Transitional care interventions to reduce readmission in patients with chronic obstructive pulmonary disease:A meta-analysis of randomized controlled trials
Min Liu,Yng Zhng,Dn-Dn Li,Jing Sun
aDepartment of Nursing,Yancheng City No.1 People Hospital,Yancheng,Jiangsu 224000,China
bCollege of Nursing,Southeast University,Nanjing,Jiangsu 210009,China
cCollege of Nursing,Nanjing University of Traditional Chinese Medicine,Nanjing,Jiangsu 210000,China
Transitional care interventions to reduce readmission in patients with chronic obstructive pulmonary disease:A meta-analysis of randomized controlled trials
Min Liua,*,Yang Zhangb,Dan-Dan Lic,Jing Suna
aDepartment of Nursing,Yancheng City No.1 People Hospital,Yancheng,Jiangsu 224000,China
bCollege of Nursing,Southeast University,Nanjing,Jiangsu 210009,China
cCollege of Nursing,Nanjing University of Traditional Chinese Medicine,Nanjing,Jiangsu 210000,China
A R T I C L EI N F O
Article history:
25 January 2017
Accepted 27 March 2017
Available online 7 June 2017
Transitional care
Meta-analysis
Patient readmission
Obstructive pulmonary disease
Chronic
Objective:To objectively assess the effect of transitional care on readmission for patients with chronic obstructive pulmonary disease.
Methods:The PubMed,Science Direct,Web of Science,Cochrane Library,CNKI,and Wanfang databases were searched for relevant randomized controlled trials(RCTs)published from January 1990 through April 2016.The quality of eligible studies was assessed by two investigators.The primary outcome assessed was readmission for COPD and all-cause readmission.The pooled effect sizes were expressed as the relative risk and standard mean difference with 95%con fi dence intervals.Heterogeneity among studies was assessed using the Cochrane Handbook for Systematic Reviews of Interventions(Version 5.1.0)and determined with an I2statistic.
Results:A total of seven RCTs that included 1879 participants who met the inclusion criteria were analyzed.The results of subgroup analysis showed signi fi cant differences in readmission for COPD at the 6 month and 18 month time points and all-cause readmission at the 18 month follow-up.Transitional care could reduce readmission for COPD at the 6 month[RR=0.51,95%CI(0.38,0.68),P<0.00001]and 18 month time points[RR=0.56,95%CI(0.45,0.69),P<0.00001,and also reduce all-cause readmission after 18 months[RR=0.72,95%CI(0.62,0.84),P<0.0001].The reduction of all-cause readmission between the intervention and control groups in the 2nd year,however,was less than that in the 1st year.Conclusions:Transitional care is bene fi cial to reducing readmission for patients with COPD.Duration of≥6 and≤18 months are more effective,and the effect weakens over intervention time,especially after the end of intervention.Both durations point to the importance of ongoing intervention and reinforcement after the end of intervention.
©2017 Shanxi Medical Periodical Press.Publishing services by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Chronic obstructive pulmonary disease(COPD)is a common disease worldwide that is characterized by chronic air fl ow limitation and a range of pathological changes in the lung,some heavy extra-pulmonary effects,and important comorbidities that may contribute to the severity of the disease in individual patients.1It has been estimated that COPD will be the third leading cause of death worldwide by 2030.2
Readmissions are a signi fi cant source of morbidity and a heavy healthcare burden.According to statistics,readmission among elderly patients with COPD costs approximately$924 million annually.3Unplanned readmission for COPD has exhibited an upwardyearlytrend,occurringin almostone in fi ve discharges among older adults.4The reasons for readmission of COPD patients are complex and include frequent acute exacerbations,coexisting comorbidities,and lack of transitional care.5
Nurses and other healthcare providers,as a part of a multidisciplinary team,can play a key role in COPD care by developing an individualized needs-based comprehensive discharge plan,connecting patients and outpatient providers,providing educational and behavioral interventions,managing symptoms and providing direct patient care,monitoring patients and caregivers regularly throughhomevisitsand/ortelephonecontact,providingcounseling and self-care instruction,and reviewing and managing medications during transitions from one setting to another,especially from the hospital to home.For example,discharged patients with COPD may present with severe breathlessness,expectoration and chronic productive cough,6and they may not be aware of their worsening status or the necessityof awareness of self-care,ongoing monitoring,and care coordination.As a result,they require professional education to identify risks,especially in the selfassessment of the acute exacerbated stage of COPD signs and symptoms as well as adherence to self-care maintenance recommendations.Transitional care executors play a critical role in narrowing these potential gaps when transitioning COPD patients from one care setting to another.
