复杂TASC D级髂股动脉病变的杂交手术治疗
王曰伟,李永欣,李长风,张中旺,李君,王豪夫
(青岛大学附属医院血管外科,青岛 266003)
随着人口老龄化和代谢异常导致的发病率增高,下肢动脉硬化性闭塞症(arteriosclerosis obliterans,ASO)已成为老年人突出的问题,其中>70岁的老年人患病率达20%[1]。动脉闭塞引起下肢缺血症状,轻则间歇性跛行,重则静息痛、肢体坏疽,严重影响患者生活质量。严重肢体缺血(critical limb ischemia,CLI)患者1年截肢率27%,5年死亡率46%[2]。对于ASO的治疗,泛大西洋学会共识(Trans-Atlantic Inter-Society Consensus, TASC)Ⅱ[3]根据病变的部位、程度和范围进行了分级,并推荐了相应的治疗原则,A级、B级和高危C级病变首选血管腔内治疗,D级病变首选手术治疗。随着腔内技术和器材的发展,如支架植入、斑块旋切、血栓抽吸、准分子激光消融、药物涂层球囊[3-7],目前腔内治疗已成为D级病变的重要手段,但尚未有大数据支持和指南推荐D级病变首选腔内治疗。而对于复杂D级病变,即主髂动脉或股腘动脉D级病变分别合并流出道或流入道C级以上病变,病变广泛复杂,需要同期处理主髂动脉和股腘动脉病变,改善流入道或流出道。单纯腔内治疗成功率低,操作复杂,单纯手术创伤大,患者难以耐受,因此,对于该类患者尤其还多合并基础疾病和全身血管病变的患者进行治疗乃是血管外科医师比较纠结的临床问题。我科根据病变部位、类型和患者身体状况,采取手术和腔内联合方式共治疗复杂D级髂股动脉病变27例,取得良好效果,报道如下。
1 对象与方法
1.1 研究对象
回顾性分析2007年1月至2013年12月期间我院接收的27例复杂TASC D级病变患者,男性25例,女性2例;年龄62~89(75.1±7.3)岁;患者Rutherford[3]Ⅲ、Ⅳ、Ⅴ级分别有10、12和5例,合并症包括高血压19例,冠心病9例,2型糖尿病11例,脑栓塞5例,高脂血症9例,吸烟15例。入组患者均为复杂D级髂股动脉病变,即D级主髂动脉病变合并C级或D级股腘动脉病变或D级股腘动脉病变合并C级主髂动脉病变。
1.2 方法
所有患者术前行CT血管成像(computed tomography angiography, CTA),根据TASC病变分级原则,将患者分为C级主髂动脉病变合并D级股腘动脉病变14例,D级主髂动脉病变合并C级股腘动脉病变7例,D级主髂动脉病变合并D级股腘动脉病变6例。因为患者均是复杂D级病变,合并流出道或流入道C级以上病变,我科根据病变类型和患者身体状况采取个体化治疗,选择创伤较小的手术方式;记录术前、术后6、12、24和36个月踝肱指数(ankle-brankial index, ABI),并分析术前及术后随访12、24和36个月的通畅率。
1.3 统计学处理
2 结 果
2.1 术中所见
