Simplif ed point-of-care ultrasound protocol to conf rm central venous catheter placement: A prospective study
Sean P. Wilson, Samer Assaf, Shadi Lahham, Mohammad Subeh, Alan Chiem, Craig Anderson, Samantha Shwe, Ryan Nguyen, John C. Fox
1Department of Emergency Medicine, University of California, Irvine, Orange, California 92868, USA
2Department of Emergency Medicine, University of California, Sylmar, Los Angeles, California 91342, USA
Simplif ed point-of-care ultrasound protocol to conf rm central venous catheter placement: A prospective study
Sean P. Wilson1, Samer Assaf1, Shadi Lahham1, Mohammad Subeh1, Alan Chiem2, Craig Anderson1, Samantha Shwe1, Ryan Nguyen1, John C. Fox1
1Department of Emergency Medicine, University of California, Irvine, Orange, California 92868, USA
2Department of Emergency Medicine, University of California, Sylmar, Los Angeles, California 91342, USA
BACKGROUND: The current standard for conf rmation of correct supra-diaphragmatic central venous catheter (CVC) placement is with plain f lm chest radiography (CXR). We hypothesized that a simple point-of-care ultrasound (POCUS) protocol could effectively conf rm placement and reduce time to conf rmation.
METHODS: We prospectively enrolled a convenience sample of patients in the emergency department and intensive care unit who required CVC placement. Correct positioning was considered if turbulent flow was visualized in the right atrium on sub-xiphoid, parasternal or apical cardiac ultrasound after injecting 5 cc of sterile, non-agitated, normal saline through the CVC.
RESULTS: Seventy-eight patients were enrolled. POCUS had a sensitivity of 86.8% (95%CI77.1%–93.5%) and specif city of 100% (95%CI15.8%–100.0%) for identifying correct central venous catheter placement. Median POCUS and CXR completion were 16 minutes (IQR 10–29) and 32 minutes (IQR 19–45), respectively.
CONCLUSION: Ultrasound may be an effective tool to confirm central venous catheter placement in instances where there is a delay in obtaining a conf rmatory CXR.
Point-of-care ultrasound; Emergency ultrasound; Central venous access
INTRODUCTION
Central venous catheter (CVC) placement has been identified as an essential tool in the resuscitation of the critically ill.[1–3]It is estimated that there are on average 5 million CVCs placed annually in the U.S. alone.[4]This nearly widespread use of CVCs allows for the rapid infusion of f uids, delivery of centrally acting medications and active hemodynamic monitoring.[1]Complications are expansive and include catheter tip misplacement.[4]Therefore, following placement, plain f lm chest radiography (CXR) has been largely considered as standard to identify correct catheter tip location.[5]
Point-of-care ultrasound (POCUS) has long been identif ed as a reliable procedural guidance tool to reduce complications associated with CVC placement,[6,7]to identify post-procedure pneumothorax[7–13]and has most recently gained traction as a potential tool to reduce the potential delay of confirmatory post-procedure CXR during supra-diaphragmatic CVC placement.[7–13]However, these current ultrasound protocols to confirm supra-diaphragmatic CVC placement, even without a post-pneumothorax assessment can be complex and cumbersome for some users.
We therefore hypothesized that a simplif ed, single viewPOCUS protocol could identify correct CVC positioning and would be more rapid than standard CXR.
METHODS
Study design, setting and population
This was a prospective evaluation of POCUS to identify correct and timely supra-diaphragmatic CVC placement in a convenience sample of critically ill patients in the emergency department (ED) and intensive care unit (ICU) at an urban, academic level 1 trauma center. Annual census of the ED was 50 000 patients. The study was performed between January 2012 and May 2015. Patients less than 18 years of age or who informed consent was not obtained were excluded. The study site institutional review board approved this study.