Regardingtheeffectoftransitionalcareonreadmissionreduction, there have been many studies on the relationship between transitional-caremodelsandthereadmissionreductioneffectamong patients with COPD,but the results of different trials have not been consistent.7Therefore,theaimof thisreviewistostudy theeffectsof transitional-care models on readmission reduction for patients with COPD moving from the hospital to home and to provide guidance to transitional care providers in developing and implementing appropriate processes that may promote a reduction in readmissions.
2.Methods
2.1.Search strategies
A research librarian was consulted to search for and identify articles related to our study.The PubMed,Science Direct,Web of Science,Cochrane Library,China National KnowledgeInfrastructure (CNKI),and Wan-fang databases were searched.The PubMed search was conducted using the following algorithm:[(Transitional care[MesH]OR Transition*care[tw]OR care transition[tw]OR transition after hospitalization[tw]OR transition for COPD patients [tw]OR transition interventions[tw])OR(“Continuity of Patient Care”[MesH]OR(continuum of care[tw]OR care continuum[tw])) OR(Patient Care Planning[MesH])]AND(Pulmonary Disease, Chronic Obstructive[MesH]OR COPD[MesH])AND(Patient Readmission[MesH]OR Patient Admission[MesH]OR readmission [tw]).Other databases were searched using a similar search strategy.In PubMed,we conducted searches in all fi elds and identi fi ed 101 articles.In other databases,we conducted searches in the title/ abstract/keyword fi elds and identi fi ed 145 articles from Science Direct;163 from Web of Science;97 from the Cochrane Library;56 from CNKI;and 41 from the Wanfang Database.Searches were limited to English language articles published from January 1990 through April 2016.Articles had to include patients with COPD exclusively and have at least 1 transition component from one setting to another.In addition,the reference lists and academic conference literature were manually searched,and experts in the clinical nursing fi eld were consulted to locate additional studies.
The literature search consisted of four steps:(1)Searches of systematic literature studies relevant to COPD transition were conducted in the Cochrane and JBI libraries;(2)The titles,abstracts, keywords and subjects of original articles retrieved from PubMed, Science Direct and Web of Sciencewere analyzed to further con fi rm retrieval of keywords and subjects;(3)relevant databases were searched by keywords and subjects,and full-text articles whose abstracts met the inclusion criteria were retrieved;and(4)references from the obtained articles were further retrieved.
2.2.Inclusion criteria and study selection
Studies were included if they met the following criteria:(1) Patients who reached the age of 18 were diagnosed with COPD, patients in the intervention group who accepted post-discharge transitional care,and other patients in the control group who accepted usual care without post-discharge transitional care;patients with asthma as a primary diagnosis and with major comorbidities(e.g.,serious heart failure,malignant or terminal disease) were excluded as were patients with dementia or uncontrolled psychiatric illness.(2)The interventions in the articles included in this review were:patient situation and homecare needs assessment before discharge;after discharge,a speci fi c transition executor provided individual care to patients with COPD by telephone and/or home visit.Patients could also contact the executor for further information during the intervention period.(3)The outcomes in the studies were classi fi ed as readmissions for COPD and all-cause readmissions.
Fig.1 shows the selection process for the fi nal 7 articles for this review.Anadditional136additionalfull-textarticleswere excluded:73 articles with incomplete readmission data,29 articles with incomplete intervention group/control group(IG/CG)data, and 34 articles for other reasons.We originally retrieved these articles for meta-analysis between January 1990 and April 2016,and all of the articles investigated readmission as an outcome of transitional care for patients with COPD.
