单侧甲状腺腺叶切除+对侧肿物切除或大部切除术与双侧甲状腺大部切除术治疗双侧结节性甲状腺肿的对比研究
陈 笑 肖 晖 郁正亚
单侧甲状腺腺叶切除+对侧肿物切除或大部切除术与双侧甲状腺大部切除术治疗双侧结节性甲状腺肿的对比研究
陈 笑①*肖 晖①郁正亚①
目的:探讨治疗双侧结节性甲状腺肿的合理术式。方法:回顾性分析328例双侧结节性甲状腺肿患者资料,按照手术方式的不同,将其分为单侧甲状腺腺叶切除+对侧甲状腺肿物切除或大部切除术组(85例)和双侧甲状腺大部切除术组(243例)。比较单侧甲状腺腺叶切除+对侧肿物切除或大部切除术与双侧甲状腺大部切除术后的并发症发生率及复发率;结果:术后随访1~48个月。单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组喉返神经麻痹1例,暂时性甲状旁腺功能减退2例,甲状腺残腔血肿1例。双侧甲状腺大部切除术组喉返神经麻痹2例,皮下血肿2例。单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组复发2例(占2.35%),双侧甲状腺大部切除术组复发17例(占7.00%)。两组均无临床上需要再次手术的病例。结论:单侧甲状腺腺叶切除+对侧肿物切除或大部切除术与双侧甲状腺大部切除术相比术后并发症发生率相似,而复发率低,且具有一侧甲状腺可反复手术而不会导致严重并发症的优势,是一种值得推荐的术式。
结节性甲状腺肿;甲状腺腺叶切除;甲状腺大部切除;复发
[First-author’s address]Department of General Surgery, Capital Medical University Beijing Tongren Hospital, Beijing 100730, China.
结节性甲状腺肿是最常见的内分泌疾病之一。结节性甲状腺肿增大到一定程度会产生压迫症状,压迫气管和食道而引起呼吸困难和吞咽困难,甚至压迫静脉引起头颈部的回流障碍[1]。结节性甲状腺肿产生压迫症状通常需要手术治疗,其他的手术指征还包括肿瘤怀疑为恶性,合并甲状腺机能亢进,胸骨后甲状腺肿和影响美观[2-3]。结节性甲状腺肿最适合的手术方式目前仍存在争议,残留较多甲状腺组织会增大结节性甲状腺肿复发的概率,但扩大手术切除范围会增加术后甲状腺功能减退以及各种手术并发症的发生概率。本研究回顾性分析比较双侧结节性甲状腺肿患者行单侧甲状腺腺叶切除+对侧肿物切除或大部切除术与双侧甲状腺大部切除术术后并发症发生率和复发率的差异,探讨治疗双侧结节性甲状腺肿的合理术式。
1 资料与方法
1.1 一般资料
回顾性分析2012年6月至2016年6月首都医科大学附属北京同仁医院普外科收治的328例双侧结节性甲状腺肿患者资料。其中男性76例,女性252例,男女比例为1∶3.32;年龄19~80岁,平均年龄55.41 岁。按照手术方式的不同,将其分为单侧甲状腺腺叶切除+对侧甲状腺肿物切除或大部切除术组(85例)和双侧甲状腺大部切除术组(243例)。单侧甲状腺腺叶切除+对侧甲状腺肿物切除或大部切除术组中男性23例,女性62例,男女比例为1∶2.26;年龄39~74岁,平均年龄56.73岁。双侧甲状腺大部切除术组中男性53例,女性190例,男女比例为1∶3.49;年龄19~80岁,平均年龄55.41岁。所有患者均经术后病理证实为结节性甲状腺肿。本研究不包括结节性甲状腺肿继发甲状腺机能亢进和病理证实为恶变的病例。
1.2 治疗方法
(1)单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组。行甲状腺腺叶切除术手术中常规显露喉返神经、喉上神经和甲状旁腺,而行甲状腺大部切除术不常规显露以上结构。术后常规放置负压引流。所有手术均由同一手术医师完成。术后患者均常规服用优甲乐2年,控制促甲状腺激素(thyroid stimulating hormone,TSH)0.4~1 uIU/ml(正常值为0.4~6 uIU/ml)。术后第1 d常规捡查甲状旁腺素和钙离子。甲状旁腺素<12 pg/ml(正常值为12~65 pg/ml)即诊断为暂时性甲状旁腺功能减退。血钙离子<2.1 mmol/L(正常值为2.1~2.6 mmol/L)诊断为暂时性低钙血症。声音嘶哑患者行纤维喉镜检查,确定有无声带麻痹。
