Research of serum total and high-molecular-weight adiponectin levels in patients with type 2diabetic retinopathy
Yuan Zhang,Hong-Sheng Bi,Hua-Wei Pan,Xue-Mei Pan,Yue-Qiu Feng,Li Liu,Shu-Mei Wang
·Original article·
Research of serum total and high-molecular-weight adiponectin levels in patients with type 2diabetic retinopathy
Yuan Zhang1,Hong-Sheng Bi2,Hua-Wei Pan3,Xue-Mei Pan2,Yue-Qiu Feng4,Li Liu2,Shu-Mei Wang4
1Center of Evidence-based Medicine,Second Hospital of Shandong University,Jinan 250033,Shandong Province,China
2DepartmentofOcularFundusDisease,AffiliatedEye HospitalofShandongUniversityofTraditionalChinese Medicine,Jinan 250002,Shandong Province,China
3Department of Infectious Disease Control,Center for Disease Control and Prevention of Xiqing,Tianjin 300380,China
4Department of Epidemiology,School of Public Health,Shandong University,Jinan 250012,Shandong Province,China
Correspondenceto:Shu-MeiWang,Departmentof Epidemiology,School of Public Health,Shandong University,44 Wen Hua Xi Road,Jinan 250012,Shandong Province,China.wshm@sdu.edu.cn
目的:探讨血清高分子量脂联素、总脂联素及两者比值与2型糖尿病性视网膜病变的关系,研究非增殖性糖尿病性视网膜病变发生的危险因素。
方法:共374例研究对象纳入本研究,包括88例增殖性糖尿病性视网膜病变患者(PDR)、124例非增殖性糖尿病性视网膜病变患者(NPDR)、78例无视网膜病变的糖尿病患者(DR)和84例健康对照志愿者(对照组)。收集人口学资料、体检及实验室指标,ELISA方法测定血清总脂联素和高分子量脂联素水平。统计学分析方法包括协方差分析和累积logit模型。
结果:对照组的总脂联素水平高于其他三组(修正均数:5.717、3.310、3.288、3.822 ug/ml,F=18.792,P<0.01),PDR组的总脂联素水平高于NPDR组(P<0.05)。对照组的高分子量脂联素水平高于其他三组(修正均数:2.490、1.425、1.409、1.633 ug/ml,F=14.025,P<0.01),其他三组的高分子量脂联素水平的差异无统计学意义(P>0.05)。高分子量脂联素与总脂联素的比值在四组间的差异无统计学意义(F=0.650,P>0.05)。服药史、高水平的高密度脂蛋白胆固醇、总脂联素和高分子量脂联素是NPDR的保护性因素,年老、糖尿病病程长、肿瘤坏死因子-α升高是NPDR的独立危险因素。
结论:较低浓度的血清总脂联素和高分子量脂联素水平可能参与非增殖性糖尿病性视网膜病变的发生,总脂联素水平可能与糖尿病性视网膜病变的严重程度有关。
引用:张媛,毕宏生,潘华伟,潘雪梅,冯月秋,刘力,王束玫. 2型糖尿病性视网膜病变患者血清总脂联素和高分子量脂联素水平研究.国际眼科杂志2016;16(3):403-408
·AIM:To explore the levels of serum total adiponectin,high-molecular-weight(HMW)adiponectin and its ratio in type 2 diabetic retinopathy and to investigate risk factors of non-proliferative diabetic retinopathy.
·METHODS:Three hundred and seventy-four subjects were recruited from an epidemiological survey,including 88 patients with proliferative diabetic retinopathy,124 patients with non-proliferative diabetic retinopathy,78 patients only with type 2 diabetes mellitus and 84 healthy volunteers.Demographics,physicalandlaboratory parameterswerecollected.SerumtotalandHMW adiponectin levels were detected by ELISA.The main statisticalanalysisincludedcovarianceanalysisand cumulative logit model.
·RESULTS:Total adiponectin level was higher in healthy group than in groups of only diabetes,non-proliferative and proliferative diabetic retinopathy(harmonic mean,5.717,3.310,3.288,3.822 μg/ml,F=18.792,P<0.01). Total adiponectininproliferativediabeticretinopathy increasedcomparedwithnon-proliferativediabetic retinopathy(harmonic mean,3.822,3.288 ug/ml,P<0.05).HMW adiponectin level of healthy group is more than other groups(harmonic mean,2.490,1.425,1.409,1.633 μg/ml,F=14.025,P<0.01).HMW adiponectin among only type 2 diabetes mellitus,non-proliferative and proliferativediabeticretinopathygroupshadno differences(P>0.05).The ratio of HMW adiponectin and total adiponectin had no differences among four groups(F=0.650,P>0.05).Drug history,high levels of high densitylipoproteincholesterol,totalandHMW adiponectin had protective effects to the non-proliferative diabetic retinopathy(P<0.05).Older age,long duration of diabetes,high level of tumor necrosis factor-α(TNF-α)were independent risk factors.
