Risk factors for ligamentum flavum hypertrophy in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region, China: protocol for a retrospective, single-center study
Gang Zhou, Yu-kun Zhang, Wei-min Huang*
Second Department of Spine Surgery, Sixth Affiliated Hospital, Xinjiang Medical University, Urumqi, Xinjiang Uygur Autonomous Region, China
Introduction
History and current related studies
The increase in human social activities has resulted in an increase in spinal degenerative disease (Chotai et al.,2016; Boissière et al., 2017). Lumbar vertebrae have special anatomical structures and biomechanical characteristics that can easily lead to lumbar spinal stenosis (Kreiner et al., 2014). Lumbar spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebrae(Appendix 1; Schüppel and Weber, 2017; Ulrich et al.,2017). Common causes of degenerative lumbar spinal stenosis include vertebral spondylolisthesis, facet joint hyperplasia, bony spur posterior extension, intervertebral disc prolapse/protrusion, and ligamentum flavum hypertrophy.
Ligamentum flavum hypertrophy is an important cause of spinal stenosis (Gil-Salú et al., 2002; Thomé et al., 2008).When conservative treatment is ineffective, nerve compression (such as single nerve palsy or cauda equina palsy)can cause muscle paralysis or bladder symptoms, which requires surgical treatment (Shen et al., 2014; Spadaro et al., 2014). Common surgical techniques include pedicle screw fixation, flavectomy, laminectomy and facetectomy(Losiniecki et al., 2013; Seki et al., 2013; Amirouche et al.,2016; Baldawa et al., 2016; Burke et al., 2016; Ha et al.,2016). These types of surgery involve important anatomical structures, such as pedicles, ligamentum flavum, laminae,and articular processes.
Many previous studies have investigated pedicle morphology, lumbar ligamentum flavum, laminae and articular processes; important reference data are listed in Table 1.Safak et al. (2010) reported that ligamentum flavum thickness was not associated with sex, ligamentum flavum was markedly thicker on the left side of segments L4/5and L5/S1than on the right side, and ligamentum flavum thickness was not positively correlated with age. Few studies have addressed whether ligamentum flavum thickness is associated with nationality, sex and obesity.
Main objective
The aim of this retrospective study is to measure the ligamentum flavum thickness on CT scans of patients of different nationalities, sexes, heights, ages, and weights from the Xinjiang Uygur Autonomous Region of China, explore the correlation between various factors and ligamentum flavum thickness, provide a reference for pedicle screw placement and lumbar decompression surgery, develop individualized surgical programs, and effectively reduce the incidence of unnecessary postoperative complications induced by misplacement.
Methods/Design
Study design
A retrospective, single-center, case analysis.
Study setting
Sixth Af filiated Hospital, Xinjiang Medical University,Urumqi, Xinjiang Uygur Autonomous Region, China.
Study procedures
We collected lumbar CT imaging data of 104 patients with lumbar spinal stenosis who were evaluated in the Sixth Affiliated Hospital, Xinjiang Medical University from May 2012 to May 2016. We observed the incidence of ligamentum flavum hypertrophy inpatients of different nationalities,sexes, heights, ages, and weights, and explored risk factors affecting ligamentum flavum hypertrophy (Figure 1). Data collection began in May 2012, and data analysis is expected to be completed in May 2017.
Patients who met the inclusion criteria of this study were recruited by telephone. All patients agreed to the experiment and signed informed consent.
