Rapid response of brain metastasis to crizotinib in a patient with KLC1-ALK fusion and MET gene amplification positive non-small cell lung cancer: a case report
Peng Wang, Pei Xiao, Yingnan Ye, Pengpeng Liu, Lei Han, Li Dong, Chunhua She, Jinpu YuDepartment of Neuro-Oncology;Cancer Molecular Diagnostic Center, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin's Clinical Research Center for Cancer, Tianjin 300060, China
Rapid response of brain metastasis to crizotinib in a patient with KLC1-ALK fusion and MET gene amplification positive non-small cell lung cancer: a case report
Peng Wang1*, Pei Xiao2*, Yingnan Ye2, Pengpeng Liu2, Lei Han2, Li Dong2, Chunhua She1, Jinpu Yu21Department of Neuro-Oncology;2Cancer Molecular Diagnostic Center, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin's Clinical Research Center for Cancer, Tianjin 300060, China
Non-small cell lung cancer (NSCLC) ranks as the leading cause of cancer-related death in the world. Brain metastasis (BM) is a common complication of NSCLC, with 25%–40% of patients developing BM during the course of the disease. A significant strategy of local disease control in the central nervous system is radiation therapy. With the development of precision medicine, the concept of treating lung cancer BM has gradually changed. In this case, we performed a surgical procedure to obtain enough tumor tissue for the detection of the target gene and other related experiments after the patient was informed. Finally, we found that the patient had both hepatocyte growth factor receptor (MET) gene amplification and kinesin light chain 1-anaplastic lymphoma kinase fusion (KLC1-ALK) through next-generation sequencing and showed sensitivity to the targeted therapy of crizotinib. The patient exhibited good response. Our case was successful and underwent targeted therapy with the guidance of precise diagnosis.
NSCLC; precision medicine; KLC1-ALK fusion; MET amplification; next-generation sequencing
Introduction
Lung adenocarcinoma is the most common subtype of nonsmall cell lung cancer (NSCLC), which is the leading cause of cancer-related deaths worldwide, with a five-year survival rate of approximately 2% in the metastatic setting1. Early accurate diagnoses are significant for the prognosis of NSCLC patients. Lung cancer diagnoses have advanced unprecedentedly in the past decade. Therefore, developing a molecular test that obtains a huge number of potentially clinical genetic variants through minimally invasive techniques is a huge challenge. The implementation of the nextgeneration sequencing (NGS) platforms for molecular diagnoses in NSCLC patients is becoming common2. These platforms enable multiple genetic variant screening from a simplex sample, thus benefitting patients.
Brain metastasis (BM) is a common event in NSCLC, resulting in significant morbidity and poor survival prognosis in 25%–40% of NSCLC patients3usually within the first two years after primary tumor diagnosis. In fact, cytotoxic chemotherapy has a limited role in NSCLC patients with BM because of poor blood-brain barrier penetration. Local therapy, such as radiotherapy, remains one of the effective treatments and the standard for majority of patients with BM. However, some shortcomings are present in radiation therapy, such as brain edema of the irradiated part and change in the blood vessels with the aggravation of intracranial pressure4. The genotype-driven treatment of NSCLC has obtained great success in the previous decade with effective targeted therapies in patients with distinct molecular alterations. Genomic studies have also identified several targetable molecular alterations, such as EGFR and ALK, and so on.
With the development of targeted therapy, the concept of treating BM in NSCLC has gradually changed. Currently, as the disease develops, accurate diagnosis and precise treatment are constantly changing. In this study, we present an NSCLC patient case with hepatocyte growth factorreceptor (MET) gene amplification and kinesin light chain 1-anaplastic lymphoma kinase (KLC1-ALK) fusion who showed sensitivity to crizotinib but failed to respond to chemotherapy and did not undergo radiotherapy. Treatment with crizotinib effectively controlled the tumor in BM. To date, the prognosis of such patients with both KLC1-ALK fusion and MET amplification is unreported. Therefore, crizotinib may be an effective treatment option for patients with both MET amplification and KLC1-ALK fusion following the development of BM. Our case was successful with the guidance of precise diagnosis.