C级主髂动脉病变合并D级股腘动脉病变14例。其中8例行髂动脉支架植入、股深动脉成形、股腘动脉旁路;C级主髂动脉病变包括单侧髂外动脉长段狭窄(3例)及单侧髂外动脉闭塞累及髂内动脉或股总动脉近端(5例),D级股腘动脉病变是股浅动脉全程闭塞,股深动脉狭窄且膝关节动脉网存在。髂动脉支架植入后行股深动脉成形、股腘动脉人工血管旁路,其中3例直视下顺行穿刺股总动脉吻合口近端前外侧壁,置入导管鞘于人工血管内,行下肢动脉造影、膝下动脉球囊扩张(图1)。其余6例行髂动脉取栓、支架植入、股腘动脉人工血管旁路;C级主髂动脉病变表现为髂外动脉闭塞累及股总动脉,D级股腘动脉病变表现为股浅动脉全程闭塞;术中发现股总动脉血栓,切开股总动脉,行髂动脉导管取栓、球囊扩张、支架植入,后行股腘动脉人工血管旁路,其中2例术中穿刺股总动脉,行膝下动脉球囊扩张(图2)。
D级主髂动脉病变合并C级股腘动脉病变7例。D级主髂动脉病变是患侧髂及髂外动脉闭塞,其中对侧髂动脉狭窄1例, 髂动脉瘤1例; C级股腘动脉病变是股浅动脉多发狭窄和闭塞。双侧腹股沟切口,游离股动脉,若对侧髂动脉正常,直接行股股动脉人工血管旁路;若对侧髂动脉狭窄,先行髂动脉支架植入,再行股股动脉人工血管旁路,后直视下顺行穿刺患侧股总动脉吻合口近端前外侧壁,行股浅动脉球囊扩张、支架植入(图3)。
D级主髂动脉病变合并D级股腘动脉病变6例。其中2例单侧髂总动脉远段和髂外动脉全程闭塞,胫后动脉受累1例,胫前动脉和腓动脉同时受累1例;游离患侧股动脉,先用取栓导管取出髂动脉血栓,若取栓导管无法通过髂动脉闭塞段,导管、导丝通过后,再交换取栓导管,残余闭塞和狭窄支架植入,后行股腘动脉人工血管旁路,再直视下顺行穿刺股动脉,置入导管鞘于人工血管内,行膝下动脉球囊扩张。2例患侧髂动脉全程闭塞,对侧髂动脉狭窄,行对侧髂动脉支架植入、股股动脉人工血管旁路、股腘动脉人工血管旁路,其中1例行股深动脉成形、膝下动脉球囊扩张。2例主髂动脉闭塞,行腹主动脉切开取栓、闭塞侧股动脉切开取栓,再行主股动脉人工血管旁路。直视下顺行穿刺吻合口近侧股动脉前外侧壁,行下肢动脉造影、球囊扩张、股动脉支架植入(图4)。术中主髂动脉病变经肱动脉穿刺建立通路4例;髂动脉植入覆膜支架8例,其中Fluency 3例,Viabahn 5例;股股动脉旁路人工血管为8 mm×40 cm外支撑环(巴德),股腘动脉旁路人工血管为6 mm×50 cm袖状碳涂层(巴德),股动脉内膜剥脱9例,腘动脉内膜剥脱6例。
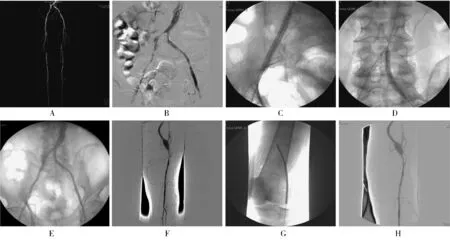
图1 C级主髂动脉病变合并D级股腘动脉病变杂交手术Figure 1 Hybrid surgery of type C aorto-iliac lesion and type D femoro-popliteal lesion
A: CT angiography shows occlusive lesions of the iliac and femoral artery; B: stenosis and occlusion of the bilateral iliac artery(DSA); C: balloon dilation of the right iliac artery after stenting; D: balloon dilation of the left iliac artery after stenting; E: the patent iliac artery after stenting(DSA); F: severe stenosis of the popliteal artery distal to the anastomosis after femoro-popliteal bypass and endarterectomy(DSA); G: balloon dilation of the popliteal artery; H: the patent popliteal and peroneal artery(DSA). DSA: digital subtraction angiography