Study protocol
Research associates were present in the ED and ICU between the hours of 8 am and midnight to identify and enroll potential study participants. After informed consent, POCUS was performed by resident trainee after CVC placement. Each resident trainee was familiar with obtaining the appropriate cardiac view for the study, but had not necessarily seen turbulent flow before (specific ultrasound protocol is outlined below). A CXR was also performed immediately after CVC placement as per institutional guidelines and in no instance was POCUS to delay obtaining a CXR. Time points were compared between time of ultrasound and CXR completion; the actual time it took to perform the ultrasound from start to finish was not recorded. Accuracy of appropriate placement were compared to radiology interpreted CXR (often delayed many hours, but considered gold standardfor study). Appropriate placement was considered to have occurred if the CVC tip was visualized at or immediately above the right atrium on CXR. Results and all time points were recorded by the research associates.

Figure 1. B-Mode sub-xiphoid view of the heart. RA: right atrium; RV: right ventricle.
Ultrasound protocol
A low frequency (1–5 MHz) phased array probe was used to obtain a parasternal long, apical or subcostal view of the heart with the patient in a supine position. Next, a 5 cc injection of sterile, non-agitated, normal saline was rapidly pushed through one of the ports on the CVC. The CVC was interpreted to be in the appropriate position if echogenic, turbulent flow was visualized by B-Mode sonography within the right atria (Figures 1 and 2) immediately after injection. Sonosite Edge or M-turbo machines were used for image acquisition (FujiFilm Sonosite Inc, Bothell, WA).
Data analysis
Sensitivity and specificity are reported using descriptive statistics, with CXR being considered the gold standard. Comparison between POCUS and CXR mean completion time was found to be least skewed using Wilcoxon signed-test, with clinical significant considered to beP<0.05. Median and IQR ranges are also presented as descriptive statistics. Data analysis was performed using Stata (Version 12.1, Stata Corp, College Station, TX).
RESULTS
Seventy-eight patients were enrolled. Forty (51%) patients were female. Average body mass index was 29. A total of 13 (17%) were placed in the ED, while therest were placed in the ICU. Specific location of supradiaphragmatic CVC placement was as follows: 43 (55%) right internal jugular, 21 (27%) left internal jugular, 9 (12%) left subclavian and 5 (6%) right subclavian. Comparison between CXR and POCUS are outlined in Table 1. There were 2 instances where the central line had a malposition detected on CXR: in the first case there was coiling in the neck with tip extension toward the right atrium and in the second case the central line crossed the midline into the subclavian vein. In both of these instances of malposition POCUS was correctly unable to confirm correct CVC placement (no turbulent f ow seen).
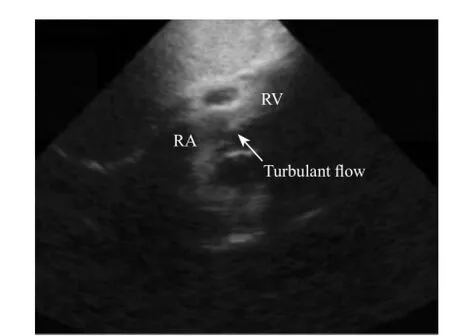
Figure 2. B-Mode sub-xiphoid view of the heart after 5 cc injection of non-agitated normal saline. RA: right atrium; RV: right ventricle.
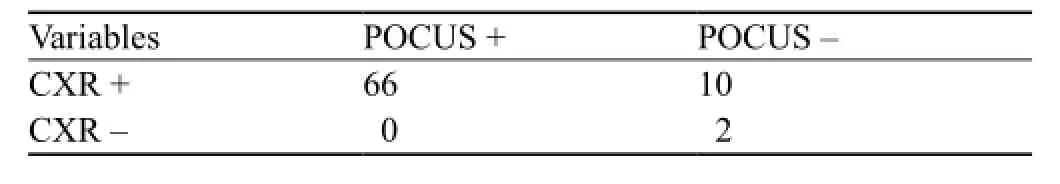
Table 1. Comparison between CXR and POCUS conf rmation of CVC placement
Sensitivity and specif city for POCUS in conf rmation of correct supra-diaphragmatic CVC placement were 86.8% (95%CI77.1%–93.5%) and 100% (95%CI15.8%–100.0%), respectively. Mean time to completion for POCUS was 27.6 (95%CI20.3%–35.0%) minutes and 37.6 (95%CI30.3%–45.0%) minutes for CXR. CXR completion was therefore, on average delayed an additional 10 minutes (P=0.07). Median POCUS and CXR completion were 16 minutes (IQR 10–29) and 32 minutes (IQR 19–45), respectively.
