慢性肾脏病各分期患者矿物质骨代谢指标变化特征研究
胡丽莉,涂卫平,房向东,徐承云
·论著·
慢性肾脏病各分期患者矿物质骨代谢指标变化特征研究
胡丽莉,涂卫平,房向东,徐承云*
目的 分析慢性肾脏病(CKD)1~5期患者矿物质骨代谢指标变化特征,为早期CKD患者矿物质骨代谢的治疗提供依据。方法 回顾性选取2013年在南昌大学第二附属医院肾内科住院且符合纳入标准的391例CKD患者的临床资料,依据肾脏病预后质量倡议(KDOQI)指南推荐的CKD分期标准将患者分为CKD 1~2期32例(CKD 1~2期组)、CKD 3期67例(CKD 3期组)、CKD 4期79例(CKD 4期组)、CKD 5期213例(CKD 5期组)。比较4组患者一般资料(性别、年龄、糖尿病发生率)、血肌酐、估算肾小球滤过率(eGFR)、矿物质骨代谢指标{血钙、血磷、血钙磷乘积、全段甲状旁腺激素(iPTH)、25羟维生素D3〔25(OH)D3〕、骨型碱性磷酸酶(BSALP)、骨钙素};分析CKD患者eGFR、部分矿物质骨代谢指标〔iPTH、25(OH)D3、BSALP、骨钙素〕的相关性;并计算CKD 3、4、5期组患者血钙、血磷、血钙磷乘积、iPTH达标率(达标率均参照KDOQI指南推荐的CKD患者矿物质骨代谢指标参考范围)。结果 CKD 3期组患者25(OH)D3低于CKD 1~2期组(P<0.05);CKD 4期组患者血磷、血钙磷乘积、iPTH、BSALP高于CKD 1~2期组,25(OH)D3低于CKD 1~2期组和CKD 3期组,骨钙素高于CKD 1~2期组和CKD 3期组(P<0.05); CKD 5期组患者血钙低于CKD 1~2期组、CKD 3期组、CKD 4期组,血磷、血钙磷乘积、iPTH、骨钙素高于CKD 1~2期组、CKD 3期组、CKD 4期组,25(OH)D3低于CKD 1~2期组和CKD 3期组,BSALP高于CKD 1~2期组、CKD 3期组(P<0.05)。eGFR与iPTH、BSALP、骨钙素呈负相关(r值分别为-0.49、-0.18、-0.43,P<0.05),与25(OH)D3呈正相关(r=0.34,P<0.05);iPTH与25(OH)D3呈负相关(r=-0.17,P<0.05),与BSALP、骨钙素呈正相关(r值分别为0.34、0.60,P<0.05);25(OH)D3与骨钙素呈负相关(r=-0.11,P<0.05),25(OH)D3与BSALP无直线相关关系(r=-0.10,P>0.05);BSALP与骨钙素呈正相关(r=0.25,P<0.05)。CKD 3、4、5期组患者血钙达标率分别为86.6%(58/67)、79.7%(63/79)和37.6%(80/213);CKD 3、4、5期组患者血磷达标率分别为82.1%(55/67)、69.6%(55/79)、46.0%(98/213);CKD 3、4、5期组患者血钙磷乘积达标率分别为100.0%(67/67)、97.5%(77/79)、76.5%(163/213);CKD 3、4、5期组患者iPTH达标率分别为43.3%(29/67)、26.6%(21/79)、39.0%(83/213)。CKD 3、4、5期组患者各项指标均达标的达标率分别为31.3%(21/67)、19.0%(15/79)、11.7%(25/213)。结论 早、中期CKD患者已存在矿物质骨代谢指标异常,且随着肾功能的恶化,iPTH、BSALP、骨钙素均有不同程度的升高;血钙、血磷在CKD 4~5期变化明显;CKD 1~5期患者普遍存在25(OH)D3不足和缺乏现象,CKD 3~5期患者矿物质骨代谢指标符合KDOQI指南推荐参考范围的达标率很低,特别是iPTH。
肾病;慢性病;矿物质骨代谢
胡丽莉,涂卫平,房向东,等.慢性肾脏病各分期患者矿物质骨代谢指标变化特征研究[J].中国全科医学,2017,20(12):1434-1438.[www.chinagp.net]
HU L L,TU W P,FANG X D,et al.Changing characteristics of mineral and bone metabolism indicators in patients with chronic kidney disease at different stages[J].Chinese General Practice,2017,20(12):1434-1438.