Case report
A 57-year-old man was diagnosed with advanced lung cancer by transbronchial lung biopsy in our hospital in December 2015. The patient previously underwent seed implantation postoperatively and received chemotherapy with vinorelbine plus cisplatin outside our hospital. The patient did not feel uncomfortable until a mass of approximately 0.8 cm in the left frontal lobe was detected through a brain magnetic resonance imaging (MRI) scan on June 15, 2016. Thus, the patient was referred to our department for further treatment. After comprehensive consideration, the patient underwent right ventricle Ommoya capsule implantation and right occipital lobe neoplasm resection on June 23, 2016 along with genetic testing, immunohistochemical detection, and drug sensitivity.
Pathologically, the mass was confirmed as a metastatic tumor from lung cancer, and the immunohistochemical analysis tended toward carcinoma. To re-evaluate the molecular features, DNA extracted from the tumor tissue was subjected to DNA sequencing analysis by NGS. The results showed that the patient had both MET gene amplification and a novel ALK rearrangement, collectively known as KLC1-ALK fusion, which was created by KLC1 exon 9 and ALK exon 20 (Figure 1A and 1B). The BM progressed despite gefitinib administration. Thus, crizotinib administration began on July 12, 2016 after gefitinib treatment, with the former not showing clinically relevant adverse effects in the patient. The dosage of crizotinib treatment was 250 mg/day at twice a day for this patient. After four weeks of crizotinib therapy, a repeated brain MRI examination demonstrated a slight decrease of tumor size in the left frontal lobe and amelioration of the surrounding edema on August 9, 2016 compared with the brain MRI scan in July 2016. However, the patient decided to undergo radiotherapy instead of crizotinib treatment for a variety of reasons. Cranial MRI examination on August 23, 2016 confirmed a dramatic increase in contrast-enhancing lesion size of about 1.6 cm and a deterioration of the previously identified CNS lesion that had decreased from crizotinib treatment (Figure 2).
Discussion
We have entered a new era of personalized medicine in the field of cancer research and treatment, in which biomarkers are used to select patients who are likely to benefit from a specific drug. The success of molecular targeted therapy enables the selection of specific tumor-targeting drugs in NSCLC patients. Therefore, accurate treatment depends on accurate diagnosis. The development of new genotype-directed therapies is widespread in solid tumor oncology, and it leads to an increasing application of NGS panels to test tumor biopsies for a wide range of potentially targetable mutations. The implementation of NGS platforms and genomic technologies has led to the discovery of new molecular events that characterize NSCLC and may represent vital oncogenic drivers.