DISCUSSION
Current standards dictate that correct positioning of a supra-diaphragmatic CVC be confirmed by CXR before catheter use. Methods that may reduce time to confirmation or provide an alternative to CXR when unavailable may be able to improve patient care, especially in the critically ill. Recently, multiple studies have demonstrated that with a combination of ultrasound views and injectable materials, POCUS may be able to provide earlier and correct CVC positioning in the superior vena cava.[7,13,14]Vezzani et al[13]illustrated that the use of contrast enhanced, agitated saline could be used to conf rm placement of CVC. This visualization of the echogenic agitated saline allowed for confirmation of correct CVC placement in an average of 10 minutes with 96% sensitivity. Zanobetti et al[14]used a more complex ultrasound protocol with multiple views and also observed correct CVC placement in an average of 5 minutes with 94% sensitivity. Although requiring more views, these studies are also promising for rapid confirmation of supra-diaphragmatic CVC. We believe that in the critically ill patient, who requires immediate central acting vasoactive medications, may benef t from even a reduction in delay of only 5 to 15 minutes.
Our study differed from these previous studies in that it was even further simplified and yet despite this simplification continued to observe with reasonable sensitivity that there is an opportunity for POCUS to provide early confirmation of correct CVC placement. This protocol simplification was achieved through multiple methods. First, we opted to simplify our scanning protocol to only a single cardiac view. This mainly reduced the need to confirm correct vessel cannulation, which is redundant as it should already have been done in a dynamic process during the initial CVC placement. Second, we replaced the use of agitated normal saline or contrast material injection with a sterile, non-agitated normal saline. This simplif ed the injection procedure for the provider as well as reduced the need for any additional training or hospital regulatory efforts of using a contrast enhanced material.
While we were able to appreciate a similar sensitivity, we were not able to appreciate the same time benef t as with the prior studies. In particular, we observed that it took on average relatively longer to perform the ultrasound protocol than that of the prior studies. We suspect this delay was much in part due to the fact that the majority of our studies were performed in the ICU, where the resident trainees may have been less comfortable than our ED counterparts at performing POCUS. Another factor is that the residents performing the ultrasound may have been distracted by other tasks such as order entry, documentation, updating families or providing other patient care which would delay time to POCUS completion. It is also possible that since the ICU has less POCUS equipment per patient, there may have been limited the equipment accessibility to perform the scan. We suspect if this confirmation protocol becomes more validated, there may be more priority to complete a POCUS conf rmation and therefore the time to completion would potentially be reduced signif cantly. Nonetheless, despite this, the median time to POCUS completion was less than that of CXR. It is therefore possible, if we had a higher enrollment we may have been better powered to appreciate a statistical difference in average time between POCUS and CXR.
Limitations
There were several limitations to our study. First, it was performed at a single center with a robust hospital-wide POCUS program. As a result, it is possible that our physician sonographers may be more skilled at image acquisition and interpretation than physicians at other sites. Second, our sonographers were often also those placing the CVC, so they may have experienced an interpretation bias based on their own comfort with the original CVC placement. However, this is hopefully mitigated by the fact that without a confirmatory CXR, they did not know the true success of the procedure. Third, we had only two instances of malposition, though both went appropriately unconfirmed by POCUS. Of particular concern is that, we had no cases of a central line be placed in an innominate or azygous vein, which may still have produced a false positive by visualizing turbulent f ow in the right atrium.