Inclusion criteria
Patients meeting all of the following criteria were considered for admission to the trial:
· Lumbar spinal stenosis revealed by lumbar CT images· Low back pain
· Aged 45-80 years
· Either sex
· Provided written, informed consent
Exclusion criteria
Patients presenting with any of the following were excluded from the trial:
· Spinal injury
· Spinal tumor
· Spinal infection
· Congenital or acquired spine deformity
· Pulmonary tuberculosis
· Severe systemic diseases such as malignant tumor
· Inability to cooperate due to mental illness or other causes
Sample size
Ligamentum flavum thickness greater than 4 mm on CT imagery is de fined as ligamentum flavum hypertrophy.We hypothesized that the ligamentum flavum thickness would be increased by 1.4 mm in Hazakh patients and by 0.7 mm in Han patients. The standard deviation of ligamentum flavum thickness was predicted to be 0.9. Takingβ= 0.1 and power = 90% with a signi ficance level ofα= 0.05, the final effective sample size ofn= 36 Kazakh patients was calculated using PASS 11.0 software (NSCC,Kaysville, UT, USA). Assuming a patient loss rate of 20%,we required 44 patients per group, giving a total of 132 patients of three nationalities. After screening according to the inclusion and exclusion criteria, 104 patients were included in the trial.

Table 1: Research progress regarding lumbar spinal canal anatomy
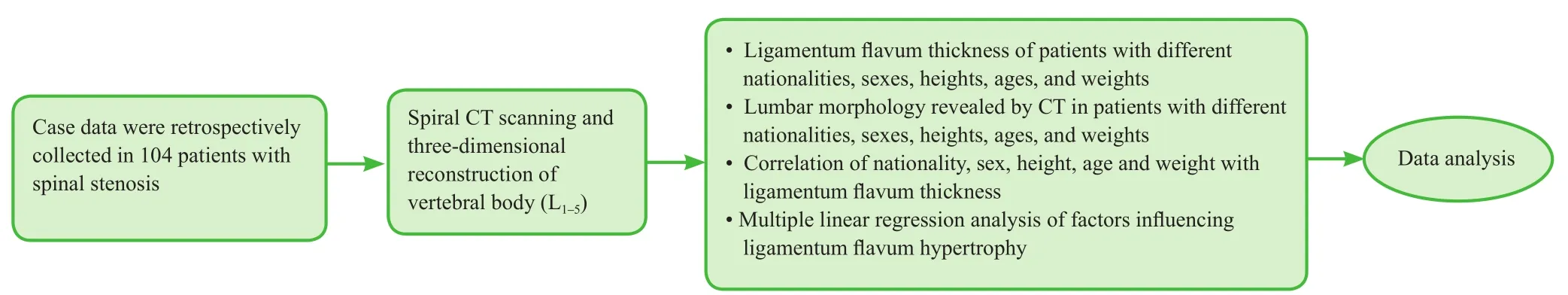
Figure 1: Flow chart of the study protocol.
Baseline analysis
Baseline data of 104 patients were evaluated after informed consent was obtained, including sex, age, height, nationality, weight, history of present illness, past history, family history, personal history, marital history, laboratory exami-nation, and CT examination (Table 2).
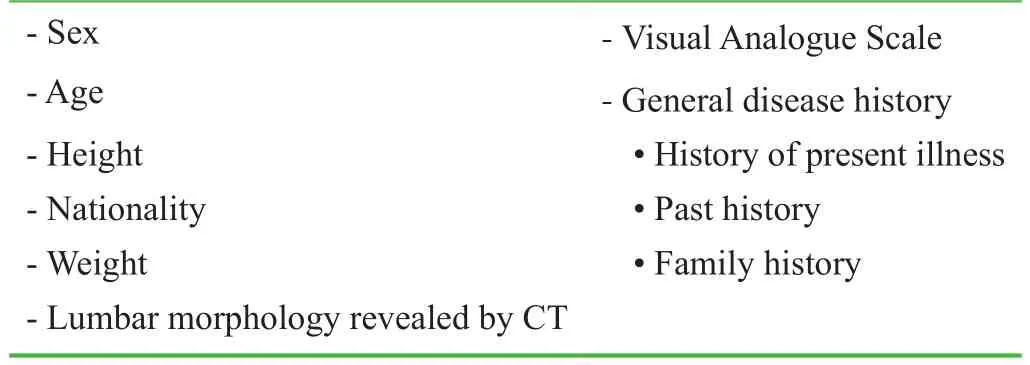
Table 2: Baseline data and general medical history of included patients
Patients’ medical records
All data were collected from medical records. Patients were asked to fill in a questionnaire, including general information (name, sex, nationality and occupation), history of present illness (causes, accompanying symptoms, severity and treatment), past history, personal history, family history, and marital history. General physical examination and special examination for lumbar spinal stenosis were conducted.We recorded left lower limb pain, right lower limb pain,both lower limb pain, intermittent claudication (Appendix 2), straight-leg raising test (+), spinous process tenderness,unilateral lower limb radiating pain, lower limb paresthesia,abnormal muscle strength, and abnormal re flexes.
