高频彩色多普勒超声在诊断小儿胆道闭锁中的应用
杜妍妍 符柳江 张向向 王红英
高频彩色多普勒超声在诊断小儿胆道闭锁中的应用
杜妍妍 符柳江 张向向 王红英
目的 分析儿童胆道闭锁中的超声图像特征,探讨高频彩色多普勒超声在早期诊断胆道闭锁中的应用价值。方法回顾性分析46例经手术及病理确诊的胆道闭锁患儿术前超声图像资料,结合术中病理结果,分析高频彩色多普勒超声时提示肝脏大小及内回声情况,胆囊显示率及胆囊大小、形态,肝门区结构,肝动脉内径及血流频谱特征的作用,评估其早期诊断价值。结果术前超声提示肝脏形态增大,肝内回声改变24例(52%),胆囊长径<15 mm 20例,胆囊长径>15 mm 18例,胆囊未显示2例,胆囊显示欠清(考虑裂隙样胆囊)6例。超声提示肝门部纤维块42例,2例MRI提示胆道闭锁,2例超声提示肝门部小囊腔。肝动脉内径2.2~2.8 mm,均值2.4 mm。肝动脉频谱为高速高阻血流,PSV:77~123 cm/s,RI:0.89~0.96。结论胆囊形态及肝门部纤维块是超声诊断胆道闭锁的重要征象,综合分析肝脏形态及肝动脉内径与频谱特征对早期诊断小儿胆道闭锁具有一定价值。
高频彩色多普勒超声;胆道闭锁;胆囊;肝门部纤维块;肝脏形态;肝动脉
胆道闭锁(biliary atresia,BA)的病因和发病机 制不明,是先天性发育障碍所致的胆道梗阻,病变多累及整个胆道,也可仅累及部分胆管[1]。是小婴儿阻塞性黄疸的主要病因,早期与婴儿肝炎综合征较难鉴别,晚期可出现胆汁性肝硬化,愈后较差。尽早明确诊断,早期手术对胆道闭锁的愈后至关重要[2]。本研究回顾性分析46例经手术及病理检查确诊的胆道闭锁患儿术前超声图像资料,探讨高频超声检查在早期诊断胆道闭锁中的价值。
材料与方法
一、研究对象
回顾性分析2014年1月至2014年12月由本院诊断并经手术及病理检查确诊的胆道闭锁患儿46例,其中男性26例,女性20例,年龄30~121 d,平均年龄56 d。临床表现为黄疸进行性加重,伴有淡黄色甚至白陶土样大便,疑诊为阻塞性黄疸。均于术前行常规超声检查,图像资料完整。
二、仪器及方法
采用 TOSHIBA SSA-790A和 SIEMENS ACUSON2000型彩色多普勒超声诊断仪,高频线阵探头频率10~12 MHz。检查方法:检查当日空腹4~6 h,哭闹不合作时给予患儿口服10%水合氯醛,剂量为0.7 mL/kg,行术前肝胆常规超声检查,观察肝脏大小及内部回声,胆囊形态及大小,肝动脉内径及频谱测量,重点观察肝门部纤维块情况。
结果
一、肝脏大小及内部回声
24例提示肝脏增大,内回声增粗,其中2例可见少量腹腔积液。22例超声检查肝脏未见明显异常。术后病理检查结果:16例提示肝脏早期损害,30例提示肝脏中期损害。
二、胆囊大小及形态,空腹及餐后半小时变化
2例未见胆囊(胆囊不显示),6例胆囊呈裂隙状,20例小胆囊(胆囊长径<1.5 cm),18例大胆囊(胆囊长径>1.5 cm),形态僵硬,不规则,餐后半小时胆囊大小无明显改变。其中6例可见肝门区小囊。术后病理检查结果:36例胆囊发育不良。
三、肝门部纤维块
42例超声检查可见肝门部纤维块,2例MRI提示BA,2例提示肝门区小囊腔。
16例患儿测量肝动脉内径2.2~2.8 mm,均值2.4 mm。肝动脉频谱为高速高阻血流,PSV77~123 cm/s,RI:0.89~0.96。
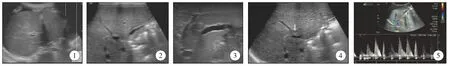
图1 肝内回声增粗,肝周可见积液暗区; 图2 胆囊形态小,长径<15 mm; 图3 胆囊长径>15 mm,形态僵硬; 图4肝门部纤维块; 图5 肝动脉频谱高速高阻Fig.1 Asperous echogenicity of the liver,and ascites around the liver; Fig.2 The morphology of gallbladder is small,and length<15 mm; Fig.3 Gallbladder length>15 mm,morphological stiffness; Fig.4 Hepatic portal fibrosis; Fig.5 High speed and high resistance of hepatic artery
讨论
BA的确切病因至今尚不清楚,单纯依靠超声图像与婴儿肝炎综合征进行鉴别较为困难,这两种疾病在治疗上出入较大,早期诊断,尽早手术,避免出现肝脏严重损害时贻误手术时机。早在1996年,Choi SO等[3]报道了BA的一个重要超声特征:肝门或左、右肝管汇合部有无团块状或索带状高回声区,即TC征。认为TC征在诊断BA中有很高的敏感性和特异性。随后,这一团队就TC征在BA诊断中的价值及与胆汁淤积等的鉴别,超声与核素扫描及肝脏针吸活检在诊断BA中的作用等进行了一系列对比研究,认为超声是最优的检查方法[4-6]。但也发现其他原因引起门静脉周围水肿或增厚而出现假阳性TC征[4]。在本组病例的回顾性分析中发现,早期的TC征其实较难明确诊断,多于复查或病情发展后发现。