近十几年来慢性肾脏病(CKD)发病率大幅度升高。在CKD早期阶段,患者的死亡风险远超过疾病进展至终末期肾脏病(ESRD)[1],且心血管事件是CKD患者最重要的死亡原因。大量研究表明,CKD患者矿物质骨代谢指标异常是心血管事件的危险因素[2-7]。矿物质骨代谢指标主要包括血钙、血磷、全段甲状旁腺激素(iPTH)、维生素D等,其异常改变易引起心血管及软组织钙化,加重CKD患者心血管病变[3]。高磷血症是CKD患者病死率增加的危险因素[4]。骨型碱性磷酸酶(BSALP)水平与早期CKD患者心血管事件发病率和病死率相关[5-6]。25羟维生素D3〔25(OH)D3〕缺乏是CKD患者病死率增加的危险因素[7]。为了更好的治疗CKD患者矿物质骨代谢指标异常及其并发症,肾脏病预后质量倡议(KDOQI)指南推荐了CKD 3~5期患者血钙、血磷、血钙磷乘积及iPTH等指标的控制范围[8];而在国外研究中CKD 1~5期患者符合KDOQI指南推荐范围的百分比很低[9]。目前国内有关透析前CKD患者矿物质骨代谢指标的研究很少,本研究旨在观察CKD 1~5期患者矿物质骨代谢指标的变化特征,为早期CKD患者的临床治疗提供理论依据。
1 对象与方法
1.1 纳入与排除标准 纳入标准:(1)血钙、血磷、iPTH、25(OH)D3、BSALP及骨钙素等临床资料完整者;(2)年龄≥18岁者。排除标准:(1)原发性甲状旁腺功能亢进者;(2)恶性疾病或肝功能损伤者;(3)3个月内服用钙剂、维生素D及磷结合剂者;(4)正在行透析治疗或有肾移植史者;(5)急性肾衰竭、大量蛋白尿者。
1.2 研究对象 回顾性选取2013年在南昌大学第二附属医院肾内科住院且符合纳入标准的391例CKD患者的临床资料,其中原发性肾小球病143例(36.6%),继发性肾脏病164例(41.9%),肾小管间质病18例(4.6%),多囊肾20例(5.1%),其他慢性肾脏病(遗传性肾脏病、尿路感染等)32例(8.2%),病因不明14例(3.6%)。本研究经南昌大学第二附属医院伦理委员会批准。
1.3 CKD诊断标准及分期 CKD诊断标准及分期参照KDOQI指南进行判定[3],并采用肾脏病饮食改良(MDRD)简化公式计算估算肾小球滤过率(eGFR)。CKD 1期eGFR≥90 ml·min-1·(1.73 m2)-1,CKD 2期eGFR 60~89 ml·min-1·(1.73 m2)-1,CKD 3期eGFR 30~59 ml·min-1·(1.73 m2)-1,CKD 4期eGFR 15~29 ml·min-1·(1.73 m2)-1,CKD 5期eGFR<15 ml·min-1·(1.73 m2)-1。本文血钙均为校正钙〔校正钙(mg/dl)=钙+0.8×(4.0-清蛋白)〕。
KDOQI指南推荐的CKD患者矿物质骨代谢指标参考范围[3]:(1)CKD 3~4期血钙8.5~10.2 mg/dl,CKD 5期血钙8.4~9.5 mg/dl。(2)CKD 3~4期血磷2.7~4.6 mg/dl,CKD 5期血磷3.5~5.5 mg/dl。(3)CDK 3~5期血钙磷乘积≤55 mg2/dl2。(4)CKD 3期iPTH 35~70 ng/L,CKD 4期iPTH 71~110 ng/L,CKD 5期iPTH 150~300 ng/L。(5)25(OH)D3在15~30 μg/L示维生素D不足,25(OH)D3<15 μg/L示维生素D缺乏,25(OH)D3<7 μg/L示维生素D严重缺乏。CKD各分期患者血钙、血磷、血钙磷乘积、iPTH符合KDOQI指南推荐的参考范围则记为达标。