图2 C级主髂动脉病变合并D级股腘动脉病变杂交手术Figure 2 Hybrid surgery of type C aorto-iliac lesion and type D femoro-popliteal lesion
A: occlusive lesion of the right iliac artery involving the common femoral artery(DSA); B: balloon dilation of the iliac artery after thrombectomy of the iliac artery; C: the patent right iliac artery after stenting(DSA); D: extensive occlusive lesions below the knee after femoro-popliteal bypass(DSA); E: the patent popliteal artery after balloon dilation(DSA); F: the patent arteries bellow the knee(DSA). DSA: digital subtraction angiography
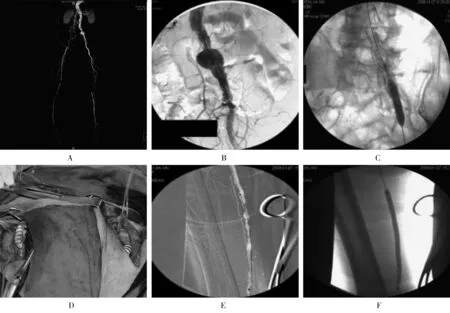
图3 D级主髂动脉病变合并C级股腘动脉病变杂交手术Figure 3 Hybrid surgery of type D aorto-iliac lesion and type C femoro-popliteal lesion
A: CT angiography shows occlusive lesions of the iliac and femoral artery associated with the left iliac atrey aneurysm; B: the left iliac artery aneurysm and occlusive lesion of the right iliac artery(DSA); C: balloon dilation after stent-graft of the left iliac artery; D: femoro-femoral bypass with prosthesis; E: stenosis and occlusion of the right femoral artery(DSA); F: balloon dilation of the femoral artery. DSA: digital subtraction angiography
2.2 围手术期情况
围术期并发症:1例股动脉穿刺点假性动脉瘤,行修补术;1例左侧臀部血肿,行臀下动脉栓塞术;无死亡病例。随访9~43(25.48±9.4)个月,失访2例,死亡2例。
2.3 患者ABI及通畅率