(2)双侧甲状腺大部切除术手术方法同上。
1.3 观察与评价指标
将结节性甲状腺肿术后复发定义为残余甲状腺腺体需要再手术,新出现结节,或旧结节增大>5 mm。术后2周患者门诊由手术医生复查,此后每3个月门诊复查1次。永久性甲状旁腺功能减退定义为手术后6个月仍需口服钙和维生素D[4]。
1.4 统计学方法
应用SPSS 18.0软件包进行数据处理。计数资料采用x2检验,当1≤理论值≤5且总例数≥40时应用校正公式,当理论值<1或总例数<40时应用Fisher精确概率法。以P<0.05为差异有统计学意义。
2 结果
2.1 两组患者术后复发率比较
单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组患者复发2例,复发率为2.35%;双侧甲状腺大部切除术组复发17例,复发率为7.00%。两组行甲状腺切除术后复发比较差异无统计学意义(Value=1.710,P>0.05)。两组均无临床上需要再次手术的病例。
2.2 两组患者术后并发症发生率比较
术后喉返神经麻痹、暂时性甲状旁腺功能减退、永久性甲状旁腺功能减退、甲状腺残腔血肿、皮下血肿两组比较,差异均无统计学意义,见表1。
3 讨论
治疗结节性甲状腺肿选择何种手术方式目前仍有争论。临床中倾向于将甲状腺大部切除是因术后并发症发生率低,但术后再手术率相对较高。近年来,随着外科技术的提高和临床经验的积累,临床中趋向于行甲状腺全切,因其复发率低[1,5-6]。但是,全甲状腺切除其并发症发生率高,且需要终生甲状腺激素替代治疗。甲状腺单侧腺叶切除,优点是对侧仍有甲状腺组织保留,多数患者无需终生服药或服药量少,易于甲状腺激素调整。由于术后保留了对侧部分腺体,因此通常不会损伤对侧的喉返神经和甲状旁腺。
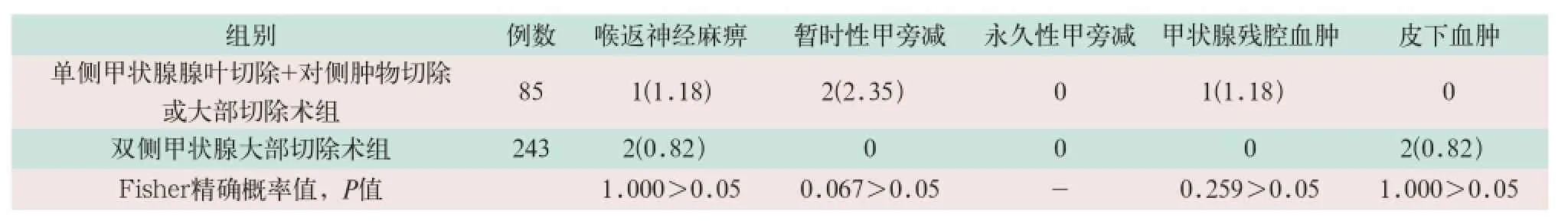
表1 两组患者术后并发症发生率的比较[例(%)]
甲状腺大部切除术的复发率为0%~50%,取决于保留的甲状腺组织的量。而甲状腺全切术的复发率仅为0.3%[7-8]。本研究甲状腺大部切除术组的复发率为7%。Bauer等[9]回顾总结了420例结节性甲状腺肿行单侧腺叶切除+峡部切除的患者,复发率为2%。本研究单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组复发率为2.35%,与文献报道相近。
有文献报道,行单侧甲状腺切除,术后暂时性低钙血症发生率为0%~18%,声音嘶哑发生率为1%~6%,血肿发生率为0%~1%,甲状旁腺功能减退发生率少见[7,10-12]。而行双侧甲状腺腺叶切除,术后暂时性低钙血症发生率为9%~35%,声嘶发生率为1%~10%,血肿发生率为0%~3%,甲状旁腺功能减退发生率为5%~30%[1,7,13-15]。本研究结果与文献报道基本相符。
甲状腺大部切除术多年来一直是结节性甲状腺肿的标准治疗方法,以往通常实施双甲状腺大部切除术治疗双侧结节性甲状腺肿以避免并发症,但会残留较多的甲状腺背侧腺体,导致复发率偏高。近年来,良性甲状腺肿的外科治疗有一种提高根治性的趋势,有外科医生建议甲状腺全切来治疗结节性甲状腺肿[7-8]。但甲状腺全切的术后并发症明显高于其他手术方式。虽然有小部分患者避免了因为复发而需要再次手术的风险,但所有患者均要面对较高的甲状旁腺功能减退或喉返神经麻痹的风险。而且,所有双侧甲状腺腺叶切除的患者术后均需要激素替代治疗来预防甲状腺功能减退。服用甲状腺素需要规律检查和偶尔的药量调整,药物过量会导致不良反应,如房颤、骨质疏松和骨质减少[16]。由于可能对患者的生活质量产生负面影响,而且治疗术后甲状腺功能减退要增加费用,应避免甲状腺激素替代治疗。因此,甲状腺全切术必须在严格评估适应证的情况下方能实施。