Lumbar spine CT scan
L1-5vertebrae were scanned with a Siemens Emotion 6 CT Scanner (Siemens, Germany), and three-dimensional reconstruction was conducted. Scan parameters were collimator 0.65 mm, layer thickness 3 mm, and reconstruction increment 1.5 mm. The reconstructed image was passed to the browser. CT and three-dimensional reconstructed images were measured with the angle and length measurement tools of the browser by the same physician. Ligamentum flavum thickness (the length of C-E in Figure 2) was measured at the segments L2/3, L3/4, L4/5and L5/S1.
Outcome measures
Primary outcome measure
· Ligamentum flavum thickness of patients of different nationalities, sexes, heights, ages, and weights measured on CT. That is, the changes in ligamentum flavum thickness according to different in fluential factors.
Secondary outcome measures
· Lumbar morphology of patients of different nationalities,sexes, heights, ages, and weights measured on CT. That is, changes in ligamentum flavum morphology.
· Correlation of nationality, sex, height, age and weight with ligamentum flavum thickness.
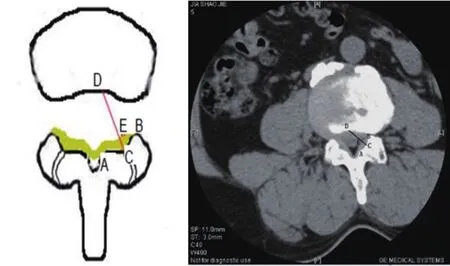
Figure 2: Ligamentum flavum thickness revealed by computed tomography.
· Multiple linear regression analysis results of relevant factors in fluencing ligamentum flavum hypertrophy.Multiple linear regression analysis was performed to verify the correlation of each in fluential factor with ligamentum flavum hypertrophy.
Data collection, management, analysis and open-access
Written and electronic data were collected. The electronic data were stored in a specialized computer, and locked by the data manager. The written data were stored and locked in a reference room that was only accessible by the data manager and laboratory manager.
The locked database was not altered and was preserved along with the original records. The database was analyzed by a professional statistician.
Prior to any analysis of the data, the analysis plan outlined in this section was reviewed, and detailed statistical analysis plans were prepared and approved. All data regarding this trial will be preserved by the Sixth Af filiated Hospital,Xinjiang Medical University, China.
Anonymized trial data were published at www. figshare.com.
Statistical analysis
All data were analyzed using SPSS 21.0 software (IBM,Armonk, NY, USA). All measurement data were normally distributed, and were expressed as the mean ± standard deviation. Ligamentum flavum thickness was compared among groups using the two-samplet-test or one-way analysis of variance. Paired comparison between groups was conducted using the Student-Newman-Keuls test.Correlation of nationality, sex, height, age and weight with ligamentum flavum thickness was analyzed using Pearson’scorrelation coef ficient. Risk factors for ligamentum flavum hypertrophy were analyzed using multiple linear regression analysis. Odds ratios and 95% con fidence intervals were calculated. The signi ficance level wasα= 0.05.