患者6、12、24和36个月ABI(0.91±0.16、0.85±0.14、0.82±0.17、0.77±0.13)比术前(0.47±0.24)均显著升高,差异有统计学意义(P<0.01);术后ABI有下降趋势,但差异无统计学意义(P>0.05)。术后12、24、36个月通畅率分别为95.7%、80.2%、72.9%(图5)。
3 讨 论
D级髂股动脉病变的特点是闭塞段长,多部位、多节段性病变,合并流出道和流入道病变,其术后通畅率要低于其他类型病变。流出道差是动脉重建后再狭窄的独立危险因素[8],通过杂交治疗能够改善流出道和流入道[9]。因此, 对于D级髂股动脉病变,要同期开通流入道或流出道,解决血流的高阻力,维持远期通畅。随着器材发展和腔内技术进步,D级病变开通成功率提高,文献报道其通畅率不亚于旁路手术,且并发症少于传统手术,提出修正TASCⅡ[10],但是缺乏大数据和随机对照试验支持,因此我们遵循TASCⅡ推荐,根据病变部位、程度和患者状况,选择合适的个体化治疗方案。患者术后1、2和3年通畅率分别达到95.7%、80.2%和72.9%,溃疡肢体愈合,静息痛消失,生活质量得到改善。
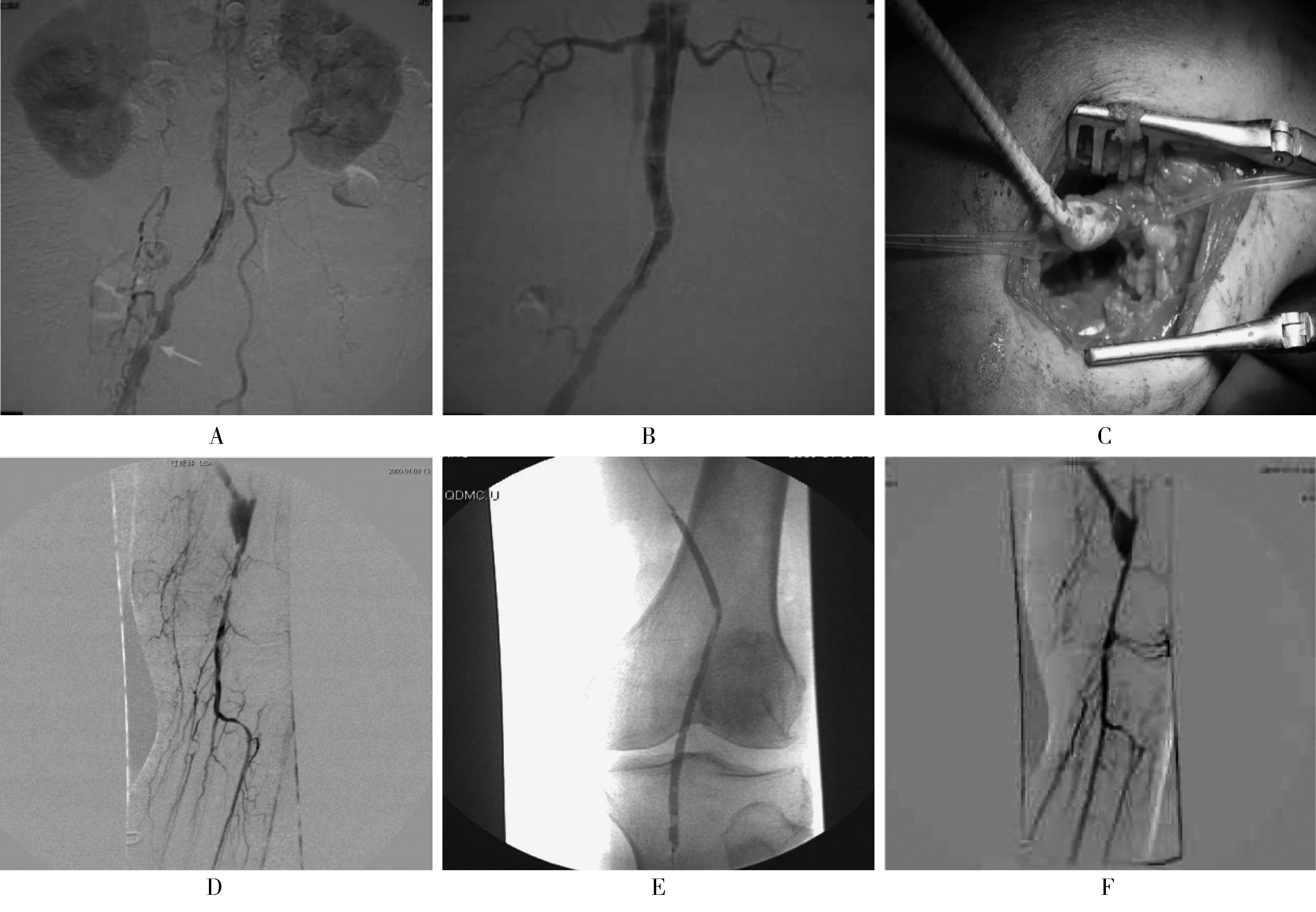
图4 D级主髂动脉病变合并D级股腘动脉病变杂交手术Figure 4 Hybrid surgery of type D aorto-iliac lesion and type D femoro-popliteal lesion
A: stenosis of the abdominal aortic and right iliac artery, occlusion of the left iliac artery(DSA); B: the patent abdominal aortic and right iliac artery after stenting(DSA); C: the anastomosis of the popliteal artery of femoro-popliteal bypass; D: severe stenosis of the popliteal artery distal to the anastomosis(DSA); E: balloon dilation of the popliteal artery; F: the patent popliteal and peroneal artery after balloon dilation(DSA). DSA: digital subtraction angiography
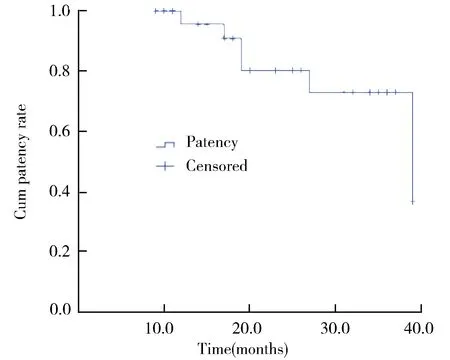
图5 D级髂股动脉病变患者术后通畅率Figure 5 The patency rate of type D iliac and femoral lesions after operation