·CONCLUSION:The lower concentrations of serum total and HMW adiponectin may result in the occurrence of non -proliferativediabeticretinopathy.Andthetotal adiponectin level was related to the severity of diabetic retinopathy.
adiponectin;high-molecular-weight adiponectin;diabetic retinopathy
INTRODUCTION
A s the leading cause of blindness among working-aged adults,diabeticretinopathy(DR)hasattacked approximately 93 million people worldwide[1].The overall prevalence of DR was 29.7%in Chinese patients with type 2 diabetes mellitus(T2DM),of which 27.3%with nonproliferative diabetic retinopathy(NPDR)and 2.4%with proliferative diabetic retinopathy(PDR)[2].A number of factors,such as poor glycaemic and blood pressure control,lipid concentrations,body mass index(BMI),familial clustering,macrovascular complications and longer diabetes duration,wereallknowntobeinvolvedinDR's progression[1,3-4].
Adiponectin is a novel,adipose-specific protein belonging to thecollectinfamily,andpresentabundantlyinthe circulation[5].Its levels were reported to be low in subjects with obesity,insulin resistance,T2DM,hypertension and cardiovascular diseases[6-8].There are three forms in serum,including a low molecular weight(LMW)trimer,a middle molecular weight(MMW)hexamer,and a multimeric high molecular weight(HMW)form,collectively referred to as total adiponectin[5].Of its isoforms,HMW complex is thought to be the most biologically active form and have more pathophysiological relevance in humans[9].However,some clinicalstudiesabouttherelationshipbetweentotal adiponectin concentration and DR were inconsistent.Yilmaz et al[10]showed plasma adiponectin concentrations in patients with NPDR or PDR were significantly lower than those in patients without retinopathy.Hotta et al[11]reported that the presenceofmicroangiopathydidnotaffecttheplasma adiponectin levels in diabetic patients.In contrast,Kato et al[12]and Komaba et al[13]reported total or HMW adiponectin is increased in T2DM with retinopathy.Only one study has taken HMW/total adiponectin ratio into account in DR[12]. We found some of these studies neither control variables impacting adiponectin nor observe the dynamic trend of adiponectin from healthy status,T2DM to different stages of DR.Therefore,in our study,we aimed to explore how the serum total adiponectin,HMW adiponectin and their ratio change with the progression of T2DM and DR,and further explored the risks of NPDR.
SUBJECTS AND METHODS
Study Design and Subjects To meet the needs of research,we calculated the sample size according to the special formula.With an alpha 0.05(two-sided test)and 90% power,at least 59 subjects were needed in each group.The definitions of T2DM and DR were used as follows.T2DM was diagnosed based on the Global Guideline from WHO and InternationalDiabetesFederation,whichwasagreed implementation by Chinese Diabetes Society[14].Diabetic retinopathy was divided into two stages based on severity,including NPDR and PDR.NPDR is the early stage of DR. The damaged retinal blood vessels leak fluid and blood into the surrounding retina.PDR is the advanced stage and the majorcauseofblindnessindiabetics,followedwith neovascularization,vitreoushemorrhage,scartissue hyperplasia,secondary retinal detachment and blindness[15]. InAffiliatedEyeHospitalofShandongUniversityof TraditionalChineseMedicine,thedetailedhistoryand physical examination was carried out for every patient and volunteer.Gender,age,diabetes duration,disease history,family history and drug history,height,weight and arterial blood pressure were evaluated.BMI was ratio of weight and height's square.It was worth mentioning that every subject underwent ophthalmoscopic examination and fasting plasma glucose(FPG)levels were measured.They were then stratified into subgroups.
Finally,88 patients with proliferative diabetic retinopathy,124 patients with non-proliferative diabetic retinopathy,78 patients only with T2DM and 84 healthy controls were recruited.All subjects were informed of the study purpose and their consent was obtained.The study was approved separately by the ethics committee of School of Public Health of Shandong University and Affiliated Eye Hospital of Shandong University of Traditional Chinese Medicine.
