New bone fixation plate for the repair of avulsion fracture of the tibial attachment of the posterior cruciate ligament: study protocol for a prospective, open-label, self-controlled, clinical trial
Guang-dong Chen*, Tong-jun Cao
Cangzhou Central Hospital, Cangzhou, Hebei Province, China
Introduction
History and current related studies
The posterior cruciate ligament is an important knee structure that maintains knee stability and prevents backward displacement of the tibia. Trauma that causes the tibia to move backward can cause posterior cruciate ligament rupture (Lai et al., 2016; Onishi et al., 2016; Xu et al., 2016;Zhang et al., 2016). Avulsion fracture of the tibial attachment of the posterior cruciate ligament creates unstable posterior movement and rotation of the knee and accelerates degeneration in the knee. Therefore, maintaining tension in the posterior cruciate ligament and restoring anatomical stability of the knee affect early rehabilitation and surgical treatment, and are the most dif ficult and key points of sports medicine related to this injury (Jia et al., 2013; Chen et al.,2015; Muhm and Winkler, 2015).
When avulsion fracture of the tibial attachment of the posterior cruciate ligament is treated with open reduction and rivet fixation, hollow screw fixation, or arthroscopic reconstruction of the posterior cruciate ligament, plaster fixation is often required for postoperative flexion and extension exercises. However, the importance of early tension reconstruction of the posterior cruciate ligament is often ignored (Nicandri et al., 2008; Wang et al., 2008; Frosch et al., 2010; Chen et al., 2012). Controversy persists regarding how to select the best fixation method for avulsion fracture of the tibial attachment of the posterior cruciate ligament and how to restore anatomical stability of the knee joint(Valis et al., 2008; Yoo et al., 2008). Recent developments in surgical techniques and instrumentation, and popularization of the concept of precision surgical treatment demand new fracture fixation methods.
Main objective
We will construct a self-designed plate fixation device for posterior cruciate ligament reconstruction aiming to verify its advantages regarding anatomical knee stability to achieve fracture healing and maintain tension after posterior cruciate ligament reconstruction.
Methods/Design
Study design
This will be a prospective, single-center, open-label, selfcontrolled, clinical trial.
Study setting
Cangzhou Central Hospital, Cangzhou, Hebei Province,China.
Study procedures
We will recruit 20 patients with avulsion fracture of the tibial attachment of the posterior cruciate ligament from Cangzhou Central Hospital of China. Tibial avulsion fracture will be repaired through a posterior approach using a new plate fixation device and posterior cruciate ligament reconstruction. The Hospital for Special Surgery knee score and Lysholm Knee Scoring Scale score will be measured preoperatively and postoperatively at 3 and 12 months(Figure 1).
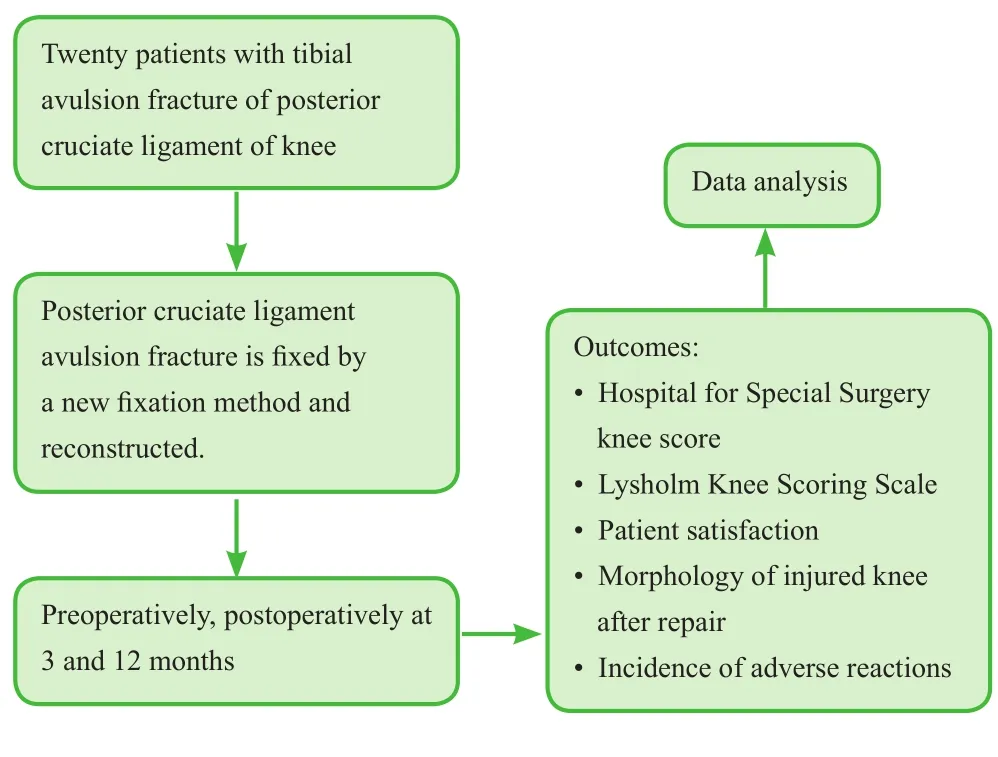
Figure 1: Flow chart of the clinical trial.
