Toxoplasma encephalitis and AIDS in a patient with seizure and altered mental status: A case report
Somayeh Valadkhani, Amir Reza Radmard, Morteza Saeedi, Sara Nikpour, Mohammad Reza Farnia
1Emergency Department, Imam Reza Hospital, Kermanshah University of Medical Sciences, Kermanshah 67146, Iran
2Radiology Department, Shariati Hospital, Tehran University of Medical Sciences, Tehran 14117-13137, Iran
3Emergency Department, Shariati Hospital, Tehran University of Medical Sciences, Tehran 14117-13137, Iran
4Forensic Medicine Department, Loghman Hospital, Shahid Beheshti University of Medical Sciences, Tehran 19857-17443, Iran
Letter to the editor
Toxoplasma encephalitis and AIDS in a patient with seizure and altered mental status: A case report
Somayeh Valadkhani1, Amir Reza Radmard2, Morteza Saeedi3, Sara Nikpour4, Mohammad Reza Farnia1
1Emergency Department, Imam Reza Hospital, Kermanshah University of Medical Sciences, Kermanshah 67146, Iran
2Radiology Department, Shariati Hospital, Tehran University of Medical Sciences, Tehran 14117-13137, Iran
3Emergency Department, Shariati Hospital, Tehran University of Medical Sciences, Tehran 14117-13137, Iran
4Forensic Medicine Department, Loghman Hospital, Shahid Beheshti University of Medical Sciences, Tehran 19857-17443, Iran
INTRODUCTION
Increasing incidences of neurological complications are being encountered with the increase in the incidence of human immunodeficiency virus (HIV).[1]These can be due to the direct involvement of the central nervous system (CNS) by the virus or due to other opportunistic infections. Cerebral toxoplasmosis is a common opportunistic infection seen in HIV-infected patients, but it has rarely been encountered before the diagnosis of HIV infection is established.[1]We report a case of altered mental status secondary to acute Toxoplasma gondii encephalitis.
CASE
The patient was a 34-year-old man admitted to the emergency department with fever and altered mental status progressing for two days. His complaints began 7 days before with mild headache; after that he experienced progressive confusion, vomiting and a generalized tonic clonic seizure. The patient's mother denied any major illness, substance abuse or hospitalization of her son in the past, but pointed to one episode of suspicious seizure about 11 months ago, which had not been investigated.
On physical examination the patient was lethargic and quite ill. Upon admission to the emergency department, his body temperature was 38.5 ºC, blood pressure 110/70 mmHg, heart rate 102 beats/minute, respiratory rate 22/minute and oxygen saturation of 94% on room air. Bedside serum glucose level was 98 mg/dL. A focused neurologic exam highlighted drowsiness and time, place and person disorientation, but no focal deficits. The cranial nerves were intact and the patient was able to move all four extremities without limitation. Deep tendon reflexes were normal and there was no ataxia and neck stiffness present. Pupils were midsize and reactive. Limbs exam revealed no skin rash or track marks. Other systems, including cardiac, respiratory, abdominal, and genitourinary examination, were normal. A CT scan of the brain showed hydrocephalus and a hypodense lesion in the midbrain (Figure 1). Primary laboratory workup revealed a normal complete blood count, normal electrolytes, negative urine drug screen and a mildly elevated erythrocyte sedimentation rate (23 mm/hour). The cerebrospinal fluid (CSF) was clear with a protein concentration of 1.08 g/L and a glucose concentration of 4.2 mmol/L. There was no bacterial growth after 48 hours of incubation.
He was started on Phenytoin for seizure prophylaxis, and empiric treatment with Metronidazole and Cefotaxime for possible brain abscess, but he did not respond to treatment. Fever and altered mental status did not improve; so, other causes of ring enhanced brain lesions were investigated. The patient immune system was checked. Rapid HIV antibody test was requested, which revealed a positive result. CD4 count was 186 cell/mm3and subsequent testing conf rmed HIV infection, but anti-toxoplasma IgG and IgM were negative. For further assessment, MRI was performed (Figure 2A and 2B) and showed a ring-enhancinglesion with edema in the left tectal plate of midbrain. Nevertheless, after the infectious disease specialist counselling, the patient was treated with Pyrimethamine, Sulfadiazine, Folic acid and Dexamethasone for cerebral toxoplasmosis. After 6 days of treatment with antitoxoplasmosis therapy, he responded well to the treatment with good neurological recovery and was discharged in two weeks with oral anti-toxoplasmosis regimen and was referred to his primary care physician. Antiretroviral therapy was to be initiated as an outpatient.