Sample Collection and Laboratory Assays Fasting venous blood samples were collected and immediately centrifuged to serum at 1000g for 15min at normal atmospheric temperature,and kept frozen at-80℃until assay analysis.All laboratory examinations were done by technicians of Medical Laboratory in Shandong University.Serum concentrations of FPG were determined by glucose oxidase method.Triglyceride(TG),total cholesterol(T-C),high density lipoprotein cholesterol(HDL-C),low density lipoprotein cholesterol(LDL-C)were measured by enzyme chromatometry.Creatinine was assayed bytrinitrophenalchromatometry.Fastinginsulin(FINS)and tumor necrosis factor-α(TNF-α)were determined by radioimmunity.
Serum total and HMW adiponectin were measured using a sandwich enzyme-linked immunosorbent assay(ELISA)kit(Innogent Bioscience Inc.,Shenzhen,China).Determination of the latter needed pre-treatment of serum with special digestive juice.Absorbances were measured using multiskan MK3 microplate reader(Thermo Labsystems Inc.,USA).
Statistical Analysis Results were reported as numbers or mean±standard deviation.χ2test was used for discrete variables.Levene's test was used to evaluate the distribution of continuous variables.One-way analysis of variance(ANOVA)was for homogeneity of variance and Kruskal-Wallis rank sum test(H test)for heterogeneity of variance. By covariance analysis,after controlling factors influencing the adiponectin,we observed the harmonic mean of total and HMW adiponectin within groups.Cumulative logit model was used for risks analysis.All analyses were performed using SAS(version 9.4,SAS Institute,Cary,NC,USA),and the P<0.05 was statistically significant.
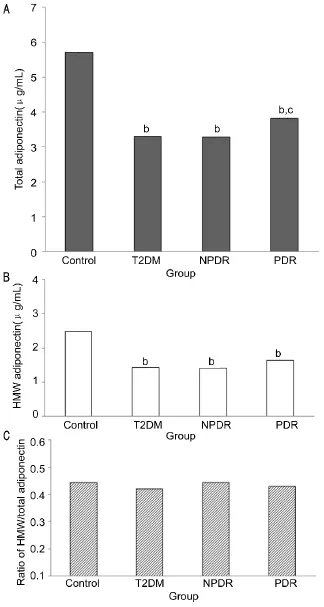
Figure 1 Serumlevelsoftotaladiponectin A:HMW adiponectin;B:HMW adiponectin ratio;C:HMW adiponectin among groups of control,T2DM,NPDR and PDR.bP<0.01 vs control group,cP<0.05 vs NPDR group.
RESULTS
Baseline Characteristic of Healthy Controls and T2DM Subjects with Absence or Presence of Retinopathy Demographic,clinical and laboratory data of the patients and controls are shown in Table 1.No significant differences were observed among four groups in sex,diabetic family history,BMI,LDL-C,systolic blood pressure,diastolic blood pressure,ratio of HMW and total adiponectin(P>0.05).
Age in DR groups was higher than T2DM and control group(P<0.01);diabetic duration was also longer in DR groups(P<0.01);FPG in control group was lower(P<0.01),but other three groups had no different because they all took antidiabetic drugs(P>0.05);FINS was higher in DR groups(P<0.01);T-C,TG and HDL-C had some differences(P<0.01);TNF-α was higher in NPDR group than in T2DM and control groups(P<0.01);with the aggravation of disease,creatinine had a gradual increase(P<0.01);highest levels of total and HMW adiponectin appeared in control group(P<0.01).
Serum Total and HMW Adiponectin Levels in T2DM Retinopathy taking the factors which affected adiponectin into account,and to observe the real levels of total adiponectin,HMWadiponectinandtheirratio,wecontrolled interferences,includingsignificantdifferencesofage,hypertension history,drug history,duration of diabetes,FPG,FINS,TC,TG,HDL-C,TNF-α and creatinine(P<0.05).And we put them as covariates and made covariance analysis.
As shown in Figure 1A and Figure 1B,it revealed that total adiponectin level of healthy group was higher than groups of only T2DM,NPDR and PDR(harmonic mean,5.717,3.310,3.288,3.822 μg/ml,F=18.792,P<0.01).Total adiponectin in PDR increased compared with NPDR(P<0.05).Similarly,HMW adiponectin level of healthy group was more than other groups(harmonic mean,2.490,1.425,1.409,1.633 μg/ml,F=14.025,P<0.01).But HMW adiponectin among groups of T2DM,non-proliferative and proliferative diabetic retinopathy had no differences(P>0.05).From healthy people to diabetic retinopathy patients,the trends of total and HMW adiponectin were down at first and then up.In stage of NPDR,both were the lowest.Figure 1C showed that the ratio of HMW adiponectin and total adiponectin had no differences within groups(0.445,0.422,0.444,0.432,F=0.650,P>0.05).