This trial is designed to verify that this new fixation device is solid, safe and reliable, can effectively reconstruct the posterior cruciate ligament, maintain good tension, and restore knee function so that patients can undergo rehabilitation exercise as soon as possible after surgery.
Participants were recruited from August 2013 to November 2015. Postoperative follow-up and data collection were completed from November 2015 to November 2016.
Inclusion criteria
Patients who satisfy all of the following criteria will be considered for study inclusion:
· Avulsion fracture of the tibial attachment of the posterior cruciate ligament
· Limited flexion and extension of the knee, posterior drawer test (+)
· History of knee trauma
· Age range: 35-58 years
· Either gender
· Signed informed consent
Exclusion criteria
Patients with one or more of the following conditions will be excluded from this study:
· Pathological fracture
· Fracture accompanied by nerve injury
· Knee osteoarthritis
· Other chronic knee disease
Baseline analysis
Patients’ demographic information and general medical history are shown in Table 1.
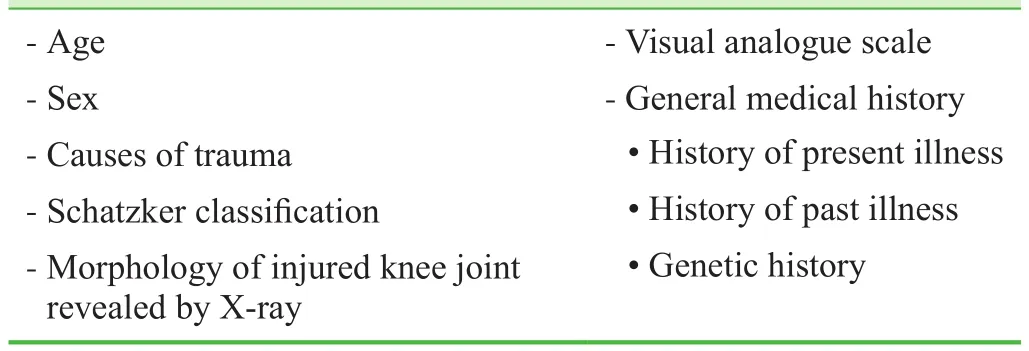
Table 1: Patients’ baseline data
Sample size
Based on previous experience, we hypothesize that Hospital for Special Surgery will increase 50 points 12 months’postoperatively compared with preoperative scores (35-45 points). The standard deviation of the Hospital for Special Surgery score will be set at 10 points. Withβ= 0.1 and power = 90% and with a signi ficance level ofα= 0.05,we calculated a final effective sample size ofn= 13 using PASS 11.0 software (NCSS, Kaysville, UT, USA). If we assume a patient loss rate of 20%, we will require 16 patients.Therefore, we aim to include 20 patients in accordance with the inclusion and exclusion criteria.
Recruitment
Recruitment information will be posted on the Cangzhou Central Hospital bulletin boards. Notice information will clarify the content of the study and indicate that patients participating in the trial will have access to postoperative nutrition-related drugs free of charge. Patients will be able to contact the project leader by telephone. After providing informed consent, potential participants meeting the inclusion and exclusion criteria will be enrolled.