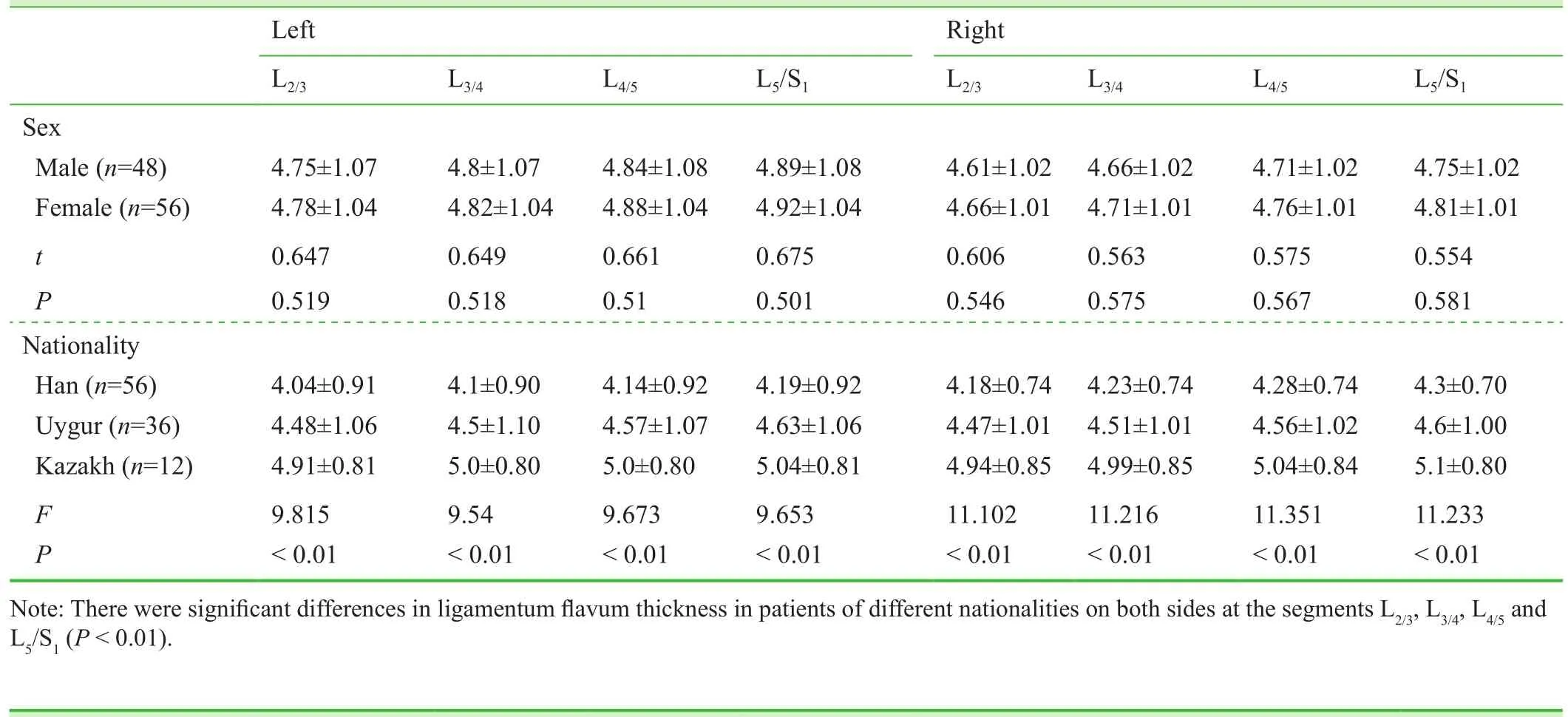
Table 3: Comparison of the difference in ligamentum flavum thickness in patients of different nationalities and sexes
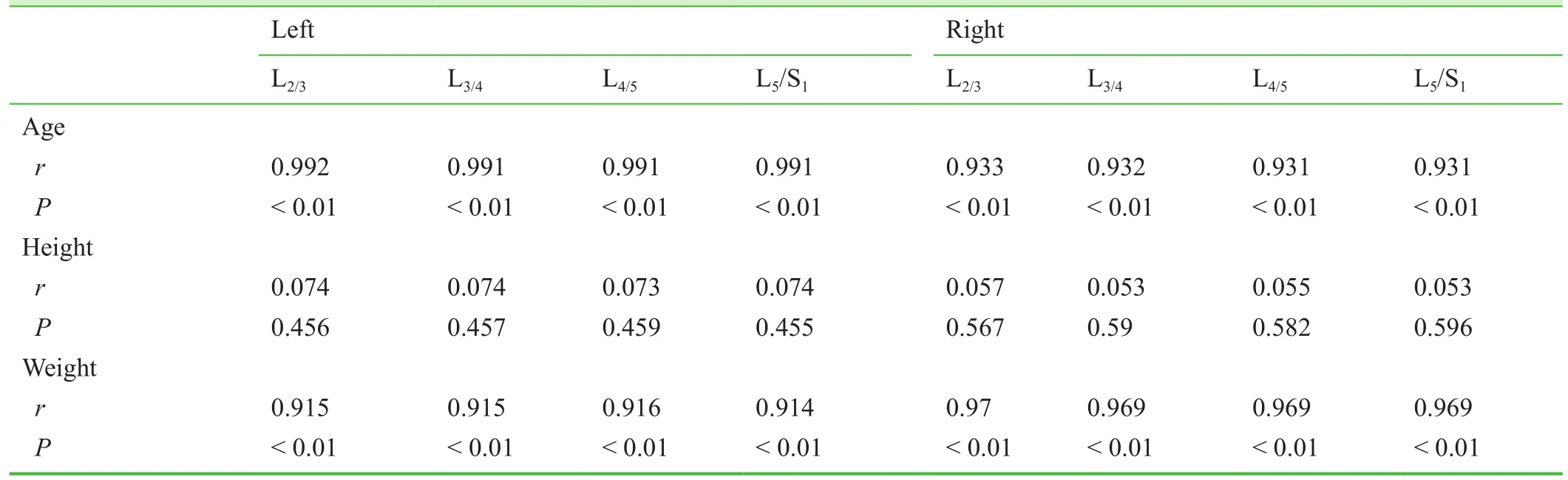
Table 4: Correlation of age, height and weight with ligamentum flavum thickness
Trial Status
Data analysis has been partially completed, and the partial results are as follows:
(1) Baseline data: Among 104 patients, there were 48 males and 56 females, with a mean age of 49.12 ± 11.06 years. There was left lower limb pain in 43 cases, right lower limb pain in 61 cases, both lower limbs pain in 43 cases,intermittent claudication in 19 cases, straight-leg raising test(+) in 34 cases, and spinous process tenderness in 32 cases;moreover, 75 cases experienced unilateral lower limb radiating pain, lower limb paresthesia, abnormal muscle strength and abnormal re flexes.
(2) Difference in ligamentum flavum thickness in patients with different nationalities and sexes: The thickness at segments L2/3, L3/4, L4/5and L5/S1on both sides was normally distributed. There was no signi ficant difference between sexes in ligamentum flavum thickness at the segments L2/3,L3/4, L4/5and L5/S1(P> 0.05). Ligamentum flavum thickness signi ficantly differed at the segments L2/3, L3/4, L4/5and L5/S1according to nationality (P< 0.01; Table 3).
(3) Correlation of age, height and weight with ligamentum flavum thickness: Ligamentum flavum thickness was positively correlated with age and weight (P< 0.05), but was not obviously associated with height (Table 4).