Analysis of Risk Factors of Non-proliferative Diabetic Retinopathy Cumulative logit model was used for ordinal variables according to the severity of disease,including healthy control,T2DM and NPDR.We put above significant parametersintothismodel.BecausetotalandHMW adiponectin had close co-linear,analysis was made twice respectively.Model was good(likelihood ratio test,P<0.05;goodness-of-fit test,Pearson P>0.05,Deviance P>0.05). Finally,seven variables were retained(P<0.05).Estimate,odds ratio(OR)and P value demonstrated comprehensively that drug history,high level of HDL-C,total and HMW adiponectin had protective effects to NPDR.Older age,long duration of diabetes,high level of TNF-α were independent risk factors.Results are shown in Table 2 and Table 3.

Table 1 Demographic,clinical and laboratory characteristics of the patients and controls

Table 2 Total adiponectin and other factors of non-proliferative diabetic retinopathy

Table 3 HMW adiponectin and other factors of non-proliferative diabetic retinopathy
DISCUSSION
DR is a microangiopathy of the retina from which nearly all diabetic patients eventually suffer.Regular ophthalmological examinations,timely laser therapy depending on the stage of the disease,andcloseinterdisciplinarycooperationare essential to prevent visual loss[15].Adiponectin is a key adipocytokine in T2DM and DR[5].It was discovered during gene-expression profiling of human adipose tissue conducted by the human cDNA project.Located on chromosome 3q27,a locus fordiabetessusceptibility,adiponectinencodesa polypeptide of 247 amino acids with a secretory signal sequence at the amino terminus,a collagenous region(Gly-XY repeats),and a globular domain[16].It exists as full-lengthorasmaller,globularfragment;however,almostall adiponectin appears to exist as full-length adiponectin in plasma.Adiponectin belongs to a family of proteins possessing a collagen-like domain and can be divided to three styles by different molecular weight,including LMW trimer,MMW hexamer and a multimeric HMW form[17].
Our findings in this study were that serum total adiponectin was decreased in T2DM and diabetic retinopathy compared with healthy controls.The levels of total adiponectin in PDR higher than NPDR illustrated that it was positively correlated withtheprogressionofdiabeticretinopathy.Scilicet,hypoadiponectinemia was closely related to the occurrence of diabetic retinopathy,which was consistent with Kato et al's[12]and Pradeepa et al's[18]studies.The mechanism may be a physiological response to mitigate retinal microvascular injury and to prevent the further progression of diabetic retinopathy through its anti-inflammatory and anti-atherogenic effects. On the other hand,when proliferative diabetic retinopathy appeared,diabetic nephropathy often accompanied.Serum adiponectinincreasedintheendstageofdiabetic nephropathy[19].Inthisstudy,serumcreatininelevels increased gradually up to 71.93 umol/L in the group of PDR. This maybe renal function was damaged to some extent and the rate of clearance to adiponectin reduced,resulting in total serum adiponectin rising in serum.
Serum HMW adiponectin levels were also found to be associated with diabetic retinopathy,independent of age,hypertension history,drug history,duration of diabetes,FPG,FINS,TC,TG,HDL-C,TNF-α and creatinine.In response to endothelial dysfunction,it may be increased compensatorily to repair microvascular lesions because one report considered that it induces endothelia nitric oxide production in vitro[20].Conversely,HMW adiponectin may worsen diabetic microangiopathies,although this appears to be contrary to the concept of adiponectin as a beneficial hormone todiabetesandcardiovasculardisease[6-8].Diabetic retinopathy itselfisachroniclong-term inflammatory reaction[21].HMW adiponectin was reported to have dual action,both pro and anti-inflammatory.An initial period of NF-κBactivationbyHMWadiponectinmightbe proinflammatory,but it could be counteracted by activation of AMP-activated protein kinase(AMPK)/eNOS,which lead to a potential reduction in a second activation of NF-κB against inflammatory stimuli[22].In short,that increase of adiponectin is cause or result of the serious stage of diabetic retinopathy needs to be studied further.