Randomization and blinding
This is a single-sample, open-label, self-controlled clinical trial without randomization. Patients, physicians, and assessors will not be blinded to group information or the therapeutic regimen.
Interventions
Fixation methods: Following induction of anesthesia,patients will be placed in the prone position. Skin will be sterilized three times with povidone iodine, and following draping with sterile towels, an inverted “L”-type incision will be made posterior to the knee. Incision direction follows the medial midline skin posterior to the knee in the transverse direction along the upper medial margin of the gastrocnemius arc, cut interoinferiorly. Deep fascia will be longitudinally incised. The loose tissue between the semitendinosus and medial head of the gastrocnemius will be separated to expose the posterior articular capsule. The posterior articular capsule will then be incised to enter the knee joint cavity. Tension sutures will be placed in patients with severe avulsion fracture of the posterior cruciate ligament. Under proper tension to maintain tension in the ligament, the tibial fracture fragments will be easily reset. An anatomical locking plate will be placed on the tibial plateau followed by cancellous bone screw to fix the middle upper fracture site. The screw will not exceed the tibial plateau. Braided suture will then be secured to a special internal fixation device (different types of fixture devices have received national utility model patent approval; patent No. ZL201620025670.3). Tension in the posterior cruciate ligament, and flexion, extension and stability of the knee will then be evaluated, and the incision will be closed.
Postoperative management: Toe plantar flexion and dorsiflexion will be performed on the affected side after patients regain consciousness on the day of surgery. After removal of the drainage system, patients will perform non-weightbearing walking with crutches on day 2 after surgery for functional exercise of the quadriceps femoris. Passive knee flexion exercises will be initiated 2 weeks later. Active knee exercises will be performed with guidance at 3-4 weeks.At 6 weeks, X-rays will be performed to con firm fracture healing and satisfactory fixation position. Patients will then perform weight-bearing exercises.
Follow-up: After discharge following surgery, patients will be followed-up once per month for 6 months, then every 2 months for 6-12 months. Follow-up evaluations of the study parameters will be performed postoperatively at 3 and 12 months.
Knee function evaluation
(1) Hospital for Special Surgery (Kladny et al., 2002): The total score is 100 points, which comprises 30 points for pain, 22 points for function, 18 points for range of motion, 10 points for muscle strength, 10 points for flexion deformity, and 10 points for joint stability. Deduction items are walker use, varus and valgus deformity, and incomplete extension. Excellent: greater than 85 points;good: 70-84 points; average: 60-69 points; poor: less than 59 points.
(2) Lysholm Knee Scoring Scale (Bengtsson et al., 1996):Eight items score 0-100 points in total. Excellent: greater than 95 points; good: 94-85 points; average: 84-65 points;poor: less than 65 points.
Outcome measures
Primary outcome measure
Hospital for Special Surgery preoperatively and postoperatively at 3 and 12 months: The higher the score, the better the recovery of knee function.
Secondary outcome measures
· Lysholm Knee Scoring Scale preoperatively and postoperatively at 3 and 12 months.
· Patient satisfaction postoperatively at 3 and 12 months:The percentage of the number of patients with satisfactory knee function compared with the total number of cases. The higher the value, the more satis fied the patient is with the treatment plan.
· Morphology of the injured knee 3 and 12 months after repair: X-ray, computed tomography, and magnetic resonance imaging will be used to evaluate the repair of the injury site, whether the fixator is stable, and whether the fracture line is healed.
Other outcome measure
Incidence of adverse events 3 and 12 months postoperatively: The percentage of the number of cases with adverse events compared with the total number of cases to determine the incidence of complications.
The schedule of outcome-measurement assessments is shown in Table 2.