作者结合本组病例的声像图发现,所有病例的胆囊均发育异常,少数病例胆囊先天缺如,多数病例空腹时胆囊形态小,胆囊腔内无回声区未能显示。即使胆囊大小正常,有胆囊腔存在,但胆囊的形态僵硬且不规则,餐后胆囊大小与形态无明显改变。因此,胆囊明显狭小、形态不规则、胆囊壁黏膜线消失,胆囊呈索条状或消失在诊断BA上具有很高的敏感性,该结果与TanKendrick AP等[7]研究一致。王晓曼等[8]认为,胆囊形态是超声诊断BA的重要征象,合并肝门区小囊肿则可确诊为胆道闭锁。本组病例两例发现肝门部小囊腔,其中1例外院诊断胆总管囊肿,本院复查后发现胆囊形态僵硬,后观察到肝门部斑块继而明确诊断BA。
BA患儿除了TC征和胆囊异常以外,肝动脉增宽也是其特征。Kim WS等[9]报道BA患儿肝动脉增宽,并以在门静脉右支前、后支分叉处测量的肝右动脉内径>1.5 mm为阈值诊断BA的敏感度、特异度和准确性分别为92%、87%和89%。本组16例测量肝动脉内径均增宽,频谱测量显示为高速、高阻。肝门部纤维块、胆囊宽径和肝动脉内径是彩色多普勒超声鉴别囊性胆道闭锁和胆总管囊肿的有效指标,可用于指导术前鉴别诊断[10]。肝门部纤维块和胆囊形态异常被认为是超声检查识别胆道闭锁的客观标志,其诊断胆道闭锁的特异性 96%~100%[11]。肝动脉扩张诊断胆道闭锁的敏感性和特异性分别为92% 和87%[12]。
高频彩色多普勒超声对BA的诊断有很高的敏感性、特异性,较MRI和CT检查具有优势,并具有可短期重复检查等便利条件,对肝脏回声的观察提示肝脏损害程度,对手术预后有一定提示作用。综合以上四项特征,并参考患儿总胆红素及直接胆红素指标,可协助临床早期诊断BA。
1 李智涵,王斌.Ⅲ型胆道闭锁手术治疗研究进展[J].临床小儿外科杂志,2016,15(01):11—13.DOI:10.3969/j.issn.1671—6353.2016.01.004.Li ZH,Wang B.III the operative treatment of biliary atresia is reviewed[J].J Clin Ped Sur,2016,15(01):11—13.DOI:10.3969/j.issn.1671—6353.2016.01.004.
2 詹江华,冯杰雄.开展胆道闭锁多中心研究的价值[J].临床小儿外科杂志,2015,14(01):1—3.DOI:10.3969/j.issn.1671—6353.2015.01.001.Zhang JH,Feng JX.The value of biliary atresia multicenter study[J].J Clin Ped Sur,2015,14(01):1—3.DOI:10.3969/j.issn.1671—6353.2015.01.001.
3 Choi SO,Park WH,Lee HJ,et al.“Triangular cord”:a sonographic finding applicable in the diagnosisof biliary atresia[J].J Pediatr Surg,1996,31(3):363—366.DOI:10.1016/S0022—3468(96)90739—3.
4 ParkWH,Choi SO,Lee HJ.The ultrasonographic“triangular cord”coupled with gallbladder images in thediagnostic prediction of biliary atresia from infantileintrahepatic cholestasis[J].J Pediatr Surg,1999,34(11):1706—1710.DOI:10.1016/S0022—3468(99)90650—4.
5 Park Wh,Choi So,Lee HJ,et al.A new diagnosticapproach to biliary atresia with emphasis on theultrasonographic triangular cord sign:comparison ofUltrasonography,hepatobiliary scintigraphy and liverneedle biopsy in the evaluation of infantile cholestasis[J].J Pediatr Surg,1997,32(11): 1555—1559.DOI:10.1016/S0022—3468(97)90451—6.
6 Lee HJ,Lee SM,Park WH,et al.Objective criteria oftriangular cord sign in biliary atresia on US scans[J].Radiology,2003,229(2):395—〗400.DOI:10.1148/radiol.292020472.