Discussion
Analysis of test results
Degenerative spinal stenosis is the most common cause of spinal stenosis. Ligamentum flavum hypertrophy is one of the most common causes of lumbar spinal stenosis. CT images revealed a strip- or V-shaped soft tissue density shadow at the posterior spinal canal along the laminae. Thickness of more than 4 mm was considered ligamentum flavum hypertrophy. CT can clearly reveal the morphology and boundaries of the ligamentum flavum. The tracer method can be used to measure ligamentum flavum thickness,sagittal diameter of the dural sac, and sagittal diameter of the lateral recess, thereby revealing the location, extent and range of hypertrophic ligamentum flavum. CT can be used to observe the morphology and width of bilateral nerve root canals in the same layer, and is of great value in the diagnosis of lateral ligamentum flavum hypertrophy.
Most previous studies have con firmed that the ligamentum flavum increases with age, mainly because of long-term fiber damage and repair (Yoshiiwa et al., 2016). Our results demonstrated that weight was also a factor affecting ligamentum flavum thickness in lumbar spinal stenosis.The increased weight increased the pressure on the lumbar vertebrae, and long-term activity led to an increased chance of ligamentum flavum injury, thereby resulting in increased ligamentum flavum thickness.
Nationality was another factor that affected the thickness of the ligamentum flavum in lumbar spinal stenosis patients in the Xinjiang Uygur Autonomous Region of China, indicating that there were some differences in ligamentum flavum development between nationalities, possibly because of genetic causes. Another possible reason is that different ethnic dietary habits lead to different probabilities of obesity. Nationalities in Xinjiang Uygur Autonomous Region eat a diet that is mostly meat-based. Long-term excess intake of nutrients leads to increased body mass, resulting in ligamentum flavum hypertrophy. The third possible reason is differences in occupation. Different nationalities may have different working habits and physical composition due to the degree of physical labor undertaken, resulting in different degrees of ligamentum flavum damage.
Limitations of this study
The sample size was small and the study area was singular.We hope to carry out a multicenter, large sample of clinical studies in subsequent trials to reduce bias (Li, 2016; Wu and Zhang, 2016; Yin et al., 2016).
Significance of this study
CT was conducted in lumbar spinal stenosis patients from the Xinjiang Uygur Autonomous Region to measure ligamentum flavum thickness, and evaluate its correlation with sex, age, nationality and weight. The results will promote the prevention and treatment of lumbar spinal stenosis caused by ligamentum flavum hypertrophy in the Xinjiang Uygur Autonomous Region.
Appendix 1 Definition for lumbar spinal stenosis
A medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebrae. Lumbar spinal stenosis is one of the most common causes of lumbar diseases, such as low back pain and leg pain, and mainly occurs in those aged greater than 40 years. No symptoms are seen at rest. Lower limb pain,numbness, and weakness can appear after walking. The above symptoms will be mitigated after squatting down or resting. The exacerbation of symptoms causes patients to walk shorter distances, and require longer rest periods.
Appendix 2 Definition for intermittent claudication
A symptom that describes muscle pain, including ache,cramp, numbness or sense of fatigue, classically in the calf muscle, which occurs during exercise, such as walking, and is relieved by a short period of rest. The severity of intermittent claudication is commonly judged by claudication distance and remission time. Claudication distance refers to walking distance from the beginning of the walk to the onset of pain. Obvious discomfort and pain can appear in severely affected patients after walking 50-100 m. Remission time refers to the time from pain onset to painlessness after resting. The remission time is generally 2-5 minutes.Claudication is one of the main clinical features of lumbar spinal stenosis.
Declaration of patient consent
The authors certify that they will obtain all appropriate patient consent forms. In the form the patients will give their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
None declared.
Author contributions
Trial concept and design, manuscript writing, critical revision,supervision, and final approval of publication: GZ. Assistance:YKZ and WMH.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
Abbas J, Hamoud K, Masharawi YM, May H, Hay O, Medlej B,Peled N, Hershkovitz I (2010) Ligamentum flavum thickness in normal and stenotic lumbar spines. Spine (Phila Pa 1976)35:1225-1230.
