Aggressive primary hepatic epithelioid hemangioendothelioma: a case report and literature review
Mehdi Afrit, Meher Nasri, Soumaya Labidi, Nesrine Mejri, Houda El Benna, Hamouda Boussen Medical Oncology Department, Abderahman Mami Hospital, Ariana 2080, Tunisia
Aggressive primary hepatic epithelioid hemangioendothelioma: a case report and literature review
Mehdi Afrit*, Meher Nasri*, Soumaya Labidi, Nesrine Mejri, Houda El Benna, Hamouda Boussen Medical Oncology Department, Abderahman Mami Hospital, Ariana 2080, Tunisia
A new case of epithelioid hemangioendothelioma is reported to have occurred to a 67-year-old patient who consulted for rightsided chest pain. The work-up showed multiple right pulmonary lesions associated with bilateral moderate pleural effusion and left-sided pleural thickening and three hypodense nodules in the right lobe of the liver, peritoneal thickening, ascites, and multiple vertebral lytic lesions. The diagnosis of an epithelioid hemangioendothelioma was concluded through a histological examination of a computed tomography scan guided biopsy of the liver. The patient
Hemangioendothelioma; epithelioid; metastatic; liver; treatment
Introduction
Epithelioid hemangioendothelioma (EHE) is an exceptional and a very rare, low-grade malignant vascular endothelial cell tumor arising in soft tissue and rarely occurs in the liver. Hepatic epithelioid hemangioendothelioma (HEHE) was first described by Weiss and Enzinger in 19821. In 1984, Ishak et al.2reported a series of HEHE and collected 32 cases in the literature.
Positive diagnosis is frequently obtained based on histopathology and immunohistochemistry and is rarely obtained at the radiological imaging level. Most of the HEHEs are published as case studies and/or histopathological original entities because of their non-specific clinical and/or radiological features3. A new observation regarding a case of HEHE was reported highlighting the importance of immunohistopathological and radiological findings, and discussing the treatment strategy and the available data in the literature.
Case report
A 67-year-old male presented with a two-month history of right-sided parietal chest pain and right upper quadrant abdominal pain associated with mild dyspnea. The general condition was good without weight loss. Although the patient had a past medical history of hypertension, dyslipidemia, and hyperuricemia, he had no hepatitis. The physical examination showed right-sided abdominal tenderness. The systemic examination was unremarkable. The routine blood cell count and biochemical investigations (serum bilirubin, transaminases, alkaline phosphatase, and proteins) were within reference ranges. The serological tests for hepatitis B and C were negative. The chest X-ray showed right-sided minimal pleural effusion. The thoraco-abdominal computed tomography (CT) scan showed multiple right pulmonary lesions associated with bilateral moderate pleural effusion and left-sided pleural thickening. Furthermore, three hypodense nodules in the right lobe of the liver, with the largest lesion being 60 mm×52 mm in size in the segment IV, enhanced by contrast material injection suggesting their malignancy were revealed. Peritoneal thickening, ascites, and multiple vertebral lytic lesions were also observed. The upper endoscopy showed chronic diffuse gastritis. The colonoscopy showed sigmoidal diverticulosis. Tumor markers, including AFP, HCG, PSA, and CA19-9, were all within the normal limits.
Histological exam was performed on a CT-scan guidedcore biopsy of the nodule of segment VI of the liver, showing proliferation of polygonal epithelioid tumor cells with abundant vacuolated cytoplasm (Figure 1) positive for vimentin (+++), CD31 (+) (Figure 2), CD 138(+), pan cytokeratin (AE1/AE3) (+) (Figure 3), factor VIII antigen (focal) (+), and a low ki-67 (10%) proliferative activity. However, they were negative for CK7, CK20, CK19, HMB45, PSA, Desmine, NSE, HAS, and CD99. This immunohistochemical profile suggested the diagnosis of HEHE metastasis into bones.
The decision of the multi-disciplinary board was to begin a primary mono-chemotherapy with Adriamycin (75 mg/m2per three weeks) and intravenous bisphosphonates, considering the extensive and the progressive nature of the disease, and because liver transplantation is unavailable in Tunisia. A CT scan was performed after 6 cycles and demonstrated stable disease, however, the patient presented bowel obstruction. The laparoscopy showed a peritoneal carcinomatosis related to the HEHE on biopsy. Supportive care was opted because of general status impairment. The patient died after 16 months of follow-up.