对于D级主髂动脉病变,尽管主股动脉旁路通畅率高于腔内治疗和解剖外旁路(包括股股动脉旁路,腋股动脉旁路),但是创伤大,并发症多,死亡率高,不能及早恢复日常活动,本组病例为多节段D级病变,其他脏器血管如心、脑和肾存在不同程度病变,多不能耐受主股动脉旁路。因此,高龄、高危D级病变多选择单侧髂动脉支架置入、股股动脉旁路。部分C级、D级病变是动脉狭窄或闭塞基础上继发了血栓形成,缩小了动脉管径,增加了病变段长度,造成一种假象,应先行导管取栓,将其转变为B级,甚至A级病变,再行球囊扩张或支架植入。对于髂外动脉闭塞累及股总动脉的病变,行股动脉内膜剥脱。文献报道髂动脉闭塞杂交手术(髂动脉支架、股动脉内膜剥脱)住院时间短,并发症少,与开放手术相比,早期和远期效果类似,对于高危手术患者应当考虑杂交手术[11,12]。同时警惕髂动脉取栓、球囊扩张导致破裂可能,因此对于环状钙化,取栓过程中取出动脉内膜,首选植入覆膜支架[13]。
对于D级股腘动脉病变,首选股腘动脉旁路,大隐静脉作为旁路移植物远期通畅率高于人工血管,但是部分患者缺乏合适静脉移植物,创伤较大,且针对膝关节以上水平,人工血管通畅率达到了静脉移植物水平,因此我们采用袖状接头碳涂层人工血管,远端吻合口位于膝关节以上。对于合并膝下动脉病变,单纯股腘动脉旁路无法保证高的通畅率,需要同期开通膝下动脉,至少保证一条通畅的流出道血管[14,15]。吻合口处腘动脉严重狭窄,行内膜剥脱,吻合口远端腘动脉球囊扩张。股浅动脉闭塞,股深动脉开口或近段狭窄,导致通过侧支循环的血流减少,影响手术的通畅率,因此需行股深动脉成形来作为主髂动脉手术的流出道或股腘动脉旁路的流入道,其适用于股深动脉开口及近段狭窄、膝关节动脉网存在的患者。我们采取的手术方式是根据股深动脉狭窄长度,自股浅动脉开口以远切断,剥脱内膜,将股总、股深、股浅动脉“人”字形剖开,股深动脉成形,扩大股深动脉开口及起始段,增加股深动脉供血,通过其侧支提高肢体远端血流灌注压力,维持肢体存活的重要血供来源。
此外,术中直视下穿刺股动脉,为血管腔内治疗提供了便利,避免了邻近组织的损伤,减少穿刺引起的并发症。抗凝治疗至关重要,复杂D级病变合并流入道和流出道病变,流入血流慢,流出血流高阻力,导致血流淤滞,极易形成血栓,术中、术后均需要肝素抗凝治疗,预防血栓形成。若术中造影发现残存血栓,留置导管鞘、溶栓导管,泵入尿激酶,择期复查造影、二期处理。
复杂D级髂股动脉病变累及主髂动脉和股腘动脉,是多节段病变,需要同期处理流入道和流出道,以获得远期通畅。根据TASCⅡ推荐的治疗原则,术前评估患者的基础状态和病变的位置、范围、程度,选择合适的杂交治疗,降低麻醉和手术的打击,相对安全,中期效果好,尤其适合于下肢严重缺血、高龄、高危患者。
【参考文献】
[1] Diehm C, Schuster A, Allenberg JR,etal. High prevalence of peripheral arterial disease and co-morbidity in 6880 primary care patients: cross-sectional study[J]. Atherosclerosis, 2004, 172(1): 95-105. DOI: 10.1016/S0021-9150(03)00204-1.
[2] Karlstrom L, Bergqvist D. Effects of vascular surgery on amputation rates and mortality[J]. Eur J Vasc Endovasc Surg, 1997, 14(4): 273-283. DOI: 10.1016/S1078-5884(97)80239-0.