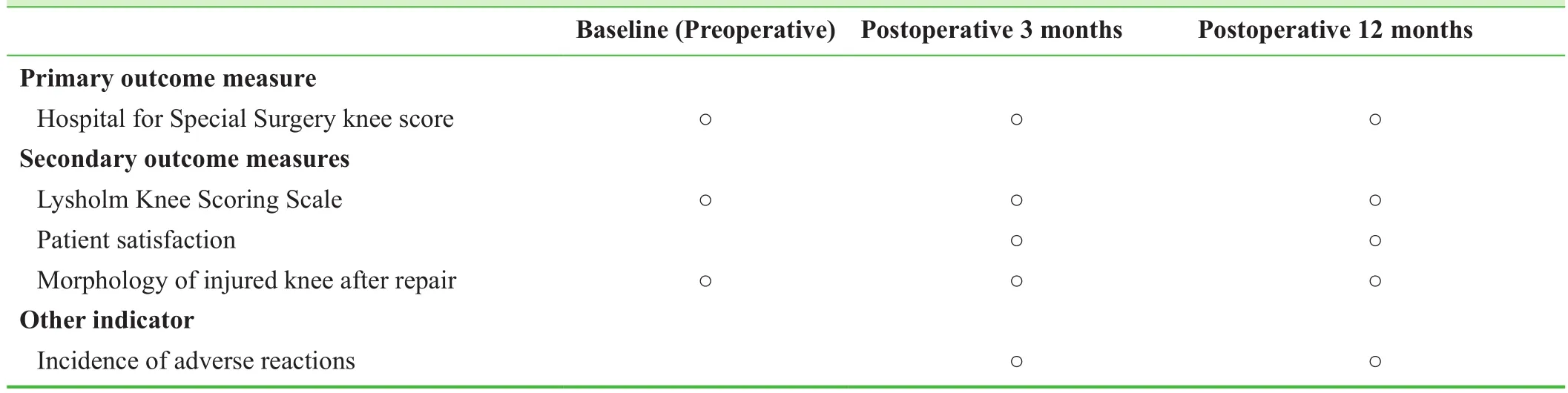
Table 2: Timing of outcome assessments
Adverse events
We will record adverse events, including incision pain,infection, knee pain, peripheral nerve injury, fixation loss,and loosening. During follow-up, if severe adverse events occur, investigators will report the details, including the date of occurrence, type, and measures taken to treat the adverse event, to the principle investigator and the institutional review board within 24 hours.
Data collection, management, analysis, open access
Data collection: Case report forms will be collected and then processed using Epidata software (Epidata Association, Odense, Denmark), collated, and then recorded electronically by data managers using a double-data entry strategy.
Data management: The locked electronic database will be accessible and locked only by the project manager.This arrangement will not be altered. Cangzhou Central Hospital, China will preserve all of the data regarding this trial.
Data analysis: A professional statistician will statistically analyze the electronic database and will create an outcome analysis report that will be submitted to the lead researchers.An independent data monitoring committee will supervise and manage the trial data, ensuring a scienti fic and stringent trial that yields accurate and complete data.
Data open access: Anonymized trial data will be published at www. figshare.com.
Statistical analysis
Statistical analysis will be performed using SPSS 13.0 software (SPSS, Chicago, IL, USA) and will follow the intention-to-treat principle. Normally-distributed measurement data will be expressed as means ± standard deviation and minimums and maximums. Non-normally-distributed measurement data will be expressed as the lower quartile and median and upper quartiles. The count data will be expressed as a percentage.
Normally-distributed data from the Hospital for Special Surgery and Lysholm Knee Scoring Scale scores preoperatively and 3 and 12 months postoperatively will be analyzed with one-way analysis of variance and least signi ficant difference. Non-normally-distributed data will be analyzed using Kruskal-WallisH-test and Cohen’s dtest. Patient satisfaction and incidence of adverse events 3 and 12 months postoperatively will be compared using McNemar’sχ2test. The signi ficance level will be set atα= 0.05.
Trial Status
This trial was completed at the time of submission. Partial results are as follows:
Twenty patients were followed for 12 months. No serious complications occurred, such as incision infection or vascular and nerve injury. All fractures healed satisfactorily,and no fixation loss or failure occurred. Two patients experienced slight soreness at the posterior knee when performing flexion and extension exercises during the final follow-up,but the soreness did not impact normal life.
Hospital for Special Surgery results were excellent in 15 cases, good in 4 cases, and average in 1 case, with an excellent and good rate of 95%. The mean knee flexion and extension angle was 110°-135°. Patient satisfaction evaluation revealed that 19 patients were “very satis fied or satis fied”, and 1 patient selected “general”, with a total satisfaction rate of 90%. Hospital for Special Surgery and Lysholm Knee Scoring Scale scores were not signi ficantly different comparing 3- and 12- month postoperative scores (P> 0.05; Tables 3, 4). Typical cases are displayed in Figure 2.