2.3.Data extraction and quality assessment
Data from the 7 studies were extracted by one of the two reviewers(Liu)with a standard data extraction form.All of the data extracted from these studies were checked by the other reviewer (Zhang).We adopted the Cochrane Handbook for Systematic Reviews of Interventions(Version 5.1.0)8to assess the risk of bias, which includes six domains:selection bias,performance bias, detection bias,attrition bias,reporting bias and other bias.Two reviewers(Liu and Zhang)assessed each study independently and consulted in the case of disagreements,all of which were then resolved by consensus.
2.4.Statistical method
Software Review Manager version 5.3 was used to conduct statistical analysis.The heterogeneity between studies was evaluated by the I2test.If I2<50%,the possibility of heterogeneity between studies was low and the fi xed effect model could be utilized. If I2>50%,there was heterogeneity between studies and the sources of heterogeneity should be analyzed.The criteria for signi fi cance were P<0.05 and 95%CI not including 0.
3.Results
3.1.Systematic review
3.1.1.Characteristics of the selected studies
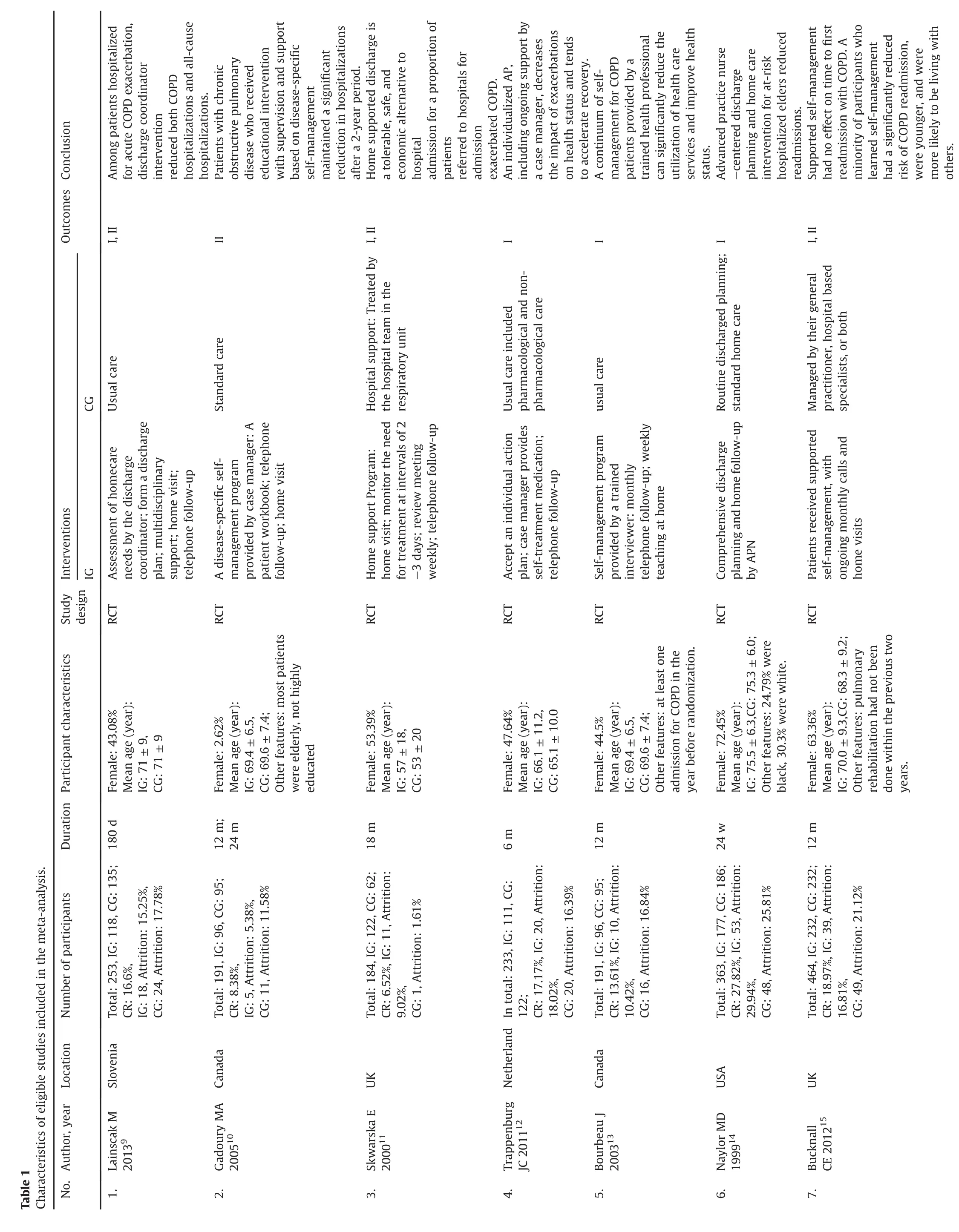