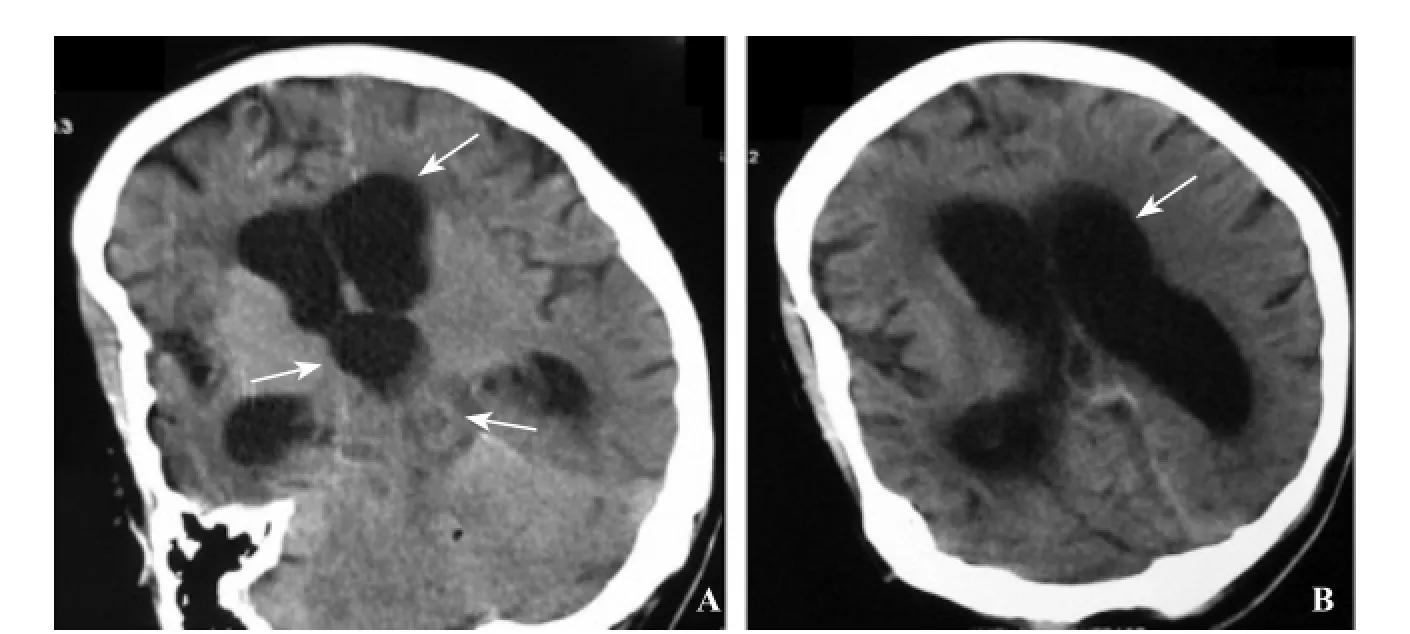
Figure 1. Axial brain CT scan without IV contrast. (A, B) An ill-def ned hypodense lesion is seen in left side of the midbrain extending to tectum (thick arrow), which causes an obstructive supratentorial hydrocephalus (thin arrows).
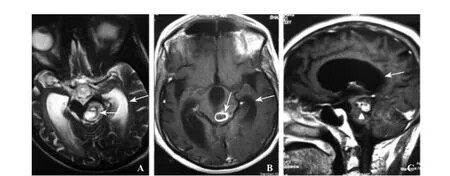
Figure 2. MRI of the brain. A: Axial T2-weighted image shows a hyperintense lesion (thick arrow) in left tectal plate of midbrain with pressure effect on cerebral aqueduct and accompanying peripheral edema. In axial (B) and sagittal (C) post contrast T1-weighted images, there is dominantly peripheral ring enhancement (thin arrow) with a nodular heterogeneous enhancing component in left side (arrowhead) compatible with toxoplasmosis. Secondary dilatation of lateral and third ventricles is also evident (curved arrows) due to mass effect on aqueduct.
After normal mental status recovery, the patient revealed previous IV drug abuse, which he quit two years before. A follow-up MRI after three weeks showed decreased size of lesion and brain edema; subsequently, IgG for toxoplasma was repeated which had a positive result.
DISCUSSION
Neurological manifestations of HIV can occur at any time from viral acquisition to the late stages of AIDS; they are varied and may affect any part of the nervous system including the brain, spinal cord, autonomous nervous system and the peripheral nerves. HIV affects the nervous system in 70%–80% of infected patients.[2]The effect may be due to the direct effect of the virus, opportunistic infections and/or malignancies.
Toxoplasma encephalitis is the neurological disorder most frequently found in HIV/AIDS patients.[3]CT scan of the brain reveals multiple, bilateral, hypodense, contrast-enhancing brain lesions in the majority of patients. Toxoplasma encephalitis may less frequently present with a single lesion or with no lesions on CT scan. MRI is more sensitive than CT scan and thus is the preferred imaging technique.[4]
MRI shows that around 70% of cerebral toxoplasmosis lesions are multifocal. Although considered rare, single lesion may be present in 14% to 17% of AIDS patients.[5]Patients with toxoplasma encephalitis typically exhibit rapid improvement after initiation of appropriate therapy. Neurologic response is noted in 51% of patients by day3, and in 91% of patients by day 14.[6]Most patients will also experience radiologic improvement by the third week of treatment.[7,8]Therefore, neuroradiologic study should be repeated 2–4 weeks after initiation of therapy.