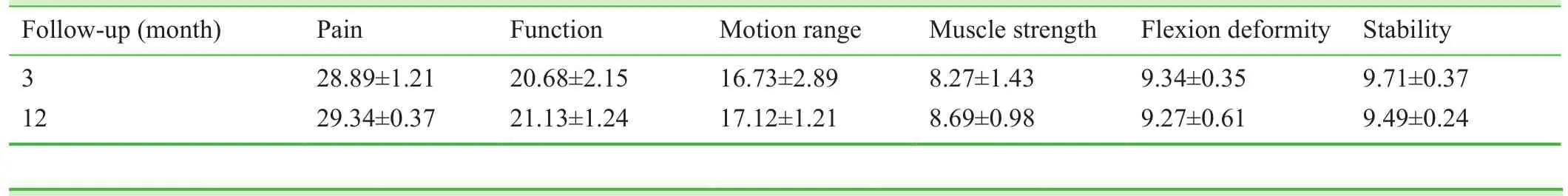
Table 3: Items in the Hospital for Special Surgery knee score
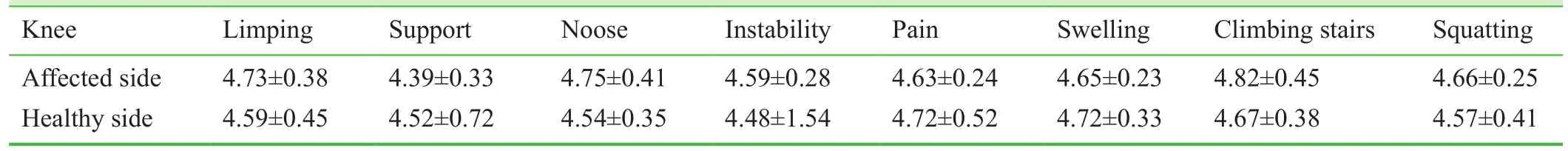
Table 4: Lysholm Knee Scoring Scale in bilateral knees

Figure 2: lmages of a 58-year-old male patient with avulsion fracture of the tibial attachment of the posterior cruciate ligament in the right knee before and after surgery.
Discussion
Significance of this study
Many scholars recommend the use of open reduction and internal fixation to treat avulsion fractures of the posterior cruciate ligament attachment on the tibial plateau. However,previous studies used primarily steel wire, high-strength sutures, hollow screws, absorbable screws, and single anchors for repair. Because fracture fragments were small in this injury, crushed bone could not be fixed firmly, and longterm postoperative external fixation was necessary to delay knee function training time. Therefore, we designed a new fixation device, and aimed to evaluate whether this fixation device was stable and reliable, and whether the technique allowed reconstruction of the posterior cruciate ligament and maintained good ligament tension and knee stability to permit early functional exercises, postoperatively. Long-term follow-up demonstrated that knee function was excellent and good in the majority of patients. This fixation device is designed based on anatomy, is light-weight, avoids friction between the device and the posterior articular capsule, and avoids related complications.
Limitations of this study
The limitations of this study are as follows: We did not include a control group in the study design. Outcomes re flect a single institution, and may not be transferrable to other areas. We cannot effectively verify the ef ficacy and safety, which must be con firmed in further randomized controlled clinical trials(Li et al., 2016; Wu and Zhang, 2016; Yin et al., 2016).
Evidence for contribution to future studies
We hope to maximize the restoration of knee stability and to promote postoperative knee function recovery using internal fixation with a new fixation device through a posterior approach and reconstruction of the posterior cruciate ligament.
Declaration of patient consent
The authors certify that they will obtain all appropriate patient consent forms. In the form the patients will give their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
Trial concept and design, manuscript writing, critical revision,supervision: GDC. Assistance: TJC. Final approval of publication:GDC and TJC.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
Bengtsson J, Möllborg J, Werner S (1996) A study for testing the sensitivity and reliability of the Lysholm knee scoring scale. Knee Surg Sports Traumatol Arthrosc 4:27-31.
Chen LB, Wang H, Tie K, Mohammed A, Qi YJ (2015) Arthroscopic fixation of an avulsion fracture of the tibia involving the posterior cruciate ligament: a modi fied technique in a series of 22 cases.Bone Joint J 97-B:1220-1225.