The ratio of HMW adiponectin and total adiponectin had no differences within T2DM and its retinopathy.Kato et al[12]also said the ratio was not correlated with the diabetic retinopathy stage.Ratio of plasma level of HMW adiponectin to that of total adiponectin had better predictive power for the prediction of insulin resistance and metabolic syndrome than plasma total adiponectin level[9].This relationship may be existed only in diabetic macrovascular disease,not in microvascular disease. In study of diabetic retinopathy risks,we found drug history, high level of HDL-C,total and HMW adiponectin had protective effects to the non-proliferative diabetic retinopathy. Older age,long duration of diabetes,high level of TNF-α wereriskfactors.Thesewereconsistenttosome researches[1,23-24].
The study had several limitations.Firstly,because of the casecontrol study,we cannot determine the causal relationship between total or HMW adiponectin and diabetic retinopathy. Prospective in-depth investigations with larger sample sizes are required to clear this important question[25].Secondly,whether HMW adiponectin involved in the inflammatory process of diabetic retinopathy requires further study.
In summary,the results from our study suggested that serum total adiponectin and HMW adiponectin were the chief contributors to the generation of both type 2 diabetes and nonproliferative diabetic retinopathy.Future prospective studies with greater numbers of patients are recommended to establish adirectrelationshipbetweenserumadiponection concentrations and the severity of diabetic retinopathy.
REFERENCES
1 Yau JW,Rogers SL,Kawasaki R,Lamoureux EL,Kowalski JW,Bek T,Chen SJ,Dekker JM,Fletcher A,Grauslund J,Haffner S,Hamman RF,Ikram MK,Kayama T,Klein BE,Klein R,Krishnaiah S,Mayurasakorn K,O'Hare JP,Orchard TJ,Porta M,Rema M,Roy MS,Sharma T,Shaw J,Taylor H,Tielsch JM,Varma R,Wang JJ,Wang N,West S,Xu L,Yasuda M,Zhang X,Mitchell P,Wong TY;Meta-Analysis for Eye Disease(META-EYE)Study Group.Global prevalence and major risk factors of diabetic retinopathy.Diabetes care 2012;35(3): 556-564
2 He BB,Wei L,Gu YJ,Han JF,Li M,Liu YX,Bao YQ,Jia WP. Factors associated with diabetic retinopathy in Chinese patients with type
2 diabetes mellitus.Int J Endocrinol 2012;2012:157940
3 Ellis D,Burgess PI,Kayange P.Management of diabetic retinopathy. Malawi Med J 2013;25(4):116-120
4 Zheng W.Factor analysis of diabetic retinopathy in Chinese patients. Diabetes Res Clin Pract 2011;92(2):244-252
5 Okamoto Y,Kihara S,Funahashi T,Matsuzawa Y,Libby P. Adiponectin:a key adipocytokine in metabolic syndrome.Clin Sci 2006;110(3):267-278
6 Fasshauer M,Paschke R,Stumvoll M.Adiponectin,obesity,and cardiovascular disease.Biochimie 2004;86(11):779-784
7 Kadowaki T,Yamauchi T,Kubota N,Hara K,Ueki K,Tobe K. Adiponectin and adiponectin receptors in insulin resistance,diabetes,and the metabolic syndrome.J Clin Invest 2006;116(7):1784-1792
8 Iwashima Y,Katsuya T,Ishikawa K,Ouchi N,Ohishi M,Sugimoto K,Fu Y,Motone M,Yamamoto K,Matsuo A,Ohashi K,Kihara S,FunahashiT,RakugiH,MatsuzawaY,OgiharaT. Hypoadiponectinemia is an independent risk factor for hypertension. Hypertension 2004;43(6):1318-1323
9 Hara K,Horikoshi M,Yamauchi T,Yago H,Miyazaki O,Ebinuma H,Imai Y,Nagai R,Kadowaki T.Measurement of the high-molecular weight form of adiponectin in plasma is useful for the prediction of insulin resistance and metabolic syndrome.Diabetes care 2006;29(6):1357-1362