7 Tan Kendrick AP,Phua KB,Ooi BC,et al.Biliaryatresia: making the diagnosis by the gallbladder ghosttriad[J].Pediatr Radiol,2003,33(5):311—315.DOI:10.1007/ s00247—003—0867—z.
8 王晓曼,贾立群.胆道闭锁的超声诊断[J].放射学实践,2010,26(2):220—222.DOI:10.3969/j.issn.1000—0313.2011.02.027.Wang XM,Jia LQ.Ultrasound diagnosis of biliary atresia[J].Raduik Practice,010,26(2):220—222.DOI:10.3969/j.issn.1000—0313.2011.02.027.
9 Kim WS,Cheon JE,Youn BJ,et al.Hepatic arterial diameter measured with US:adjunct for US diagnosis of biliary atresia[J].Radiology,2007,245(2):549—555.
10 陕泉源,蔡秀英,蒋宏,等.彩色多普勒超声检查在鉴别婴幼儿囊性胆道闭锁与胆总管囊肿中的价值[J].中华肝脏外科手术学电子杂志,2015,4(2):105—108.DOI:10.3877/cma.j.issn.2095—3232.2015.02.011.Shan QY,Cai XY,Jiang H,et al.Value of color Doppler ultrasonography in the differential diagnosis of cystic biliary atresia and choledochal cyst in infants[J],Chin J Hepat Surg(Electronic Edition),2015,4(2):105—108.DOI: 10.3877/cma.j.issn.2095—3232.2015.02.011.
11 Lee JH,Kim SH,Kim HY,et al.Early experience of laparoscopiccholedochal cyst excision in children[J].J Korean Surg Soc,2013,85(5):225—229.DOI:10.4174/jkss.2013.85.5.225.
12 Mandrekar JN.Measures of interrater agreement[J].J Thorac Oncol,2011,6(1):6—7.DOI:10.1097/JTO.0b013e318200f983.
Application of high frequency color Doppler ultrasound in the diagnosis of biliary atresia in children.
Du Yanyan,Fu Liujiang,Zhang Xiangxiang,Wang Hongying.
Department of Ultrasonography,Guangzhou women and children’s medical center,Guangzhou 510623,China.Corresponding author:duyanyan,E-mail: duyan962@163.com
ObjectiveTo analyze the ultrasound imaging characteristics of infantile biliary atresia,and to discusses high frequency colour ultrasound imaging in the early diagnosis of biliary atresia.Methods46 cases confirmed by surgery and pathology were retrospectively analyzed biliary atresia with preoperative ultrasound image data,combinedwith intraoperative and pathological findings,Comprehensive analysis of ultrasound in liver size and inner conditions of the echo,the detection rate of gallbladder and gallbladder size and shape,liver mun structure,hepatic artery diameter and blood flow spectrum features,and evaluate the early diagnostic value.ResultsPreoperative ultrasound showed increase liver morphology,24 cases(52%)of the echo change in the liver.There are 2 cases ofGallbladder is notdisplayed,6 cases of gallbladder show less clear (with crack sample gallbladder),20 cases of gallbladder length to diameter<15 mm with,and 18 cases of gallbladder length to diameter>15 mm children.Ultrasonic indicated that liver fiber piece of 42 cases of portal vein,2 cases MRI suggested biliary atresia,2 cases of ultrasonic hint antrum of hepatic portal vein capsule.Hepatic artery diameter 2.2~2.8 mm,the average of 2.4 mm.Hepatic arterial spectrum for high-speed,high resistance of blood flow,PSV:77~123 cm/s,RI:0.89 to 0.96.ConclusionsGallbladder morphology and hepatic portal vein fiber is one of the important signs of ultrasonic diagnosis of biliary atresia,integrated application of the liver and hepatic artery diameter and spectrum characteristics has certain value for early diagnosis of infantile biliary atresia.
The high frequency exceeds;Biliary atresia;The gallbladder;Hepatic portal vein fiber; The liver form;The hepatic artery
2016—08—22)
(本文编辑:仇 君 王爱莲)
杜妍妍,符柳江,张向向,等.高频彩色多普勒超声在诊断小儿胆道闭锁中的应用[J].临床小儿外科杂志,2017,16(1):89-91.
10.3969/j.issn.1671—6353.2017.01.021.
Cite this article as:Du YY,Fu LJ,Zhang XX,et al.Application of high frequency color Doppler ultrasound in the diagnosis of biliary atresia in children[J].J Clin Ped Sur,2017,16(1):89-91.DOI:10.3969/j.issn.1671—6353.2017.01.021.
10.3969/j.issn.1671—6353.2017.01.021
广东省卫生厅A2013519 超声斑点追踪技术评价妊娠糖尿病胎儿心室局部收缩功能
广州市妇女儿童医疗中心超声科(广东省广州市,510623),通信作者:杜妍妍,E-mail:duyan962@163.com