Altinkaya N, Yildirim T, Demir S, Alkan O, Sarica FB (2011) Factors associated with the thickness of the ligamentum flavum: is ligamentum flavum thickening due to hypertrophy or buckling?Spine (Phila Pa 1976) 36:E1093-1097.
Amirouche F, Solitro GF, Magnan BP (2016) Stability and spine pedicle screws fixation strength-a comparative study of bone density and insertion angle. Spine Deform 4:261-267.
Amonoo-Kuo fiHS (1995) Age-related variations in the horizontal and vertical diameters of the pedicles of the lumbar spine. J Anat 186:321-328.
Baldawa S, Shivpuje V (2016) Migratory low velocity intradural lumbosacral spinal bullet causing cauda equina syndrome: report of a case and review of literature. Eur Spine J
doi:10.1007/s00586-016-4913-6.
Boissière L, Moal B, Gille O, De-Roquefeuil E, Durieux M, Obeid I, Dousset V, Vital JM, Skalli W (2017) Lumbar spinal muscles and spinal canal study by MRI three-dimensional reconstruction in adult lumbar spinal stenosis. Orthop Traumatol Surg Res
doi:10.1016/j.otsr.2016.10.025.
Burke SM, Hwang SW, Safain MG, Riesenburger RI (2016) Iatrogenic spinal cord injury during removal of the inferior articular process in the presence of ossi fication of the ligamentum flavum.Case Rep Surg
doi:10.1155/2016/2318759.
Chotai S, Parker SL, Sielatycki JA, Sivaganesan A, Kay HL, Wick JB, McGirt MJ, Devin CJ (2016) Impact of old age on patientreport outcomes and cost utility for anterior cervical discectomy and fusion surgery for degenerative spine disease. Eur Spine J
doi:10.1007/s00586-016-4835-3.
Cui XG, Ding ZH, Cai JF (2004) Radiographic anatomy study of the relationship between the root and the pedicle of thoracolumbar spinous process. Zhongguo Jiaoxing Waike Zazhi 1296-1298.
Du LJ, Li JJ (2009) Correlative study on the radius and de flection of pedicle of vertebrae and thoracic vertebrae in Chinese adult men.Zhongguo Jizhu Jisui Zazhi 19:545-549.
Gil-Salú JL, López-Escobar M, Gómez-Cárdenas E, Rodríguez-Peña F, Repeto-López JA, López-López J, García-Vázquez F(2002) Calci fication of the thoracic yellow ligament as a cause of myelopathy. Rev Neurol 34:750-753.
Ha KY, Kim SI, Kim YH, Kim YH, Oh IS (2016) Predictive factors for postoperative follow-up: which patients are prone to loss to follow-up after spinal surgery? Clin Spine Surg
doi:10.1097/BSD.0000000000000465.
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P, Fernand R, Ghiselli G,Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK (2014) An evidencebased clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14:180-191.
Li Z (2016) Minimally invasive closed reduction and internal fixation with fully threaded headless cannulated compression screws for repair of distal radius fracture: study protocol for a randomized controlled trial. Clin Transl Orthop 1:58-63.
Losiniecki AJ, Serrone JC, Keller JT, Bohinski RJ (2013) Lumbar ligamentum flavum: spatial relationships to surrounding anatomical structures and technical description of en bloc resection. J Neurol Surg A Cent Eur Neurosurg 74:388-392.
Safak AA, Is M, Sevinc O, Barut C, Eryoruk N, Erdogmus B, Dosoglu M (2010) The thickness of the ligamentum flavum in relation to age and gender. Clin Anat 23:79-83.
Schüppel J, Weber F (2017) Retrospective matched-pair cohort study on effect of bisegmental fenestration versus hemilaminectomy for bisegmental spinal canal stenosis at L3-L4and L4-L5. J Neurol Surg A Cent Eur Neurosurg
doi:10.1055/s-0036-1597617.