1.4 方法 依据KDOQI指南推荐的CKD分期将患者分为CKD 1~2期32例(CKD 1~2期组)、CKD 3期67例(CKD 3期组)、CKD 4期79例(CKD 4期组)、CKD 5期213例(CKD 5期组),比较4组患者的一般资料(性别、年龄、糖尿病发生率)、血肌酐、eGFR、矿物质骨代谢指标〔血钙、血磷、血钙磷乘积、iPTH、25(OH)D3、BSALP、骨钙素〕;分析CKD患者eGFR、部分矿物质骨代谢指标〔iPTH、25(OH)D3、BSALP、骨钙素〕间的相关性;计算CKD 3、4、5期组患者血钙、血磷、血钙磷乘积、iPTH达标率。

2 结果
2.1 4组患者一般资料、血肌酐、eGFR、矿物质骨代谢指标比较 4组患者性别、年龄、糖尿病发生率比较,差异无统计学意义(P>0.05)。4组患者血肌酐、eGFR、血钙、血磷、血钙磷乘积、iPTH、25(OH)D3、BSALP、骨钙素比较,差异有统计学意义(P<0.05);其中CKD 3期组患者25(OH)D3低于CKD 1~2期组,差异有统计学意义(P<0.05);CKD 4期组患者血磷、血钙磷乘积、iPTH、BSALP高于CKD 1~2期组,25(OH)D3低于CKD 1~2期组和CKD 3期组,骨钙素高于CKD 1~2期组和CKD 3期组,差异有统计学意义(P<0.05);CKD 5期组患者血钙低于CKD 1~2期组、CKD 3期组、CKD 4期组,血磷、血钙磷乘积、iPTH、骨钙素高于CKD 1~2期组、CKD 3期组、CKD 4期组,25(OH)D3低于CKD 1~2期组和CKD 3期组,BSALP高于CKD 1~2期组和CKD3期组,差异有统计学意义(P<0.05,见表1)。
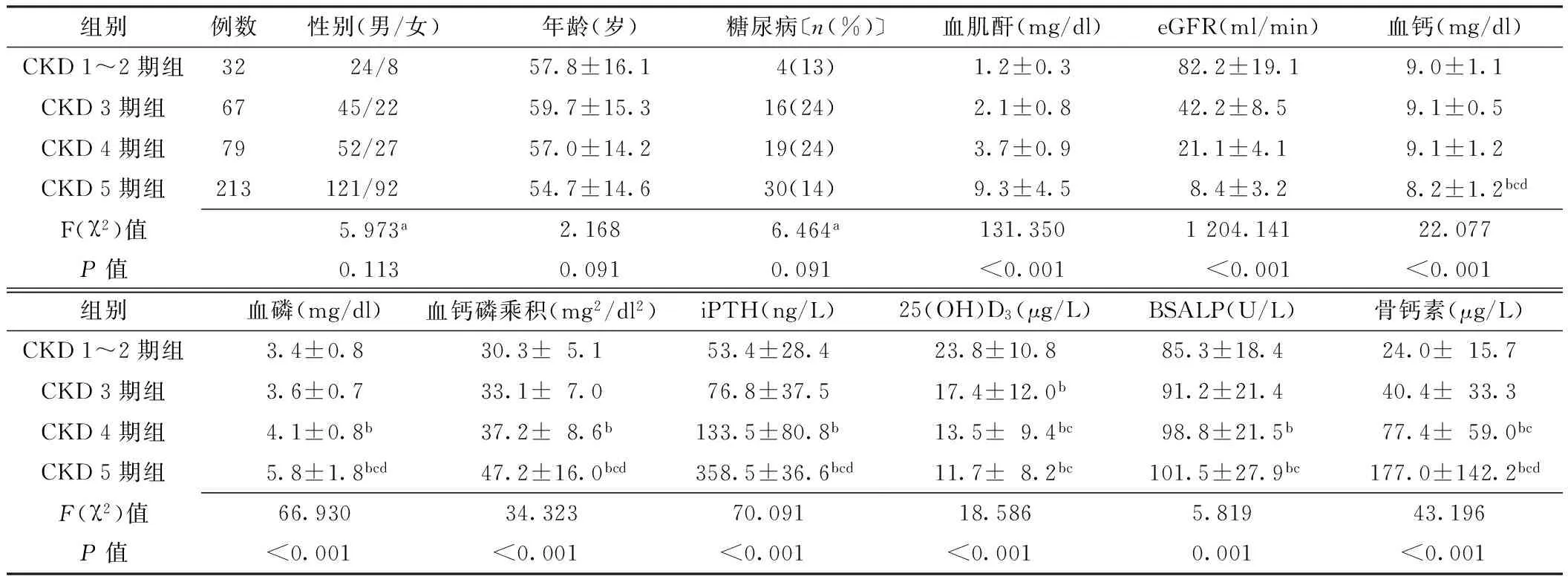
表1 4组患者一般资料、血肌酐、eGFR、矿物质骨代谢指标比较
注:a为χ2值;与CKD 1~2期组比较,bP<0.05;与CKD 3期组比较,cP<0.05;与CKD 4期组比较,dP<0.05;eGFR=估算肾小球滤过率,iPTH=全段甲状旁腺激素,25(OH)D3=25羟维生素D3,BSALP=骨型碱性磷酸酶,CKD=慢性肾脏病
2.2 CKD患者eGFR、部分矿物质骨代谢指标〔iPTH、25(OH)D3、BSALP、骨钙素〕的相关性分析 eGFR与iPTH、BSALP、骨钙素呈负相关(r值分别为-0.49、-0.18、-0.43,P<0.05),与25(OH)D3呈正相关(r=0.34,P<0.05);iPTH与25(OH)D3呈负相关(r=-0.17,P<0.05),与BSALP、骨钙素呈正相关(r值分别为0.34、0.60,P<0.05);25(OH)D3与骨钙素呈负相关(r=-0.11,P<0.05),25(OH)D3与BSALP无直线相关关系(r=-0.10,P>0.05);BSALP与骨钙素呈正相关(r=0.25,P<0.05)。2.3 CKD 3、4、5期组患者血钙、血磷、血钙磷乘积、iPTH达标率 CKD 3、4、5期组患者血钙达标率分别为86.6%(58/67)、79.7%(63/79)和37.6%(80/213);CKD 3、4、5期组患者血磷达标率分别为82.1%(55/67)、69.6%(55/79)、46.0%(98/213);CKD 3、4、5期组患者血钙磷乘积达标率分别为100.0%(67/67)、97.5%(77/79)、76.5%(163/213);CKD 3、4、5期组患者iPTH达标率分别为43.3%(29/67)、26.6%(21/79)、39.0%(83/213)。CKD 3、4、5期组患者各项指标均达标的达标率分别为31.3%(21/67)、19.0%(15/79)、11.7%(25/213)。