Figure 1 Liver biopsy specimen: intra sinusoïdal epithelioid tumor cells proliferation (H&E staining, 200×).

Figure 2 The tumor cells of epithelioid hemangioendothelioma are positive for CD31 by immunohistochemical staining (IHC staining, 100×).
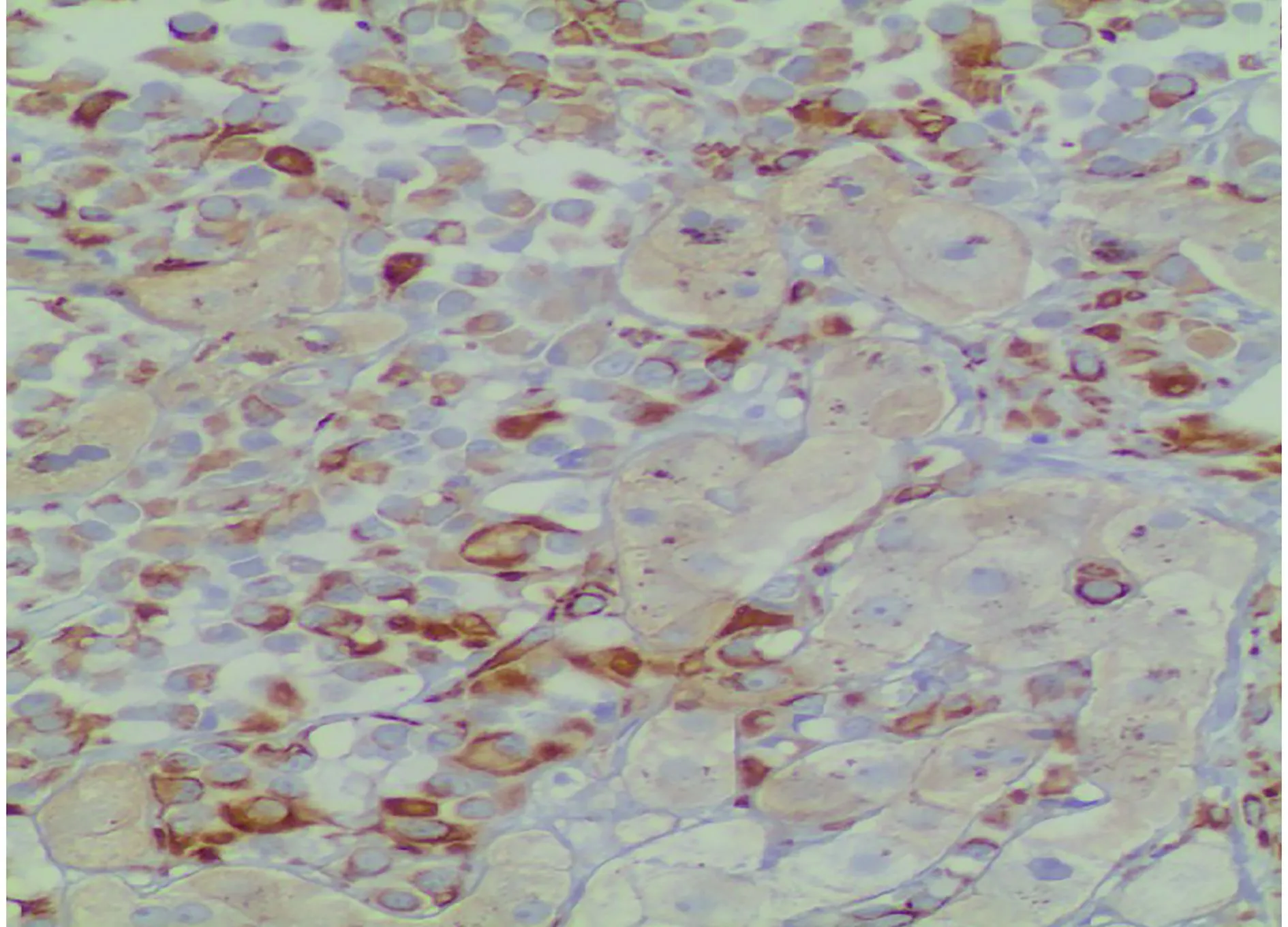
Figure 3 The tumor cells of epithelioid hemangioendothelioma are positive for cytokeratin by immunohistochemical staining (IHC staining, 200×).