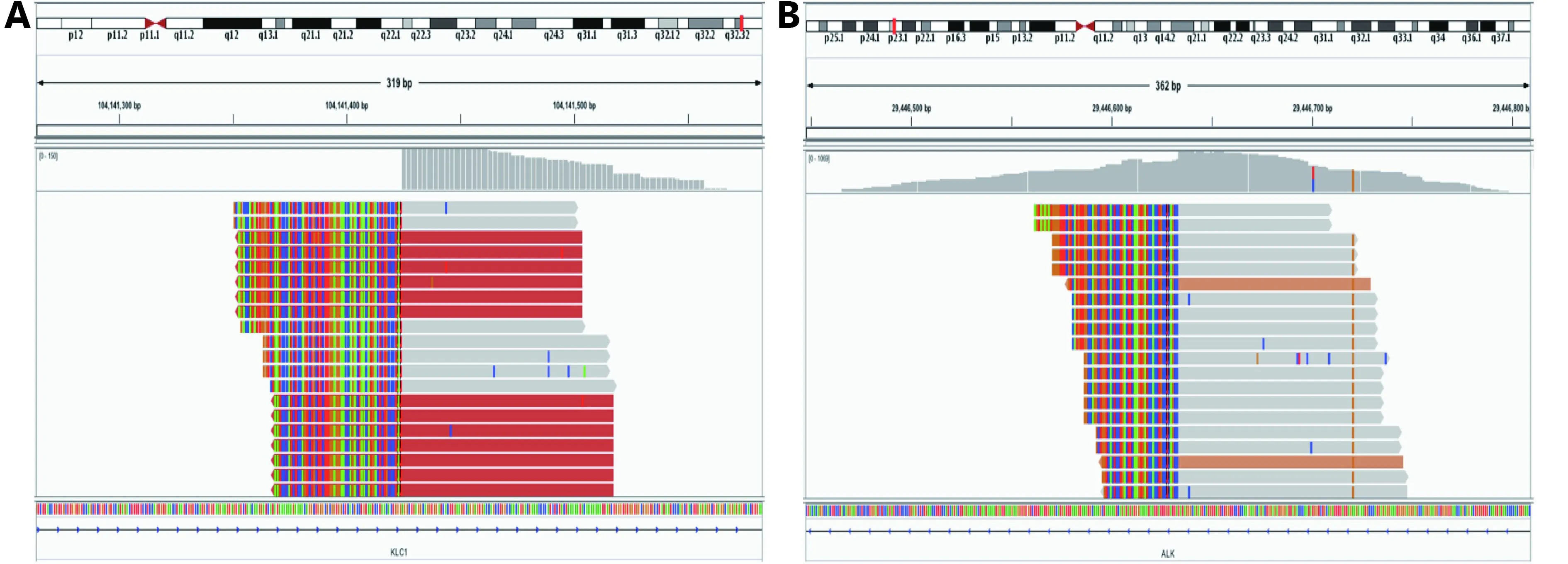
Figure 1 NGS indicating that the patient has a novel ALK rearrangement, that is, KLC1-ALK fusion, which is created by KLC1 exon 9 (A) and ALK exon 20 (B).
ALK fusion is the most common activation and overexpression mechanism in NSCLC, and it occurs in approximately 5% of cases5. Eight fusion partners of ALK in NSCLC patients, including echinoderm microtubuleassociated protein-like 4 (E ML4), TRK-fused gene, kinesin family member 5B (K IF5B), kinesin light chain 1 (KLC1), protein tyrosine phosphatase and nonreceptor type 3, huntingtin interacting protein 1 (HIP1), spectrin beta nonerythrocytic 1 (SPTBN1), and translocated promoter region (TPR), have been reported. Among these genes, KLC1-ALK fusion was first reported in 20126, and it was found in formalin-fixed and paraffin-embedded tissue. KLC1-ALK fusion is extremely rare but existent in lung adenocarcinoma. MET amplification occurs in about 5%–22% of NSCLC7. It is one of the acquired resistance mechanisms to EGFR tyrosine kinase inhibitors and has been associated with poor outcomes.
In the last decade, we witnessed great progress in NSCLC therapy. Molecular-based targeted therapy has fundamentally changed the prognosis of NSCLC patients whose tumor subtypes harbor actionable abnormalities, consistent with the strategic concept of precision medicine in matching different subtypes with effective targeted therapies. Crizotinib, an oral small inhibitor of ALK, ROS1, and MET receptor kinase, has demonstrated significant antitumor efficacy in advanced NSCLC patients and has been used to treat ALK-positive NSCLC8. The management of patients with BM continues to present a major challenge in oncology, with relatively low response rates and limited survival benefits brought by the current chemotherapeutic options. Although a few studies have verified the antitumor efficacy of crizotinib in NSCLC patients with ALK-positive or MET amplification, the drug exhibits extremely poor blood–brain barrier penetration. Therefore, crizotinib has limited applications in the treatment of NSCLC patients with BM9,10. In addition, the efficacy of targeted therapy on patients with both KLC1-ALK fusion and MET amplification has not been reported. Therefore, we report a rare NSCLC patient with BM who showed efficacy of crizotinib treatment.