Seven articles identi fi ed as part of the systematic literature searches are summarized in Fig.1.Based on a thorough review of this literature,7 articles9-15in the review included a total of 1879 participants.Table 1 presents the characteristics and pulmonary functions.The number of participants of each study ranged from 18411to 464.15All participants had COPD.In these studies,the mean age was over 65 years old.In 2 studies,11,15the participants were British,2 other studies10,13reported that the participants were Canadian,and 3 further studies reported9,12,14adult participants from Slovenia,the Netherlands and the United States.The intervention duration ranged from 6 months9,12,14to 24 months.10One study10had more than one follow-up interval that ranged from 12 to 24 months.Six studies9,11-15investigated readmissions for COPD, and 4 studies9-11,15investigated all-cause readmissions.Onestudy10investigated the number of hospitalizations,and the other 6 studies9,11-15investigated the number of readmitted patients.The details of intervention in IG and CG can be found in Table 1.
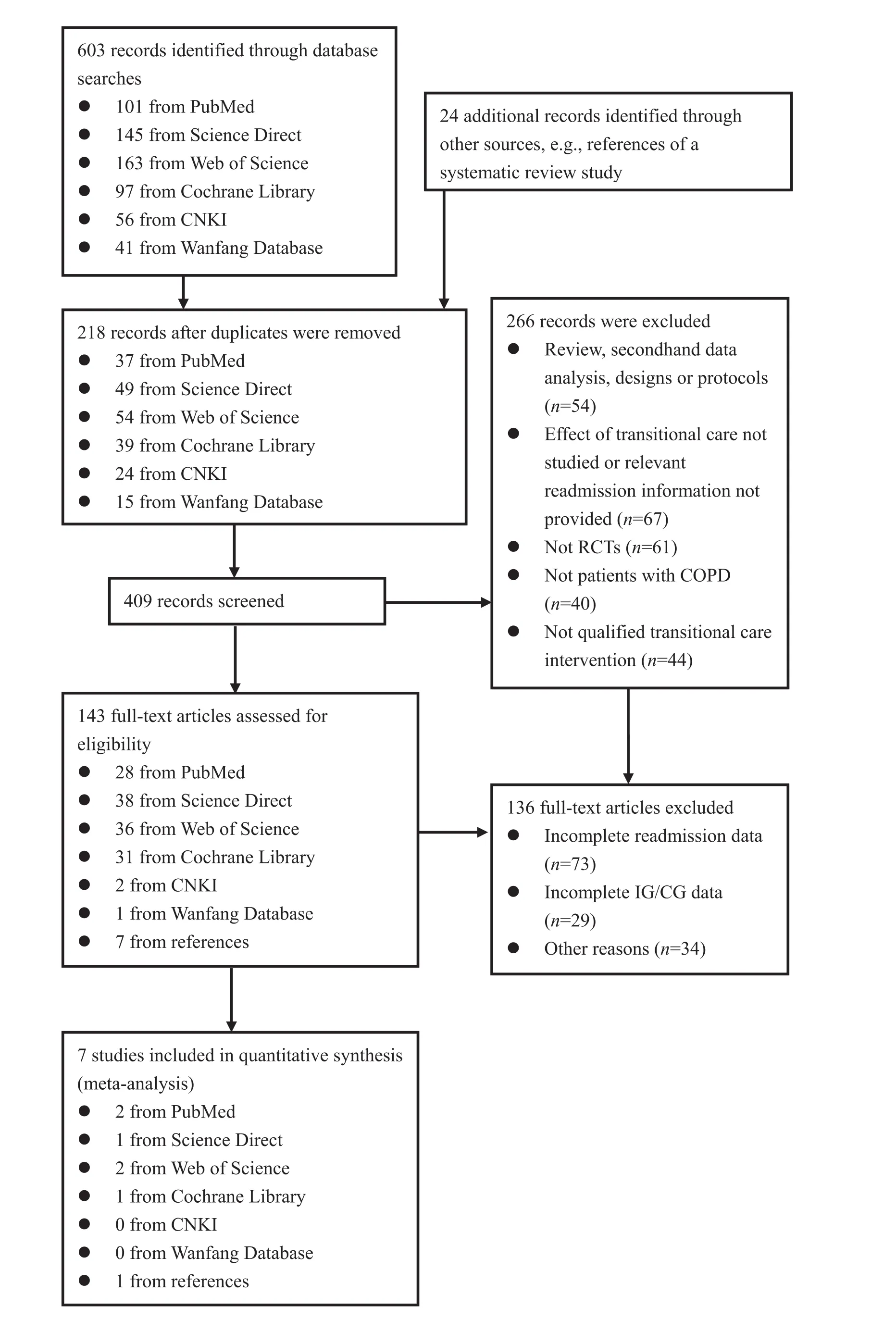
Fig.1.Flowchart of the study selection.
3.2.Meta-analyses
3.2.1.Risk of bias