Scoles PV, Linton AE, Latimer B, Levy ME, Digiovanni BF (1988)Vertebral body and posterior element morphology: the normal spine in middle life. Spine (Phila Pa 1976) 13:1082-1086.
Seki S, Kawaguchi Y, Ishihara H, Oya T, Kimura T (2013) Lumbar spinal stenosis due to a large calci fied mass in the ligamentum flavum. Asian Spine J 7:236-241.
Shen L, Fang L, Qiu Y, Xing S, Chen D, He X, Wang J, Lai J, Shi G, Zhang J, Liao T, Tan J (2014) Study on different surgical approaches for acute lumber disk protrusion combined with cauda equina syndrome. Int J Clin Exp Pathol 7:8875-8880.
Shim E, Lee JW, Lee E, Ahn JM, Kang Y, Kang HS (2016) Fluoroscopically guided epidural injections of the cervical and lumbar spine. Radiographics
doi:10.1148/rg.2017160043.
Spadaro A, Ciarrocchi I, Masci C, Cozzolino V, Monaco A (2014)Effects of intervertebral disc disorders of low back on the mandibular kinematic: kinesiographic study. BMC Res Notes 7:569.
Steffee AD, Biscup RS, Sithowski DJ (1986) Segmental spine plates with pedicle screw fixation a new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop 203:45.
Thomé C, Börm W, Meyer F (2008) Degenerative lumbar spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int 105:373-379.
Ulrich NH, Burgstaller JM, Pichierri G, Wertli MM, Farshad M,Porchet F, Steurer J, Held U (2017) Decompression surgery alone versus decompression plus fusion in symptomatic lumbar spinal stenosis: a Swiss prospective multi-center cohort study with 3 years of follow-up. Spine (Phila Pa 1976)
doi:10.1097/BRS.0000000000002068.
Wu T, Zhang GQ (2016) Minimally invasive treatment of proximal humerus fractures with locking com¬pression plate improves shoulder function in older patients: study protocol for a prospective randomized controlled trial. Clin Transl Orthop 1:51-57.
Yin PB, Long AH, Shen J, Tang PF (2016) Treatment of intertrochanteric femoral fracture with proximal femo¬ral medial sustainable intramedullary nails: study protocol for a randomized controlled trial. Clin Transl Orthop 1:44-50.
Yoshiiwa T, Miyazaki M, Notani N, Ishihara T, Kawano M, Tsumura H (2016) Analysis of the relationship between ligamentum flavum thickening and lumbar segmental instability, disc degeneration, and facet joint osteoarthritis in lumbar spinal stenosis.Asian Spine J 10:1132-1140.
Zeng ZY, Jiang CY, Song YX, Zhang JQ, Wang B, Jin CY, Long DY,Wu P, Wang YP (2009) Imaging measurement and clinical signi ficance of lumbar vertebral lamina and articular process. Zhongguo Linchuang Jiepouxue Zazhi 27:420-425.
Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, Thomas JC, Rothman SL, Fields BT (1987) Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 12:160-166.
 Clinical Trials in Orthopedic Disorder2017年1期
Clinical Trials in Orthopedic Disorder2017年1期
- Clinical Trials in Orthopedic Disorder的其它文章
- Information for Authors -Clinical Trials in Orthopedic Disorders
- Genetic risk factors of degenerative intervertebral disc disease:a case-control study
- MRI appearance of injured ligaments and/or tendons of the ankle in different positions: study protocol for a single-center,diagnostic clinical trial
- Effect of periprosthetic fracture on hip function after femoral neck-preserving total hip arthroplasty: study protocol for a prospective, single-center, self-controlled trial with 2-year follow-up
- New bone fixation plate for the repair of avulsion fracture of the tibial attachment of the posterior cruciate ligament: study protocol for a prospective, open-label, self-controlled, clinical trial
- Effect of tourniquet use during total knee arthroplasty on global inflammatory cytokine changes associated with ischemiareperfusion injury