Chen SY, Cheng CY, Chang SS, Tsai MC, Chiu CH, Chen AC, Chan YS (2012) Arthroscopic suture fixation for avulsion fractures in the tibial attachment of the posterior cruciate ligament. Arthroscopy 28:1454-1463.
Frosch KH, Balcarek P, Walde T, Stürmer KM (2010) A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures. J Orthop Trauma 24:515-520.
Jia KJ, Guan JJ, Yang CL, Liu DH, Jiang HZ, Ma GT (2013) Cannulated screw fixation through posteromedial approach screw for the treatment of tibial avulsion fracture of the tibial attachment of the posterior cruciate ligament. Zhongguo Gu Shang 26:727-729.
Kladny B, Albrecht C, Haase I, Swoboda B (2002) Outcome of inpatient rehabilitation following total knee replacement using the HSS-Score. Z Orthop Ihre Grenzgeb 140:37-41.
Lai Z, Liu ZX, Yang JL, Zhang ZF, Chang YL (2016) Clinical effect of staged repair and reconstruction of multiple ligament injuries in knee joints. Zhongguo Gu Shang 29:404-407.
Li Z (2016) Minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws for repair of distal radius fracture: study protocol for a randomized controlled trial. Clin Transl Orthop 1:58-63.
Muhm M, Winkler H (2015) The posterocentral approach to the posterior tibial plateau. Oper Orthop Traumatol 27:80-93.
Nicandri GT, Klineberg EO, Wahl CJ, Mills WJ (2008) Treatment of posterior cruciate ligament tibial avulsion fractures through a modi fied open posterior approach: operative technique and 12- to 48-month outcomes. J Orthop Trauma 22:317-324.
Onishi Y, Hino K, Watanabe S, Watamori K, Kutsuna T, Miura H(2016) The in fluence of tibial resection on the PCL in PCL-retaining total knee arthroplasty: a clinical and cadaveric study. J Orthop Sci 21:798-803.
Valis P, Repko M, Krbec M, Nýdrle M, Chaloupka R (2008) Surgical management of posterior cruciate ligament avulsion fracture.Acta Chir Orthop Traumatol Cech 75:34-39.
Wang JQ, Ao YF, Yu CL, Cui GQ, Yu JK (2008) Arthroscopic suture fixation of tibial avulsion fracture of posterior cruciate ligament 43:369-372.
Wu T, Zhang GQ (2016) Minimally invasive treatment of proximal humerus fractures with locking compression plate improves shoulder function in older patients: study protocol for a prospective randomized controlled trial. Clin Transl Orthop 1:51-57.
Xu H, Chen YM, Zhai LF, Bi DW (2016) Surgical treatment of multiple ligament injuries of knee joints. Zhongguo Gu Shang 29:456-459.
Yin PB, Long AH, Shen J, Tang PF (2016) Treatment of intertrochanteric femoral fracture with proximal femoral medial sustainable intramedullary nails: study protocol for a randomized controlled trial. Clin Transl Orthop 1:44-50.
Yoo JH, Yang BK, Ryu HK (2008) Lateral epicondylar femoral avulsion fracture combined with tibial fracture: a counterpart to the arcuate sign. Knee 15:71-74.
Zhang B, Cheng CK, Qu TB, Hai Y, Lin Y, Pan J, Wang ZW, Wen L(2016) Partial versus intact posterior cruciate ligament-retaining total knee arthroplasty: a comparative study of early clinical outcomes. Orthop Surg 8:331-337.
 Clinical Trials in Orthopedic Disorder2017年1期
Clinical Trials in Orthopedic Disorder2017年1期
- Clinical Trials in Orthopedic Disorder的其它文章
- Information for Authors -Clinical Trials in Orthopedic Disorders
- Genetic risk factors of degenerative intervertebral disc disease:a case-control study
- MRI appearance of injured ligaments and/or tendons of the ankle in different positions: study protocol for a single-center,diagnostic clinical trial
- Effect of periprosthetic fracture on hip function after femoral neck-preserving total hip arthroplasty: study protocol for a prospective, single-center, self-controlled trial with 2-year follow-up
- Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study
- Effect of tourniquet use during total knee arthroplasty on global inflammatory cytokine changes associated with ischemiareperfusion injury