All 7 studies included in this meta-analysis were RCTs,but only one study12reported blinding of participants.The individual quality of most studies revealed a low bias risk in most domains, and all of the studies were judged to have a high risk of bias in at least one domain(Fig.2).Six studies presented approved random sequence generation,9,11-15and fi ve presented allocation concealment.9,11-13,15No study reported blinding of outcome assessment,but fi ve studies reported incomplete outcome data.9,10,13-15Two studies reported a selective reporting bias,9,15and two studies seemed to be free from other risks of bias.11,15Finally,after discussion with a third author,the agreement was 100%.
3.2.2.Overall results of the transitional care effect
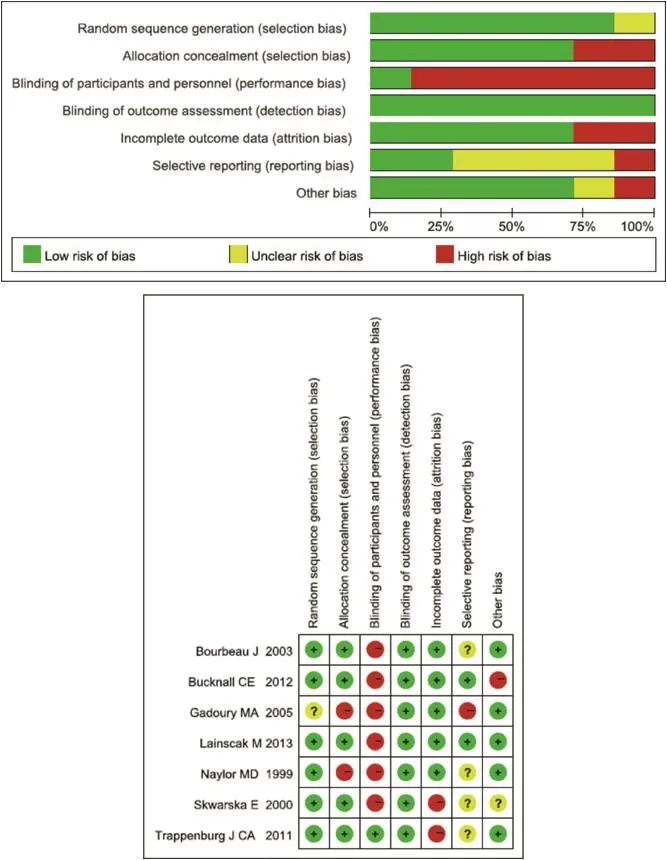
Fig.2.Risk of bias graph.
All 7 studies provided related data of readmission as the outcome measure of transitional care intervention effect.In 6 studies,9,11-15we used readmission for COPD to represent the effect ofintervention,andin3studies,9,11,15weusedall-causereadmissiontorepresenttheeffectofintervention.Three studies,9,12,14however,only provided the results of a 6 month follow-up,2 studies13,15provided the results of a 12 month followup,1 study11provided the results of an 18 month follow-up,and 1 study10provided the results of 12 and 24 month follow-up.