A significant strategy of local disease control in the CNS is radiation therapy, which is still the standard of care for the majority of NSCLC patients with BM. Based on the concept of targeted therapy in this study, we prescribed NGS-based genetic testing before conducting further treatments. The metastatic tumor tissues in the CNS were partly resected, and all NGS assays were performed on the Illumina Miseq platform using the capture-based target sequencing method. A rare combinative mutation of both KLC1-ALK fusion and MET amplification was detected using the NGS assay; this combination is hardly identified in NSCLC patients through conventional diagnostic methods, such as FISH and IHC. The NGS results were simultaneously confirmed with the conventional IHC method rather than FISH. Both KLC1-ALK fusion and MET amplification point to the use of the targeted drug crizotinib, which is effective in NSCLC patients with either mutation. Therefore, crizotinib treatment was used as the optimal therapy for this rare case without presenting any ethical and clinical conflicts. The patient underwent four weeks of crizotinib therapy, which resulted in tumor mass shrinkage from approximately 0.8 cm×0.6 cm to 0.6 cm×0.5 cm. A slight decrease in tumor size in the left frontal lobe and the amelioration of the surrounding edema were confirmed by MRI. Unfortunately, the patient decidedto undergo radiation treatment instead of the targeted therapy after one cycle of crizotinib treatment. One month later, cranial MRI examination confirmed the increase in tumor size to nearly 1.6 cm×1.4 cm after stopping the crizotinib treatment. This outcome implied a significant deterioration of the previously controllable CNS lesion and indirectly confirmed the clinical efficacy of crizotinib for this rare case of NSCLC with BM. In summary, the case significantly demonstrated the capability of NGS assay to indicate optimal therapeutic options for any patient with distinct genetic characteristics.
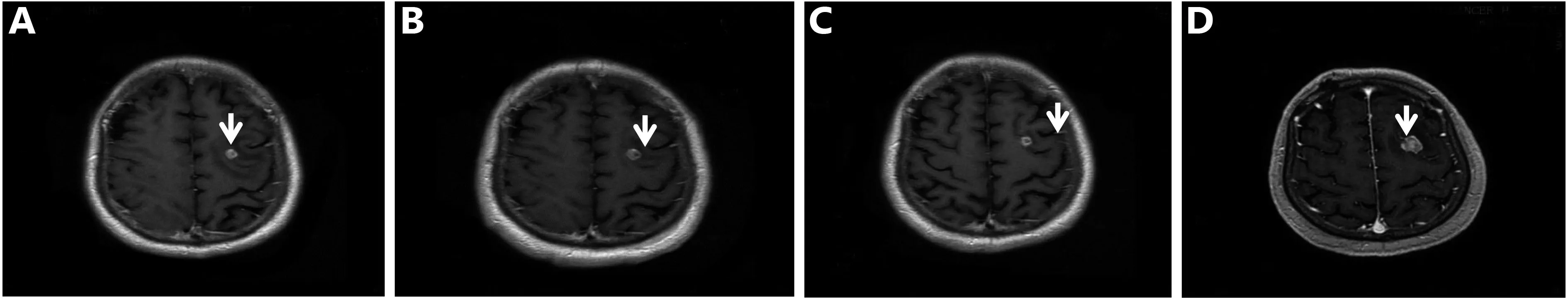
Figure 2 MRI scans of BM. (A) A mass that is approximately 0.8 cm×0.6 cm in the left frontal lobe observed on June 15, 2016 (preoperation). (B) MRI demonstrates the slight increase in mass size on June 27, 2016 (post-operation). (C) A repeated brain MRI examination demonstrates a slight decrease in tumor size of approximately 0.6 cm×0.5 cm in the left frontal lobe and the amelioration of the surrounding edema on August 9, 2016. (D) On August 23, 2016, the MRI examination confirmed a dramatic increase in tumor size of about 1.6 cm×1.4 cm.
NGS assay is now available for clinical usage, but it is not as commonly applicable as conventional diagnostic methods, such as IHC, FISH, and PCR. This case indicated the clinical feasibility of the NGS assay for advanced NSCLC patients who have no opportunity for routine therapies. In our case, we broke the traditional concept of treatment by using NGS technology for the detection of metastatic tumors and achieved success by detecting KLC1-ALK fusion and MET amplification. The patient underwent targeted therapy of crizotinib and showed a promising response to this strategy. Our case was successful and underwent targeted therapy with the guidance of precise diagnosis. We believe that a good medical strategy can bring new opportunities for cancer patients.