CONCLUSION
There are some teaching points in this case, which can be interesting and useful for emergency physicians:
1) Patients with Toxoplasma encephalitis may have only one lesion or no obvious lesion on CT scan.
2) A negative IgG test result makes the diagnosis very unlikely but does not rule it out.[9]Toxoplasmaspecific IgG antibody levels in AIDS patients often are low to moderate, but occasionally no specific IgG antibodies can be detected. Tests for IgM antibodies are generally negative. If the patient has clinical illness compatible with toxoplasmosis but the IgG titer is low, a follow-up titer two to three weeks later should show an increase in antibody titer if the illness is due to acute toxoplasmosis, assuming the host is not severely immunocompromised.[10]
3) Toxoplasma gondii can affect any part of the brain.
4) CNS toxoplasmosis presenting as hydrocephalus is a very rare entity.[11]
5) Neurological illnesses are the initial manifestation of AIDS in 7% to 20% of patients.[12]So the history of AIDS is not always clear.
Hence, clinicians must consider this possibility before a ring-enhancing space-occupying cerebral lesion, even in patients without prior immunosuppression or an HIV infection history, in order to accomplish early diagnosis and proper treatment administration.
Funding:None.
Ethical approval:Not needed.
Conf icts of interest:All authors declare that they have no conf ict of interest.
Contributors:Valadkhani S drafted the manuscript. All authors read and approved the f nal manuscript.
REFERENCES
1 Vijayvergia V, Bithu R, Singh SK, Maheshwari R. A case of cerebral toxoplasmosis as the initial presentation of HIV infection. Int J Curr Microbiol App Sci. 2016;5:801–803.
2 Federal HIV/AIDS Prevention and Control Office Federal Ministry of Health. Guidelines for management of opportunistic infections and anti retroviral treatment in adolescents and adults in Ethiopia. Betru Tekle (MD): 2008 March.
3 Pereira IA, Ferry FR, Alvarenga RM, Sá CA. Toxoplasma encephalitis after initiation of highly active anti-retroviral therapy. DST–J Bras Doenças Sex Transm. 2008;20:52–58.
4 Naqi R, Azeemuddin M, Ahsan H. Cerebral toxoplasmosis in a patient with acquired immunodeficiency syndrome. J Pak Med Assoc. 2010;60(4):316–8.
5 da Cunha Correia C, Lacerda HR, de Assis Costa VM, de Queiroz Brainer AM. Cerebral toxoplasmosis: unusual MRI f ndings. Clin Imaging. 2012;36(5):462–5.
6 Luft BJ, Hafner R, Korzun AH, Leport C, Antoniskis D, Bosler EM, et al. Toxoplasmic encephalitis in patients with the acquired immunodeficiency syndrome. N Engl J Med. 1993;329(14):995–1000.
7 Levy RM, Rosenbloom S, Perrett LV. Neuroradiologic findings in AIDS: a review of 200 cases. Am J Roentgenol. 1986;147(5):977–83.
8 Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992;327(23):1643–8.
9 U.S. Department of Health and Human Services Health Resources and Services Administration (HRSA). Guide for HIV/ AIDS Clinical Care. Laura W. Cheever (MD) 2014 Apr
10 Global Health-Division of Parasitic Diseases and Malaria [Internet]. Atlanta: Centers for Disease Control and Prevention [updated 2015 August 7; cited 2016 Jul 20] Available from: https://www.cdc.gov/parasites/toxoplasmosis/
11 Basavaprabhu A, Soundarya M, Deepak M, Satish R. CNS toxoplasmosis presenting with obstructive hydrocephalus in patients of retroviral disease-a case series. Med J Malaysia. 2012;67(2):214–6.
12 Bedu-Addo G. Cerebral toxoplasmosis in HIV/AIDS: A case report. West Afr J Med. 2006;25(3):252–3.
Received April 9, 2016
Accepted after revision October 21, 2016
Mohammad Reza Farnia, Email: mr.farnia@kums.ac.ir, dr.farniam@gmail.com
World J Emerg Med 2017;8(1):65–67
10.5847/wjem.j.1920–8642.2017.01.012
 World journal of emergency medicine2017年1期
World journal of emergency medicine2017年1期
- World journal of emergency medicine的其它文章
- Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest
- The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance
- Cardiopulmonary resuscitation knowledge and attitude among general dentists in Kuwait
- Simplif ed point-of-care ultrasound protocol to conf rm central venous catheter placement: A prospective study
- Clinical and historical features of emergency department patients with pericardial effusions
- Comparison of neurological clinical manifestation in patients with hemorrhagic and ischemic stroke