3.2.3.Results of subgroup analysis
We divided the results into three mutually exclusive groups (readmission for COPD in 6 months,readmission for COPD in 18 months,all-cause readmission in 18 months)based on the reason for readmission and intervention duration to perform the subgroup analysis(Fig.3).In the readmission for COPD in 6 months,9,12,14there was no heterogeneity(P=0.54,I2=0%)and the fi xedeffect model was selected.Meta-analysis showed that transitional care can reduce readmission for COPD in 6 months[RR=0.51,95% CI(0.38,0.68),P<0.00001](Fig.3,Section A).In the readmission for COPD in 18 months group,9,11-14given that the control group patients in a study accepted extra care outside the hospital,this may have contributed to the small differences between groups in the meta-analysis,and we therefore did not include this research in the subgroup analysis.15There was no heterogeneity(P=0.66, I2=0%),the fi xed-effect model was selected,and meta-analysis showed that transitional care can reduce readmission for COPD in 18 months[RR=0.56,95%CI(0.45,0.69),P<0.00001](Fig.3, Section A).In the all-cause readmission in 18 months group,9,11,15there was no heterogeneity(P=0.25,I2=28%),the fi xed-effect model was selected,and meta-analysis showed that transitional care can reduce all-cause readmission[RR=0.72,95%CI (0.62,0.84),P<0.0001](Fig.3,Section B).
4.Discussion
4.1.Methodological quality of the included studies
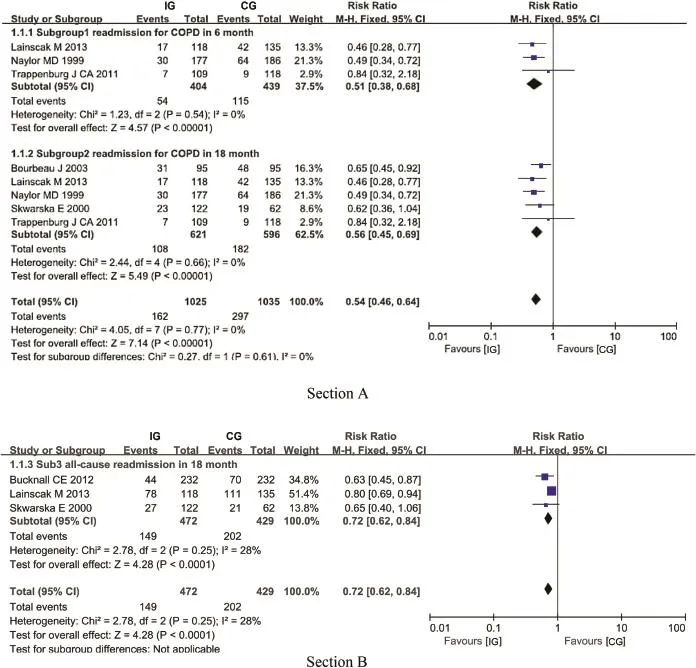
Fig.3.Forest plots.
In the 7 included studies,6 articles9,11-15reported random sequence generation and 5 articles9,11-13,15reported the process ofconcealing allocation.Although only 1 article12blinded the participants,all of the articles adopted a blinded outcome assessment to avoid detection bias.Four articles9,13-15reported the intention to treat analysis,and 6 articles9,10,12-15compared clinical and sociodemographic characteristics between the intervention group and control group at baseline and described speci fi c inclusion/exclusion criteria.
4.2.Effect of transitional care on readmission
Transitional care interventions have a signi fi cantly positive effect on reducing readmission for COPD in 6 months(95%CI 0.38 to 0.68,P<0.00001)and in 18 months(95%CI 0.45 to 0.69, P<0.00001),and there is less heterogeneity among these studies (both I2=0%).According to the subgroup analysis of all-cause readmission in 18 months,transitional care can also reduce allcause readmissions(95%CI 0.62 to 0.84,P<0.0001)and there is acceptable heterogeneity among these studies(I2=28%).As mentioned in the introduction,readmission occurred in almost one in fi ve discharged COPD patients.Therefore,the effect of transitional care on reducing readmission is crucial for patients with COPD.