Discussion
The first series of EHE concerning 32 cases was published in 1984 by Ishak et al.2. Although HEHE is a rare vascular tumor between intermediate and malignant potential, WHO classification considers HEHE as malignant neoplasm. Less than 500 cases have been reported in the literature. Mehrabi et al.4reviewed 402 HEHE patients treated from 1984 to 2005. Most HEHE were asymptomatic; clinical manifestation of this disease is not specific and the most common symptoms include right upper quadrant pain (48.6%), hepatomegaly (20.4%), and weight loss (15.6%)4. In our case, the patient was suffering from abdominal distension for two months along with a mild dyspnea. Extrahepatic metastases were observed in 36.6% of patients. The extrahepatic sites included lungs (8.5%), regional lymph nodes (7.7%), peritoneum (6.1%), bone (4.9%), spleen (3.2%), and diaphragm (1.6%). Several rare first manifestation of this disease, such as an ischemic stroke, were also observed as reported by Zis et al.5. In our case, HEHE occurred in liver and was widely metastasized to the peritoneum, lung, and bone. HEHE patients are negative for alpha-fetoprotein, ACE, and CA19-9, which was similar to the patient presented in the present case study. The T1W1 images from the MRIshows hypointense lesions with lower signal intensity in the center and intermediate to high signal intensity in the T2W2 image. The “capsular retraction” sign caused by an intense fibroproliferation and a “halo” sign caused by central coagulative necrosis are the important CT and MRI manifestations that provide diagnosis accuracy6. The diagnosis depends on the histopathological staining of cells. Makhlouf et al.7reviewed 137 HEHE cases and demonstrated that approximately 60% to 80% of HEHE patients were initially misdiagnosed because of the variable patterns of the tumor. The most common misdiagnoses were cholangiocarcinoma, angiosarcoma, and hepatocellular carcinoma (HCC). Despite the infiltrating standard of lesions in HEHE, hepatic acini and portal spaces tend to be preserved. The tumor is composed of epithelioid or dendritic tumor cells with intracytoplasmic lumen. Vascular invasion is characterized by immunoreactivity to CD31, CD34, and/or Factor VIII antigens and lack immunoreactivity to epithelial markers, mainly cytokeratins. HEHE diagnosis should be considered in the presence of one or more aspects8. In the current case, typical tumor architecture and immunohistochemical positivity of endothelial cell markers (such as CD-31) supported the diagnosis of HEHE. In the present case, the diagnosis of HEHE was made on core biopsy assisted by immunohistochemistry. Mehrabi et al.4reviewed the therapeutic modalities used in 402 HEHE patients treated from 1984 to 2005. The treatment methods were clearly documented in 286 patients. The most common management was liver transplantation (LT) in 128 patients (44.8%), followed by no treatment in 71 patients (24.8%), chemotherapy or radiotherapy in 60 patients (21%), and liver resection in 27 patients (9.4%). Currently, HEHE treatment has no standard treatment; however, orthotropic liver transplantation represents the ideal treatment even in cases of metastatic disease, whereas liver resection can be performed in case of single nodular type9. Prolonged survival after liver transplantation in 59 patients transplanted for HEHE has been reported to the European Liver Transplant Registry, in which 1-, 5- and 10-year post-LT survival rates were 93%, 83%, and 72%, respectively9. Some studies reported that the use of sorafenib exhibits more advantages over other antiangiogenic agents because of its dual anti-tumor activity10. Metastatic HEHE has shown to be successfully treated with the use of thalidomide via blocking the proliferation of the malignant vascular endothelial cells11. Recently, some authors reported a malignant HEHE successfully treated with pegylated liposomal doxorubicin12. The management options for HEHE include liver resection, LT, chemotherapy, radiotherapy, immunotherapy, or followup alone. The prognostic factors of HEHE are unclear, even if some authors have reported that the presence of symptoms, older age, and elevated serum CA19-9 negatively affect the outcome13. Furthermore, Cardinal et al.14found that the presence of extrahepatic disease beyond regional portal nodes was a negative predictor of outcome. All in all, the prognosis of HEHE may vary widely, with some patients presenting a slow-growing disease and others presenting a rapidly progressive form, however, HEHE, compared to other malignant hepatic tumor, is considered to be associated with excellent prognosis15.