[3] Norgren L, Hiatt WR, Dormandy JA,etal. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC Ⅱ)[J]. Eur J Vasc Endovasc Surg, 2007, 33(Suppl 1): S1-S75. DOI: 10.1016/j.ejvs.2006.09.024.
[4] Sixt S, Rastan A, Beschorner U,etal. Acute and long-term outcome of Silverhawk assisted atherectomy for femoro-popliteal lesions according the TASC Ⅱ classification: a single-center experience[J]. Vasa, 2010, 39(3): 229-236. DOI: 10.1024/0301-1526/a000034.
[5] Jongsma H, Bekken JA, de Vries JP,etal. Drug-eluting balloon angioplastyversusuncoated balloon angioplasty in patients with femoropopliteal arterial occlusive disease[J]. J Vasc Surg, 2016, 64(5): 1503-1514. DOI: 10.1016/j.jvs.2016.05.084.
[6] Dippel EJ, Makam P, Kovach R,etal. Randomized controlled study of excimer laser atherectomy for treatment of femoropopliteal in-stent restenosis: initial results from the EXCITE ISR trial (Excimer laser randomized controlled study for treatment of femoropopliteal in-stent restenosis)[J]. JACC Cardiovasc Interv, 2015, 8(1 Pt A): 92-101. DOI: 10.1016/j.jcin.2014.09.009.
[7] Stanek F, Ouhrabkova R, Prochazka D. Percutaneous mechanical thrombectomy in the treatment of acute and subacute occlusions of the peripheral arteries and bypasses[J]. Vasa, 2016, 45(1): 49-56. DOI: 10.1024/0301-1526/a000495.
[8] Kavaliauskiene Z, Benetis R, Inciura D,etal. Factors affecting primary patency of stenting for Trans-Atlantic Inter-Society (TASC Ⅱ) type B, C, and D iliac occlusive disease[J]. Medicina, 2014, 50(5): 287-294. DOI: 10.1016/j.medici.2014.10.003.
[9] Taurino M, Persiani F, Fantozzi C,etal. Trans-Atlantic Inter-Society Consensus Ⅱ C and D iliac lesions can be treated by endovascular and hybrid approach: a single-center experience[J]. Vasc Endovasc Surg, 2014, 48(2): 123-128. DOI: 10.1177/1538574413512381.
[10] Lun Y, Zhang J, Wu XY,etal. Comparison of midterm outcomes between surgical treatment and endovascular reconstruction for chronic infrarenal aortoiliac occlusion[J]. J Vasc Interv Radiol, 2015, 26(2): 196-204. DOI: 10.1016/j.jvir.2014.10.018.
[11] Piazza M, Ricotta JJ, Bower TC,etal. Iliac artery stenting combined with open femoral endarterectomy is as effective as open surgical reconstruction for severe iliac and common femoral occlusive disease[J]. J Vasc Surg, 2011, 54(2): 402-411. DOI: 10.1016/j.jvs.2011.01.027.
[12] Maitrias P, Deltombe G, Molin V,etal. Iliofemoral endarterectomy associated with systematic iliac stent grafting for the treatment of severe iliofemoral occlusive disease[J]. J Vasc Surg, 2017, 65(2): 406-413. DOI: 10.1016/j.jvs.2016.07.130.
[13] Psacharopulo D, Ferrero E, Ferri M,etal. Increasing efficacy of endovascular recanalization with covered stent graft for Trans-Atlantic Inter-Society Consensus Ⅱ D aortoiliac complex occlu-sion[J]. J Vasc Surg, 2015, 62(5): 1219-1226. DOI: 10.1016/j.jvs.2015.06.218.
[14] Dougherty MJ, Young LP, Calligaro KD. One hundred twenty-five concomitant endovascular and open procedures for lower extremity arterial disease[J]. J Vasc Surg, 2003, 37(2): 316-322. DOI: 10.1067/mva.2003.116.
[15] Controneo AR, Lezzi R, Marano G,etal. Hybrid therapy in patients with complex peripheral multifocal steno-obstructive vascular disease: two-year results[J]. Cardiovasc Intervent Radiol, 2007, 30(3): 355-361. DOI: 10.1007/s00270-005-0296-5.