This interesting case verifies that MET amplification and KLC1-ALK gene fusion can co-depend in NSCLC patients and that their combination may be a biomarker for a relatively poor prognosis.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No. 81472473), National Science and Technology Support Program of China (Grant No. 2015BAI12B15 and 2015BAI12B12), Project of Science and Technology of Tianjin (Grant No.13ZCZCSY20300) and Key Project of Health Industry of Tianjin (Grant No.16KG126).
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Stinchcombe TE, Socinski MA. Current treatments for advanced stage non-small cell lung cancer. Proc Am Thorac Soc. 2009; 6: 233-41.
2.Hiley CT, Le Quesne J, Santis G, Sharpe R, de Castro DG, Middleton G, et al. Challenges in molecular testing in non-smallcell lung cancer patients with advanced disease. Lancet. 2016; 388: 1002-11.
3.Preusser M, Berghoff AS, Koller R, Zielinski CC, Hainfellner JA, Liebmann-Reindl S, et al. Spectrum of gene mutations detected by next generation exome sequencing in brain metastases of lung adenocarcinoma. Eur. J. Cancer. 2015; 51: 1803-11.
4.Le Pe P-rr C, Sun A, Slotman BJ, De Ruysscher D, Belderbos J, Gore EM. Prophylactic cranial irradiation for patients with lung cancer. Lancet Oncol. 2016; 17: e277-93.
5.Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007; 448: 561-6.
6.Togashi Y, Soda M, Sakata S, Sugawara E, Hatano S, Asaka R, et al. KLC1-ALK: A novel fusion in lung cancer identified using a formalin-fixed paraffin-embedded tissue only. PLoS ONE. 2012; 7: e31323
7.Desai A, Menon SP, Dy GK. Alterations in genes other than EGFR/ALK/ROS1 in non-small cell lung cancer: trials and treatment options. Cancer Biol Med. 2016; 13: 77-86.
8.Yoshida T, Oya Y, Tanaka K, Shimizu J, Horio Y, Kuroda H, et al. Clinical impact of crizotinib on central nervous system progression in ALK-positive non-small lung cancer. Lung Cancer. 2016; 97: 43-7.
9.Shi WY, Dicker AP. CNS metastases in patients with non-small-cell lung cancer and ALK gene rearrangement. J Clin Oncol. 2016; 34: 107-9.
10.Johung KL, Yeh N, Desai NB, Williams TM, Lautenschlaeger T, Arvold ND, et al. Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J Clin Oncol. 2016; 34: 123-9.
Cite this article as: Wang P, Xiao P, Ye Y, Liu P, Han L, Dong L, et al. Rapid response of brain metastasis to crizotinib in a patient with KLC1-ALK fusion and MET gene amplification positive non-small cell lung cancer: a case report. Cancer Biol Med. 2017; 14: 183-6. doi: 10.20892/j.issn.2095-3941.2017.0017
*These a uthors have contributed equally to this work
Jinpu Yu
E-mail: yujinpu@tjmuch.com
February 20, 2017; accepted April 7, 2017.
Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年2期
Cancer Biology & Medicine2017年2期
- Cancer Biology & Medicine的其它文章
- Developmental pathways associated with cancer metastasis: Notch, Wnt, and Hedgehog
- Cellular immunity augmentation in mainstream oncologic therapy
- Mesenchymal stromal cells’ role in tumor microenvironment: involvement of signaling pathways
- Simplified microsatellite instability detection protocol provides equivalent sensitivity to robust detection strategies in Lynch syndrome patients
- Significance of stromal-1 and stromal-2 signatures and biologic prognostic model in diffuse large B-cell lymphoma
- Immunohistochemical evaluation of vitamin D receptor(VDR) expression in cutaneous melanoma tissues and four VDR gene polymorphisms
