & Ce6-doped mesoporous silica nanorods. Biomaterials. 2017; 122: 188-200.
60.Wang Y, Wang KY, Zhao JF, Liu XG, Bu J, Yan XY, et al. Multifunctional mesoporous silica-coated graphene nanosheet used for chemo-photothermal synergistic targeted therapy of glioma. J Am Chem Soc. 2013; 135: 4799-804.
61.Shao LH, Zhang RR, Lu JQ, Zhao CY, Deng XW, Wu Y. Mesoporous silica coated polydopamine functionalized reduced graphene oxide for synergistic targeted chemo-photothermal therapy. ACS Appl Mater Interfaces. 2017; 9: 1226-36.
62.Gao H, Bi Y, Chen J, Peng LR, Wen KK, Ji P, et al. Near-infrared light-triggered switchable nanoparticles for targeted chemo/photothermal cancer therapy. ACS Appl Mater Interfaces. 2016; 8: 15103-12.
63.Meng ZQ, Wei F, Wang RH, Xia MG, Chen ZG, Wang HP, et al. NIR-laser-switched in vivo smart nanocapsules for synergic photothermal and chemotherapy of tumors. Adv Mater. 2016; 28: 245-53.
64.Shen S, Tang HY, Zhang XT, Ren JF, Pang ZQ, Wang DG, et al. Targeting mesoporous silica-encapsulated gold nanorods for chemo-photothermal therapy with near-infrared radiation. Biomaterials. 2013; 34: 3150-8.
65.Feng QH, Zhang YY, Zhang WX, Hao YW, Wang YC, Zhang HL, et al. Programmed near-infrared light-responsive drug delivery system for combined magnetic tumor-targeting magnetic resonance imaging and chemo-phototherapy. Acta Biomater. 2017; 49: 402-13.
66.He CB, Duan XP, Guo NN, Chan C, Poon C, Weichselbaum RR, et al. Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockade cancer immunotherapy. Nat Commun. 2016; 7: 12499
67.Dong CH, Liu ZY, Wang S, Zheng B, Guo WS, Yang WT, et al. A protein-polymer bioconjugate-coated upconversion nanosystem for simultaneous tumor cell imaging, photodynamic therapy, and chemotherapy. ACS Appl Mater Interfaces. 2016; 8: 32688-98.
68.Ai FJ, Sun TY, Xu ZF, Wang ZG, Kong W, To MW, et al. An upconversion nanoplatform for simultaneous photodynamic therapy and pt chemotherapy to combat cisplatin resistance. Dalton Trans. 2016; 45: 13052-60.
69.Chen GJ, Jaskula-Sztul R, Esquibel CR, Lou I, Zheng QF, Dammalapati A, et al. Neuroendocrine tumor-targeted upconversion nanoparticle-based micelles for simultaneous NIR-controlled combination chemotherapy and photodynamic therapy, and fluorescence imaging. Adv Funct Mat. 2017; 27: 1604671
70.Feng XF, Jiang D, Kang T, Yao JH, Jing YX, Jiang TZ, et al. Tumorhoming and penetrating peptide-functionalized photosensitizerconjugated peg-pla nanoparticles for chemo-photodynamic combination therapy of drug-resistant cancer. ACS Appl Mater Interfaces. 2016; 8: 17817-32.
71.Chen Q, Xu LG, Liang C, Wang C, Peng R, Liu Z. Photothermal therapy with immune-adjuvant nanoparticles together with checkpoint blockade for effective cancer immunotherapy. Nat Commun. 2016; 7: 13193
72.Shi GN, Zhang CN, Xu R, Niu JF, Song HJ, Zhang XY, et al. Enhanced antitumor immunity by targeting dendritic cells with tumor cell lysate-loaded chitosan nanoparticles vaccine. Biomaterials. 2017; 113: 191-202.
73.Zhen ZP, Tang W, Wang MZ, Zhou SY, Wang H, Wu ZH, et al. Protein nanocage mediated fibroblast-activation protein targeted photoimmunotherapy to enhance cytotoxic T cell infiltration and tumor control. Nano Lett. 2017; 17: 862-9.
74.Cano-Mejia J, Burga RA, Sweeney EE, Fisher JP, Bollard CM, Sandler AD, et al. Prussian blue nanoparticle-based photothermal therapy combined with checkpoint inhibition for photothermal immunotherapy of neuroblastoma. Nanomed: Nanotechnol, Biol Med. 2017; 13: 771-81.
75.Huo MR, Zhao Y, Satterlee AB, Wang YH, Xu Y, Huang L. Tumortargeted delivery of sunitinib base enhances vaccine therapy for advanced melanoma by remodeling the tumor microenvironment. J Control Release. 2017; 245: 81-94.
76.Liu J, Wang PY, Zhang X, Wang LM, Wang DL, Gu ZJ, et al. Rapid degradation and high renal clearance of Cu3BiS3nanodots for efficient cancer diagnosis and photothermal therapy in vivo. ACS Nano. 2016; 10: 4587-98.
77.Moon H, Kumar D, Kim H, Sim C, Chang JH, Kim JM, et al. Amplified photoacoustic performance and enhanced photothermal stability of reduced graphene oxide coated gold nanorods for sensitive photo acoustic imaging. ACS Nano. 2015; 9: 2711-9.
78.Chen Q, Liang C, Wang C, Liu Z. An imagable and photothermal "abraxane-like" nanodrug for combination cancer therapy to treat subcutaneous and metastatic breast tumors. Adv Mater. 2015; 27: 903-10.
79.Wang J, Liu J, Liu Y, Wang LM, Cao MJ, Ji YL, et al. Gd-hybridized plasmonic au-nanocomposites enhanced tumor-interior drug permeability in multimodal imaging-guided therapy. Adv Mater. 2016; 28: 8950-8.
80.Yang H, Mao HJ, Wan ZH, Zhu AJ, Guo M, Li YL, et al. Micelles assembled with carbocyanine dyes for theranostic near-infrared fluorescent cancer imaging and photothermal therapy. Biomaterials. 2013; 34: 9124-33.
Cite this article as: Xin Y, Yin M, Zhao L, Meng F, Luo L. Recent progress on nanoparticle-based drug delivery systems for cancer therapy. Cancer Biol Med. 2017; 14: 228-41. doi: 10.20892/j.issn.2095-3941.2017.0052
Liang Luo
E-mail: liangluo@hust.edu.cn
April 29, 2017; accepted May 24, 2017.
Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年3期
Cancer Biology & Medicine2017年3期
- Cancer Biology & Medicine的其它文章
- Survival after pulmonary metastasectomy in colorectal cancer patients: does a history of resected liver metastases worsen the prognosis? A literature review
- Expression levels of β-catenin and galectin-3 in meningioma and their effect on brain invasion and recurrence: a tissue microarray study
- Potential predictive factors for pathologic complete response after the neoadjuvant treatment of rectal adenocarcinoma: a single center experience
- Inhibition of IKK-NFκB pathway sensitizes lung cancer cell lines to radiation
- BsmI (rs1544410) and FokI (rs2228570) vitamin D receptor polymorphisms, smoking, and body mass index as risk factors of cutaneous malignant melanoma in northeast Italy
- Preclinical and clinical applications of specific molecular imaging for HER2-positive breast cancer