The difference in the duration of transitional care intervention may in fl uence the effect on transitional care.One study10included in our review showed the reduction in the rate of all-cause readmissions in the intervention group compared to the control group: the reduction was-0.1(-0.27 to 0.07)in the preceding year,-0.70 (-0.95 to-0.46)in the fi rst year follow-up,and-0.44(-0.68 to-0.21)in the second year follow-up.Compared to the readmission difference between the control and intervention groups in the fi rst and second year follow-up,however,the difference in the second year was less than that in the fi rst year.The readmission difference in the preceding year was-6.3%and was-42.6%in the fi rst year follow-up and-26.9%in the second year follow-up.One potential limitation is that during the second year of follow-up, transitional care intervention was not under strict protocol regulation as in the fi rst year or the patients in intervention group were free from transition education.Thus,further long-term research in transitional care intervention should be executed in patients with COPD.
The outcome measures used in the included studies can also be discussed.Readmission was one of the most commonly used outcomes for discharged COPD patients,who always experience a long disease duration.Other limitations should also be taken into account when interpreting the results.Some of the included studies had a high risk of bias for several domains,which may reduce the possibility of drawing any conclusion.All of the studies that we included were RCTs to decrease the risk of bias,however,and baseline data between the two groups were comparable.Because personnel care can be hardly blinded at all in this type of intervention,researchers should be careful to minimize the risk of bias.
4.3.Study limitations
There are still some limitations in our meta-analysis.First, although the 7 studies included are RCTs,6 of those studies are not double blinded.Second,the control groups of some studies notonly adopted usual care but also additional interventions,such as postdischarge education,counseling or hospital support,which may have compromised the sensitivity of the studies to detect the true effects of transitional care.Third,some subgroups in our subgroup analyses had a small number of studies.Fourth,we did not conduct subgroup analysis controlling for other in fl uencing factors of transitional care,such as the intervention measures or intensity due to the limited number of studies.
4.4.Practice implications
Transitional care programs for patients with COPD should be extended.COPD is regarded as a signi fi cant public health concern that requires self-management strategies.Transitional care taught patients self-management skills and improved their ability to perform risk identi fi cation and acute exacerbation measurements, which were associated with readmission in adult patients with COPD.16Other suggestions from the present subgroup analyses include that the duration of transitional care should last≥6 and≤18 months and that methods to provide ongoing care should be developed.Moreover,more studies should verify the intervention components or executor skills and determine best practices.In addition,transitional care should be studied explicitly from the aspects of its executor,manner,duration of effect,intensity,intervention location,cost-effectiveness,and so on.Providing theories for how to maintain recommended self-care and management behaviors in patients'daily routines is also imperative.Finally, family caregivers and other social support systems can help facilitate adherence to the follow-up implementation.
5.Conclusions
In summary,transitional care in 7 studies achieves statistically signi fi cant bene fi ts in reducing COPD related or all-cause readmission for patients with COPD.Durations of≥6 and≤18 months are more likely to be effective,and the effect of transitional care on readmission weakens over intervention time,especially after the end of intervention.Both of these fi ndings point to the importance of ongoing intervention and the importance of reinforcement after the end of intervention.
Con fl icts of interest
All contributing authors declare no con fl icts of interest.
Acknowledgements
We thank Guohong Li,the director of the nursing department at Zhongda Hospital af fi liated to Southeast University,for study guidance.We also thank Wenmin Sun,the director of the nursing department at Chengnan Hospital,for valuable discussion.Funding from Jiangsu Provincial Commission of Health and Family Planning Foundation(H2015032)is gratefullyacknowledged.Thanks are due to Yijing Zhang,head nurse of the respiratory department at Zhongda Hospital,for producing the fi gures.We thank Chen Pan and Lei Lv for excellent technical assistance.
1.Li JM,Cheng SZ,Wei C,et al.Transitional care for patients with chronic obstructive pulmonary disease.Int J Nurs Sci.2014;1:157-164.