3 讨论
由CKD导致的血钙、血磷代谢异常,继发性甲状旁腺功能亢进,骨骼成分及结构改变,会引起或加重血管及软组织钙化,是CKD的常见并发症,不仅严重影响患者的生活质量,还与其病死率的增加密切相关。与发达国家相比,我国CKD防治工作比较滞后,有关透析前期CKD患者矿物质骨代谢的研究也很少,对该病的认知率、治疗率以及患者各指标达标率均较低[9-11];本研究对CKD各分期患者矿物质骨代谢指标变化进行了更全面深入的分析,其中部分研究结果证实了以前的研究结论[9-11],此外还另有发现,主要为:(1)CKD分期越高的患者,其iPTH和骨钙素升高越明显,且两者呈正相关;BSALP上升缓慢;(2)CKD各分期患者普遍存在25(OH)D3不足和缺乏的现象;CKD 5期患者血钙、血磷达标率较低,应在CKD早期阶段进行密切监测并给予相应治疗,降低CKD患者肾性骨病或心血管疾病的发生率。
KDOQI指南建议BSALP水平可作为评估骨代谢状态的补充检测方法[3]。BSALP由成骨细胞分泌并释放入血,参与骨矿化过程。越来越多的证据表明,血清BSALP水平是反映骨组织形态学改变的较敏感指标,与患者的临床预后关系密切[5-6,12]。本研究对CKD各分期患者BSALP进行统计分析,发现其与iPTH、骨钙素的快速变化不同;随着肾功能的恶化,BSALP上升缓慢,与RIX等[11]研究结果一致。血钙、血磷的变化会引起iPTH的快速反应,但是BSALP的变化与骨重塑有关,而骨重塑过程缓慢;此外,BSALP的t1/2为1~2 d,而iPTH仅为2~5 min[12]。以上分析可解释本研究中BSALP变化相对滞后的原因。
本研究结果显示,CKD各期患者普遍存在25(OH)D3不足和缺乏的现象,且随着eGFR下降,25(OH)D3下降明显;推测CKD早期患者25(OH)D3不足的高流行性与阳光照射、饮食因素、蛋白尿等因素有关;但是随着肾功能的恶化,25(OH)D3缺乏甚至严重缺乏的情况明显增加,一定程度上证实肾脏疾病是25(OH)D3降低的危险因素。有研究发现,尿毒症毒素可直接抑制维生素D的光转换作用和肝脏的羟基化作用[13-14]。25(OH)D3缺乏是CKD患者心血管疾病和全因病死率增加的危险因素[7,15]。CKD 3~4期患者补充维生素D可降低26%的死亡风险或延迟患者进入透析阶段[16]。因此,建议在CKD早期阶段定期监测患者25(OH)D3,并进行相应的补充治疗。
国外大样本量研究显示,CKD 3~5期患者矿物质骨代谢指标符合KDOQI指南推荐范围,其中血钙达标率分别为90.7%、85.6%、55.0%;血磷达标率分别为90.9%、77.1%、70.3%;iPTH达标率分别为42.4%、24.6%、46.8%;血钙磷乘积达标率分别为99.9%、99.6%、83.8%[9]。本研究中CKD 3~4期患者矿物质骨代谢指标达标率与上述研究结果接近,但是CKD 5期患者血钙、血磷达标率(37.6%、46.0%)远低于CRAVER等[9]的研究结果(血钙、血磷达标率分别为55.0%、70.3%)。研究显示,高磷血症是CKD患者病死率增加和肾功能下降的独立危险因素[4]。