甲状腺一叶全切+对侧大部切除,又称为Dunhill术式,是对根治性术式的妥协,残留腺体量为1~4 ml。甲状腺单侧腺叶切除+对侧大部切除术术后并发症发生率基本等同于单侧腺叶切除,并发症较甲状腺全切术明显降低,而且避免了终生激素替代治疗。有研究表明,结节性甲状腺肿行单侧腺叶切除的复发率为1.2%~26%,平均复发时间为10~16年,但并不是所有复发有症状的患者,尤其是老年患者,均需手术治疗,因此再手术率只有0.4%[14,17]。本研究将Dunhill手术略加改良,对于对侧甲状腺肿物不广泛、肿物体积不大的患者,单纯行肿物摘除,以保留尽可能多的甲状腺组织,避免术后服用甲状腺素或减少服药剂量。由于甲状腺再次手术与第一次手术相比具有更高的并发症发生率[18-19]。因此,该术式的另一重要好处是行甲状腺腺叶切除的一侧今后一般不会复发,而另一侧即使复发,可反复手术,即使发生损伤也只可能造成一侧的喉返神经或甲状旁腺损伤,不会产生双侧喉返神经损伤或永久性甲状旁腺功能减退等严重并发症。本研究单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组与双侧甲状腺大部切除术组相比较,术后喉返神经麻痹、甲状旁腺功能减退、血肿等并发症发生率均相近,表明此术式与双侧甲状腺大部切除术一样,是一种较为安全的术式。单侧甲状腺腺叶切除+对侧肿物切除或大部切除术组与双侧甲状腺大部切除术组相比复发率降低,但无统计学差异,考虑可能与随访时间较短有关。
综上所述,双侧结节性甲状腺肿行单侧甲状腺腺叶切除+对侧肿物切除或大部切除术,术后并发症发生率与双侧甲状腺大部切除术相近,而复发率较双侧甲状腺大部切除术低,而且避免了术后终生服药或减少了服药剂量,尤其是保留有一侧甲状腺,具有可反复手术而不会导致严重并发症的优势,是一种值得推荐临床应用的术式。
[1]Olson SE,Starling J,Chen H.Symptomatic benign multinodular goiter:unilateral or bilateral thyroidectomy?[J].Surgery,2007,142(4):458-461.
[2]Cooper DS,Doherty GM,Haugen BR,et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer[J].Thyroid,2009,19(11):1167-1214.
[3]White ML,Doherty GM,Gauger PG.Evidencebased surgical management of substernal goiter[J]. World J Surg,2008,32(7):1285-1300.
[4]Vassiliou I,Tympa A,Arkadopoulos N,et al. Total thyroidectomy as the single surgical option for benign and malignant thyroid disease:a surgical challenge[J].Arch Med Sci,2013,9(1):74-78.
[5]Lang BH,Lo CY.Total thyroidectomy for multinodular goiter in the elderly[J].Am J Surg,2005,190 (3):418-423.
[6]Liu Q,Djuricin G,Prinz RA.Total thyroidectomy for benign thyroid disease[J].Surgery,1998,123(1):2-7.
[7]Moalem J,Suh I,Duh QY.Treatment and prevention of recurrence of multinodular goitre:an evidence-based review of the literature[J]. World J Surg,2008,32(7):1301-1312.
[8]Agarwal G,Aggarwal V.Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review[J].World J Surg,2008,32(7):1313-1324.
[9]Bauer PS,Murray S,Clark N,et al.Unilateral thyroidectomy for the treatment of benign multinodular goiter[J].J Surg Res,2013,184(1):514-518.