2.World Health Organization.Chronic respiratory diseases:burden of COPD. WHO.2008 May 20.Accessed 10 Oct 2016.www.who.int/respiratory/copd/ World_Health_Stat_2008/en/.
3.Hines Anika L,Barrett Marguerite L,Jiang H Joannna,Steiner Claudia A. Healthcare Cost and Utilization Project(HCUP)Statistical Briefs.Rockville:Agency for Healthcare Research and Quality(US);2014 April.Accessed 16 Oct 2016 www.ncbi.nlm.nih.gov/books/NBK206781/.
4.Jencks SF,Williams MV,Coleman EA.Rehospitalizations among patients in the Medicare fee-for-service program.N Engl J Med.2009;360:1418-1428.
5.Sharif R,Parekh TM,Pierson KS,Kuo YF,Sharma G.Predictors of early readmission among patients 40 to 64 years of age hospitalized for chronic obstructive pulmonary disease.Ann Am Thorac Soc.2014;11:685-694.
6.Majothi S,Jolly K,Heneghan NR,et al.Supported self-management for patients with COPD who have recently been discharged from hospital:a systematic review and meta-analysis.Int J Chron Obstruct Pulmon Dis.2015;10:853-867.
7.Fan VS,Gaziano JM,Lew R,et al.A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations:a randomized,controlled trial.Ann Intern Med.2012;156:673-683.
8.Higgins JPT,Green S,eds.Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.Updated March 2011.The Cochrane Collaboration. 2011.www.handbook.cochrane.org.
9.Lainscak M,Kadivec S,Kosnik M,et al.Discharge coordinator intervention prevents hospitalizations in patients with COPD:a randomized controlled trial. J Am Med Dir Assoc.2013;14,450.e1-e6.
10.Gadoury MA,Schwartzman K,Rouleau M,et al.Self-management reduces both short-and long-term hospitalisation in COPD.Eur Respir J.2005;26:853-857.
11.Skwarska E,Cohen G,Skwarski KM,et al.Randomized controlled trial of supported discharge in patients with exacerbations of chronic obstructive pulmonary disease.Thorax.2000;55:907-912.
12.Trappenburg JC,Monninkhof EM,Bourbeau J,et al.Effect of an action plan with ongoing support by a case manager on exacerbation-related outcome in patients with COPD:a multicentre randomised controlled trial.Thorax.2011;66: 977-984.
13.Bourbeau J,Julien M,Maltais F,et al.Reduction of hospital utilization in patients with chronic obstructive pulmonary disease:a disease-speci fi c selfmanagement intervention.Arch Intern Med.2003;163:585-591.
14.Naylor MD,Brooten D,Campbell R,et al.Comprehensive discharge planning and home follow-up of hospitalized elders:a randomized clinical trial.JAMA. 1999;281:613-620.
15.Bucknall CE,Miller G,Lloyd SM,et al.Glasgow supported self-management trial(GSuST)for patients with moderate to severe COPD:randomised controlled trial.BMJ.2012;344:e1060.
16.Grif fi ths TL,Burr ML,Campbell IA,et al.Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation:a randomised controlled trial. Lancet.2000;355:362-368.
How to cite this article:Liu M,Zhang Y,Li D-D,et al.Transitional care interventions to reduce readmission in patients with chronic obstructive pulmonary disease:A meta-analysis of randomized controlled trials.Chin Nurs Res.2017;4:84-91.http:// dx.doi.org/10.1016/j.cnre.2017.06.004
17 December 2016
*Corresponding author.
E-mail address:lmin89@163.com(M.Liu).
Peer review under responsibility of Shanxi Medical Periodical Press.
in revised form
- Frontiers of Nursing的其它文章
- A bibliometric study of the Journal of School Health:1965-2014☆
- In fl uence of mobile education on joint function and quality of life in patients after total hip arthroplasty☆
- Development of a frailty scale for elderly people in China☆
- How to establish an expected animal model of post-traumatic osteoarthritis?
- Chewing gum for postoperative ileus after colorectal surgery: A systematic review of overlapping meta-analyses
- Retraction notice to“Relationships between perceived social support and retention patients receiving methadone maintenance treatment in China mainland”[CNR 3/1(2016)11-15]