CONCLUSION
Our data suggests that a simple, single cardiac view during injection of non-agitated normal saline may be used to identify correct and rapid confirmation of correct CVC positioning. This may be especially valuable in instances where there is delay in obtaining a conf rmatory CXR.
ACKNOWLEDGMENTS
We thank the Emergency Medicine Research Associates Program and the Medical Intensive Care Unit Research Associates Program for assistance with enrolling patients for this study.
Funding:None.
Ethical approval:The study site institutional review board approved this study.
Conflicts of interest:The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors:Wilson SP proposed the study and wrote the first draft. All authors read and approved the f nal version of the paper.
REFERENCES
1 Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
2 ProCESS Investigators, Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683–93.
3 Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372(14):1301–11.
4 McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):1123–33.
5 Lahham S, Schmalbach P, Wilson SP, Ludeman L, Subeh M, Chao J, et al. Prospective evaluation of point-of-care ultrasound for pre-procedure identif cation of landmarks versus traditional palpation for lumbar puncture. World J Emerg Med. 2016;7(3):173–7.
6 Leung J, Duffy M, Finckh A. Real-time ultrasonographically guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48(5):540–7. Epub 2006 Feb 21.
7 Liu YT, Bahl A. Evaluation of proper above-the-diaphragm central venous catheter placement: the saline flush test. Am J Emerg Med. 2011;29(7):842.e1–3.
8 Prekker ME, Chang R, Cole JB, Reardon R. Rapid conf rmation of central venous catheter placement using an ultrasonographic "bubble test". Acad Emerg Med. 2010;17(7):e85–6.
9 Gekle R, Dubensky L, Haddad S, Bramante R, Cirilli A, Catlin T, et al. Saline Flush Test: can bedside sonography replace conventional radiography for confirmation of above-thediaphragm central venous catheter placement? J Ultrasound Med. 2015;34(7):1295–9.
10 Zanobetti M, Coppa A, Bulletti F, Piazza S, Nazerian P, Conti A, et al. Verif cation of correct central venous catheter placement in the emergency department: comparison between ultrasonography and chest radiography. Intern Emerg Med. 2013;8(2):173–80.
11 Duran-Gehring PE, Guirgis FW, McKee KC, Goggans S, Tran H, Kalynych CJ, et al. The bubble study: ultrasound confirmation of central venous catheter placement. Am J Emerg Med. 2015;33(3):315–9.
12 Weekes AJ, Johnson DA, Keller SM, Efune B, Carey C, Rozario NL, et al. Central vascular catheter placement evaluation using saline flush and bedside echocardiography. Acad Emerg Med. 2014;21(1):65–72.
13 Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, Corradi F. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010;38(2):533–8.
14 Zanobetti AM, Coppa F, Bulletti S, Piazza S, Nazerian P, Conti A, et al. Verification of correct central venous catheter placement in the emergency department: comparison between ultrasonography and chest radiography. Intern Emerg Med. 2013;8(2):173–180.
Received March 6, 2016
Accepted after revision September 8, 2016
Sean P. Wilson, Email: wilsonseanpatrick@gmail.com
World J Emerg Med 2017;8(1):25–28
10.5847/wjem.j.1920–8642.2017.01.004
 World journal of emergency medicine2017年1期
World journal of emergency medicine2017年1期
- World journal of emergency medicine的其它文章
- Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2 260 patients with cardiac arrest
- The association of layperson characteristics with the quality of simulated cardiopulmonary resuscitation performance
- Cardiopulmonary resuscitation knowledge and attitude among general dentists in Kuwait
- Clinical and historical features of emergency department patients with pericardial effusions
- Comparison of neurological clinical manifestation in patients with hemorrhagic and ischemic stroke
- A comparison of perspectives on costs in emergency care among emergency department patients and residents