[10]Ho TW,Shaheen AA,Dixon E,et al.Utilization of thyroidectomy for benign disease in the United States:a 15-year population-based study[J].Am J Surg,2011,201(5):570-574.
[11]Colak T,Akca T,Kanik A,et al.Total versus subtotal thyroidectomy for the management of benign multinodular goiter in an endemic region[J].ANZ J Surg,2004,74(11):974-978.
[12]Friguglietti CU,Lin CS,Kulcsar MA.Total thyroidectomy for benign thyroid disease[J]. La ryngoscope,2003,113(10):1820-1826.
[13]Vasica G,O'Neill CJ,Sidhu SB,et al. Reoperative surgery for bilateral multinodular goitre in the era of total thyroidectomy[J].Br J Surg,2012,99(5):688-692.
[14]Ozbas S,Kocak S,Aydintug S,et al.Comparison of the complications of subtotal,near total and total thyroidectomy in the surgical management of multinodular goitre[J].Endocr J,2005,52(2):199-205.
[15]Youngwirth L,Benavidez J,Sippel R,et al. Parathyroid hormone deficiency after total thyroidectomy:incidence and time[J].J Surg Res,2010,163(1):69-71.
[16]Stoll SJ,Pitt SC,Liu J,et al.Thyroid hormone replacement after thyroid lobectomy[J]. Surgery,2009,146(4):554-548.
[17]Wadström C,Zedenius J,Guinea A,et al.Multinodular goitre presenting as a clinical single nodule:How effective is hemithyroidectomy?[J]. Aust N Z J Surg,1999,69(1):34-36.
[18]Delbridge L,Guinea AI,Reeve TS.Total thyroidectomy for bilateral benign multinodular goiter:effect of changing practice[J].Arch Surg,1999,134(12):1389-1393.
[19]De Bellis A,Conzo G,Cennamo G,et al.Time course of Graves’ophthalmopathy after total thyroidectomy alone or followed by radioiodine therapy:a 2-year longitudinal study[J]. Endocrine,2012,41(2):320-326.
Comparative study of the treatment of bilateral multinodular goiter between hemithyroidectomy combined with contralateral nodule resection or subtotal resection and bilateral subtotal resection/
CHEN Xiao, XIAO Hui, YU Zheng-ya//China Medical Equipment,2017,14(2):53-56.
Objective:To discuss the appropriate thyroid operation for the treatment of bilateral multinodular goiter.Methods:328 bilateral multinodular goiter patients undergoing surgery in the department of general surgery of Capital Medical University Beijing Tongren Hospital from June 2012 to June 2016. were retrospectively analyzed. Of these patients, 85 underwent hemithyroidectomy combined with contralateral nodule resection or subtotal resection and 243 underwent bilateral subtotal thyroidectomy. The rate of postoperative complications and recurrence between hemithyroidectomy combined with contralateral nodule resection or subtotal resection and bilateral subtotal thyroidectomy were compared.Results:The follow-up time was 1 month to 48 months after operations. In hemithyroidectomy combined with contralateral nodule resection or subtotal resection group 1 patient developed recurrent laryngeal nerve palsy, 2 patients had transient hypoparathyroidism and 1 patient had hematoma in the operative cavity. In bilateral subtotal thyroidectomy group, 2 patients developed recurrent laryngeal nerve palsy and 2 patients had subcutaneous hematoma. The rate of recurrent disease was 2.35%(2 patients) in hemithyroidectomy combined with contralateral nodule resection or subtotal resection group and 7%(17 patients) in bilateral subtotal thyroidectomy group. There was no patient in both groups needed reoperation.Conclusions:Hemithyroidectomy combined with contralateral nodule resection or subtotal resection had similar complication rate compared with bilateral subtotal thyroidectomy, but it had a significantly lower risk of recurrence than bilateral subtotal thyroidectomy, Furthermore, the rest one lobe could be resected for many times which would not cause severe complications. Hemithyroidectomy combined with contralateral nodule resection or subtotal resection is worthed to be recommended.
Multinodular goitergoiter; Subtotal thyroidectomy; Hemithyroidectomy; Recurrence
1672-8270(2017)02-0053-04
R736.1
A
10.3969/J.ISSN.1672-8270.2017.02.016

2016-09-25
①首都医科大学附属北京同仁医院普外科 北京 100730
*通讯作者:chenxiao_china@hotmail.com
陈笑,男,(1969- ),博士,副主任医师。首都医科大学附属北京同仁医院普外科,研究方向:甲状腺乳腺疾病。