一项Meta分析结果显示,CKD患者血磷水平增加1.0 mg/dl,其死亡风险增加18%〔RR=1.18,95%CI(0.12,1.25)〕[17]。分析国内CKD 5期患者低钙血症、高磷血症问题较国外突出的原因包括:(1)饮食中磷的摄入量过多,国内大多数医院没有营养师对CKD患者的饮食进行健康指导;(2)大多数CKD患者的随访时间并未参照KDOQI指南的建议,至少间隔1年以上。提示临床应对透析前期CKD患者血钙、血磷水平进行密切监测并给予相应的治疗。CKD 3~5期患者iPTH符合KDOQI指南推荐范围,达标率分别为43.3%、26.6%、39.0%,与CRAVER等[9](42.4%、24.6%、46.8%)和RIX等[11](37.0%、23.0%、39.0%)的研究数据相近。BHURIYA等[18]研究发现,iPTH>70 ng/L的CKD 3~4期患者心血管事件发生率增加。因此,临床应尽早综合评估CKD患者的血钙、血磷、维生素D、iPTH,并给予相应治疗。
综上所述,早、中期CKD患者已存在矿物质骨代谢紊乱;CKD 1~5期患者25(OH)D3不足和缺乏问题异常严峻,CKD 3~5期患者矿物质骨代谢指标符合KDOQI指南推荐参考范围的达标率很低,应在CKD早期阶段进行密切监测并给予相应治疗,降低早期CKD患者心血管事件发生风险。
作者贡献:胡丽莉进行资料收集整理、撰写论文并对文章负责;涂卫平、房向东进行试验设计及评估;徐承云进行质量控制及审校。
本文无利益冲突。
本研究不足之处:
本研究仅是对单中心慢性肾脏病 1~5期患者矿物质骨代谢指标进行了统计分析,且样本量较小,尚需进行多中心大样本量的进一步研究。
[1]KEITH D S,NICHOLS G A,GULLION C M,et al.Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization[J].Arch Intern Med,2004,164(6):659-663.
[2]DANESE M D,BELOZEROFF V,SMIRNAKIS K,et al.Consistent control of mineral and bone disorder in incident hemodialysis patients[J].Clin J Am Soc Nephrol,2008,3(5):1423-1429.DOI:10.2215/CJN.01060308.Epub 2008 Jul 2.
[3]MOE S,DRÜEKE T,CUNNINGHAM J,et al.Definition,evaluation,and classification of renal osteodystrophy:a position statement from kidney disease:Improving Global Outcomes(KDIGO) [J].Kidney Int,2006,69(1):1945-1953.
[4]KESTENBAUM B,SAMPSON J N,RUDSER K D,et al.Serum phosphate levels and mortality risk among people with chronic kidney disease[J].J Am Soc Nephrol,2005,16(2):520-528.Epub 2004 Dec 22.