Conclusions
The treatment and follow-up of HEHE has no standard therapeutic strategy because of its rare and variable clinical course. Orthotopic liver transplantation appears to be the only hope for HEHE patients because of the multifocality of the tumor. Thus, early diagnosis and treatment is crucial because the outcome of the disease is unpredictable.
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma a vascular tumor often mistaken for a carcinoma. Cancer. 1982; 50: 970-81.
2.Ishak KG, Sesterhenn IA, Goodman ZD, Rabin L, Stromeyer FW. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and followup study of 32 cases. Hum Pathol. 1984; 15: 839-52.
3.Mistry AM, Gorden DL, Busler JF, Coogan AC, Kelly BS. Diagnostic and therapeutic challenges in hepatic epithelioid hemangioendothelioma. J Gastrointest Cancer. 2012; 43: 521-5.
4.Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006; 107: 2108-21.
5.Zis P, Assi A, Kravaritis D, Sevastianos VA. Ischemic stroke as the first manifestation of hepatic epithelioid hemangioendothelioma. J Stroke Cerebrovasc Dis. 2014; 23: e237-40.
6.Lin J, Ji Y. CT and MRI diagnosis of hepatic epithelioid hemangioendothelioma. Hepatobiliary Pancreat Dis Int. 2010; 9: 154-8.
7.Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999; 85: 562-82.
8.Naqvi J, Ordonez NG, Luna MA, Williams MD, Weber RS, El-Naggar AK. Epithelioid hemangioendothelioma of the head andneck: role of podoplanin in the differential diagnosis. Head Neck Pathol. 2008; 2: 25-30.
9.Lerut JP, Orlando G, Adam R, Schiavo M, Klempnauer J, Mirza D, et al. The place of liver transplantation in the treatment of hepatic epitheloid hemangioendothelioma: report of the European liver transplant registry. Ann Surg. 2007; 246: 949-57.
10.Sangro B, Iñarrairaegui M, Fernández-Ros N. Malignant epithelioid hemangioendothelioma of the liver successfully treated with Sorafenib. Rare Tumors. 2012; 4: e34
11.Raphael C, Hudson E, Williams L, Lester JF, Savage PM. Successful treatment of metastatic hepatic epithelioid hemangioendothelioma with thalidomide: a case report. J Med Case Rep. 2010; 4: 413
12.Grenader T, Vernea F, Reinus C, Gabizon A. Malignant epithelioid hemangioendothelioma of the liver successfully treated with pegylated liposomal doxorubicin. J Clin Oncol. 2011; 29: e722-4.
13.Wang LR, Zhou JM, Zhao YM, He HW, Chai ZT, Wang M, et al. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg. 2012; 36: 2677-83.
14.Cardinal J, de Vera ME, Marsh JW, Steel JL, Geller DA, Fontes P, et al. Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg. 2009; 144: 1035-9.
15.Baron PW, Amankonah T, Cubas RF, Kore AH, Elihu A, de Vera ME, et al. Diffuse hepatic epithelioid hemangioendothelioma developed in a patient with hepatitis C cirrhosis. Case Rep Transplant. 2014; 2014: 694903
Cite this article as: Afrit M, Nasri M, Labidi S, Mejri N, El Benna H, Boussen H, et al. Aggressive primary hepatic epithelioid hemangioendothelioma: a case report and literature review. Cancer Biol Med. 2017; 14: 187-90. doi: 10.20892/j.issn.2095-3941.2016.0105
*These authors have contributed equally to this work
Meher Nasri
E-mail: mehernasri352@yahoo.fr
December 28, 2016; accepted February 3, 2017.
Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
a primary mono-chemotherapy with Adriamycin (75 mg/m2every three weeks) and intravenous bisphosphonates without response and general status impairment. The patient died after 16 months of follow-up.
 Cancer Biology & Medicine2017年2期
Cancer Biology & Medicine2017年2期
- Cancer Biology & Medicine的其它文章
- Developmental pathways associated with cancer metastasis: Notch, Wnt, and Hedgehog
- Cellular immunity augmentation in mainstream oncologic therapy
- Mesenchymal stromal cells’ role in tumor microenvironment: involvement of signaling pathways
- Simplified microsatellite instability detection protocol provides equivalent sensitivity to robust detection strategies in Lynch syndrome patients
- Significance of stromal-1 and stromal-2 signatures and biologic prognostic model in diffuse large B-cell lymphoma
- Immunohistochemical evaluation of vitamin D receptor(VDR) expression in cutaneous melanoma tissues and four VDR gene polymorphisms