[5]FAHRLEITNER-PAMMER A,HERBERTH J,BROWNING S R,et al.Bone markers predict cardiovascular events in chronic kidney disease[J].J Bone Miner Res,2008,23(11):1850-1858.DOI:10.1359/jbmr.080610.
[6]KOVESDY C P,URECHE V,LU J L,et al.Outcome predictability of serum alkaline phosphatase in men with pre-dialysis CKD[J].Nephrol Dial Transplant,2010,25(9):3003-3011.DOI:10.1093/ndt/gfq144.Epub 2010 Mar 17.
[7]NAVANEETHAN S D,SCHOLD J D,ARRIGAIN S,et al.Low 25 hydroxyvitamin D levels and mortality in non-dialysis dependent CKD[J].Am J Kidney Dis,2011,58(4):536-543.DOI:10.1053/j.ajkd.2011.04.028.Epub 2011 Aug 4.
[8]LEVEY A S,CORESH J.Should the K/DOQI definition of chronic kidney disease be changed? [J].Am J Kidney Dis,2003,42(4):626-630.
[9]CRAVER L,MARCO M P,MARTNEZ I,et al.Mineral metabolism parameters throughout chronic kidney disease stages 1-5-achievement of KDOQI target ranges[J].Nephrol Dial Transplant,2007,22(4):1171-1176.Epub 2007 Jan 5.
[11]RIX M,ANDREASSEN H,ESKILDSEN P,et al.Bone mineral density and biochemical markers of bone turnover in patients with predialysis chronic renal failure[J].Kidney Int,1999,56(3):1084-1093.
[12]SARDIWAL S,MAGNUSSON P,GOLDSMITH D J,et al.Bone alkaline phosphatase in CKD-mineral bone disorder[J].Am J Kidney Dis,62(4):810-822.DOI:10.1053/j.ajkd.2013.02.366.Epub 2013 Apr 23.
[13]ROJAS-RIVERA J,DE LA P C,RAMOS A,et al.The expanding spectrum of biological actions of vitamin D[J].Nephrol Dial Transplant,2010,25(9):2850-2856.DOI:10.1093/ndt/gfq313.Epub 2010 Jun 3.
[14]MICHAUD J,NAUD J,OUIMET D,et al.Reduced hepatic synthesis of calcidiol in uremia[J].J Am Soc Nephrol,2010,21(9):1488-1497.DOI:10.1681/ASN.2009080815.Epub 2010 Jul 1.
[15]PETCHEY W G,HOWDEN E J,JOHNSON D W,et al.Cardiorespiratory fitness is independently associated with 25-hydroxyvitamin D in chronic kidney disease[J].Clin J Am Soc Nephrol,2011,6(3):512-518.DOI:10.2215/CJN.06880810.Epub 2010 Dec 16.
[16]SHOBEN A B,RUDSER K D,DE BOER I H,et al.Association of oral calcitriol with improved survival in nondialyzed CKD[J].J Am Soc Nephrol,2008,19(8):1613-1619.DOI:10.1681/ASN.2007111164.Epub 2008 May 7.
[17]PALMER S C,HAYEN A,MACASKILL P,et al.Serum levels of phosphorus,parathyroid hormone,and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease:a systematic review and meta-analysis[J].JAMA,2011,305(11):1119-1127.DOI:10.1001/jama.2011.308.
[18]BHURIYA R,LI S,CHEN S C,et al.Plasma parathyroid hormone level and prevalent cardiovscular disease in CKD stages 3 and 4:an analysis from the Kidney Early Evaluation Program(KEEP) [J].Am J Kidney Dis,2009,53(4 Suppl 4):S3-10.DOI:10.1053/j.ajkd.2008.11.029.
(本文编辑:毛亚敏)
Changing Characteristics of Mineral and Bone Metabolism Indicators in Patients with Chronic Kidney Disease at Different Stages
HULi-li,TUWei-ping,FANGXiang-dong,XUCheng-yun*
DepartmentofNephrology,theSecondAffiliatedHospitalofNanchangUniversity,Nanchang330006,China
*Correspondingauthor:XUCheng-yun,Associatechiefphysician;E-mail:183207745@qq.com
Objective To analyze the changing characteristics of mineral and bone metabolism indicators in patients with chronic kidney disease(CKD) at stage 1 to stage 5 and to provide basis for treatment of patients with CKD in early stages.Methods According to the inclusion criteria,391 patients with CKD hospitalized in Department of Nephrology of the Second Affiliated Hospital of Nanchang University in 2013 were enrolled and their clinical data were collected retrospectively.On the basis of CKD staging in kidney disease outcomes quality initiative(KDOQI) guidelines,patients were divided into CKD of stage 1 to 2 group(n=32),CKD of stage 3 group(n=67),CKD of stage 4 group(n=79),and CKD of stage 5 group(n=213).Comparison of 4 groups of patients with the general information(gender,age,incidence of diabetes mellitus),serum creatinine,estimated glomerular filtration rate(eGFR) and mineral and bone metabolism indicators {serum calcium,serum phosphorus and serum calcium-phosphorus product,intact parathyroid hormone(iPTH),25-hydroxyvitamin D3〔25(OH) D3〕,bone-specific alkaline phosphatase(BSALP),osteocalcin}of patients in 4 groups were compared;the correlation between eGFR and partial indicators of mineral and bone metabolism 〔iPTH,25(OH) D3,BSALP,osteocalcin〕 of patients with CKD was analyzed;and the qualified rate of serum calcium,serum phosphorus,calcium-phosphorus product,iPTH(qualified rate referred to the reference range of mineral and bone metabolic indicators of CKD patients recommended in KDOQI guidelines ) among CKD of stage 3,stage 4 and stage 5 groups were calculated.Results The 25(OH)D3of CKD of stage 3 group was lower than that of CKD of stage 1 to 2 group(P<0.05);the serum phosphorus,serum calcium-phosphorus product,iPTH,BSALP of CKD of stage 4 group were higher than that of CKD of stage 1 to 2 group,its 25(OH)D3of was lower and osteocalcin was higher than that of CKD of stage 1 to 2 group and CKD of stage 3 group(P<0.05).Serum calcium of CKD of stage 5 group was lower than that of the other 3 groups,while its serum phosphorus,serum calcium-phosphorus product,iPTH,osteocalcin were higher than that of the other 3 groups,and its 25(OH)D3was lower than that of CKD of stage 1 to 2 group and CKD of stage 3 group,while BSALP was higher than that of the above 2 groups(P<0.05).eGFR was negatively correlated with iPTH,BSALP,osteocalcin(r=-0.49,-0.18,-0.43 respectively,P<0.05),and positively correlated with 25(OH)D3(r=0.34,P<0.05).iPTH was negatively correlated with 25(OH)D3(r=-0.17,P<0.05),and positively correlated with BSALP,osteocalcin(r=0.34,0.60 respectively,P<0.05).25(OH)D3was negatively correlated with osteocalcin(r=-0.11,P<0.05) and not correlated with and BSALP(r=-0.10,P>0.05).BSALP was positively correlated with osteocalcin(r=0.25,P<0.05).The qualified rate of serum calcium of patients in CKD of stage 3,CKD of stage 4 and CKD of stage 5 groups was 86.6%(58/67),79.7%(63/79) and 37.6%(80/213) respectively,the qualified rate of serum phosphorus of patients in the above 3 groups was 82.1%(55/67),69.6%(55/79),46.0%(98/213);their qualified rate of serum calcium-phosphorus product was 100.0%(67/67),97.5%(77/79),76.5%(163/213) respectively,and their qualified rate of iPTH was 43.3%(29/67),26.6%(21/79),39.0%(83/213) respectively.The qualified rate of each indicator reaching the standard of patients in CKD of stage 3,CKD of stage 4 and CKD of stage 5 groups was 31.3%(21/67),19.0%(15/79),11.7%(25/213) respectively.Conclusion There have been abnormal mineral metabolism indicators in the early and middle stage of patients with CKD.Moreover,with the deterioration of renal function,iPTH,BSALP,osteocalcin have all increased at different degrees.There are obvious changes in serum calcium and serum phosphate in CKD of stage 4 to 5.The phenomenon of insufficient 25(OH)D3is prevailing in CKD of stage 1 to 5 among patients with CKD.The qualified rate of indicators of mineral and bone metabolism is very low,especially iPTH,which accords with the reference range of KDOQI guidelines.
Nephrosis;Chronic disease;Mineral and bone metabolism
R 692
A
10.3969/j.issn.1007-9572.2017.12.006
2016-12-12;
2017-03-02)
330006江西省南昌市,南昌大学第二附属医院肾脏科
*通信作者:徐承云,副主任医师;E-mail:183207745@qq.com