10 Yilmaz MI,Sonmez A,Acikel C,Celik T,Bingol N,Pinar M,Bayraktar Z,Ozata M.Adiponectin may play a part in the pathogenesis of diabetic retinopathy.Eur J Endocrinol 2004;151(1):135-140
11 Hotta K,Funahashi T,Arita Y,Takahashi M,Matsuda M,Okamoto Y,Iwahashi H,Kuriyama H,Ouchi N,Maeda K,Nishida M,KiharaS,Sakai N,Nakajima T,Hasegawa K,Muraguchi M,Ohmoto Y,Nakamura T,YamashitaS,HanafusaT,MatsuzawaY.Plasma concentrations of a novel,adipose-specific protein,adiponectin,in type 2 diabetic patients.Arterioscler Thromb Vasc Biol 2000;20(6):1595-1599
12 Kato K,Osawa H,Ochi M,Kusunoki Y,Ebisui O,Ohno K,Ohashi J,Shimizu I,Fujii Y,Tanimoto M,Makino H.Serum total and high molecular weight adiponectin levels are correlated with the severity of diabetic retinopathy and nephropathy.Clin Endocrinol(Oxf)2008;68(3):442-449
13 Komaba H,Igaki N,Goto S,Yokota K,Doi H,Takemoto T,Kohno M,Hirosue Y,Goto T.Increased serum high-molecular-weight complex of adiponectin in type 2 diabetic patients with impaired renal function. Am J Nephrol 2006;26(5):476-482
14 Chinese Diabetes Society.Guidelines for the prevention and treatment of type 2 diabetes in China(2010 Edition).Chin J Diabetes 2012;20(1):1227-1245
15 Kollias AN,Ulbig MW.Diabetic retinopathy:Early diagnosis and effective treatment.Dtsch Arztebl Int 2010;107(5):75-83
16 Shehzad A,Iqbal W,Shehzad O,Lee YS.Adiponectin:regulation of its production and its role in human diseases.Hormones(Athens)2012;11(1):8-20
17 Kadowaki T,Yamauchi T.Adiponectin and adiponectin receptors. Endocr Rev 2005;26(3):439-451
18 Pradeepa R,Surendar J,Indulekha K,Chella S,Anjana RM,Mohan V.Associationofserumadiponectinwithdiabeticmicrovascular complications among south Indian type 2 diabetic subjects-(CURES-133).Clin Biochem 2015;48(1-2):33-38
19 Todd Leff,James G;Granneman.Adipose Tissue in Health and Disease.Wiley Blackwell 2010
20 Cheng KK,Lam KS,Wang Y,Huang Y,Carling D,Wu D,Wong C,Xu A.Adiponectin-induced endothelial nitric oxide synthase activation and nitric oxide production are mediated by APPL1 in endothelial cells.Diabetes 2007;56(5):1387-1394
21 Grigsby JG,Cardona SM,Pouw CE,Muniz A,Mendiola AS,Tsin AT,Allen DM,Cardona AE.The role of microglia in diabetic retinopathy.J Ophthalmol 2014;2014:1-15
22 Hattori Y,Nakano Y,Hattori S,Tomizawa A,Inukai K,Kasai K. High molecular weight adiponectin activates AMPK and suppresses cytokine-induced NF-kappaB activation in vascular endothelial cells. FEBS Lett 2008;582(12):1719-1724
23 Al-Rubeaan K,Abu El-Asrar AM,Youssef AM,Subhani SN,Ahmad NA,Al-Sharqawi AH,Alguwaihes A,Alotaibi MS,Al-Ghamdi A,Ibrahim HM.Diabetic retinopathy and its risk factors in a society with a type 2 diabetes epidemic:a Saudi National Diabetes Registry-based study.Acta Ophthalmol 2015;93(2):e140-147
24 Joussen AM,Poulaki V,Mitsiades N,Kirchhof B,Koizumi K,Döhmen S,Adamis AP.Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-alpha suppression.FASEB J 2002;16(3):438-440
25 Fan X,Wu Q,Li Y,Hao Y,Ning N,Kang Z,Cui Y,Liu R,Han L.Associationbetweenadiponectinconcentrationsanddiabetic retinopathy in patients with type 2 diabetes:a meta analysis.Chin Med J(Engl)2014;127(4):765-771
2型糖尿病性视网膜病变患者血清总脂联素和高分子量脂联素水平研究
张 媛1,毕宏生2,潘华伟3,潘雪梅2,冯月秋4,刘 力2,王束玫4
济南青年科技明星计划(201406014)
(1250033中国山东省济南市,山东大学第二医院循证医学中心;2250002中国山东省济南市,山东中医药大学附属眼科医院眼底病内科;3300380中国天津市,西青区疾病预防控制中心传染病控制科;4250012中国山东省济南市,山东大学公共卫生学院流行病学系)
张媛,山东大学公共卫生学院,硕士,主治医师,研究方向:临床流行病学。
王束玫,山东大学公共卫生学院,博士,教授,研究方向:临床流行病学.wshm@sdu.edu.cn
脂联素;高分子量脂联素;糖尿病性视网膜病变
10.3980/j.issn.1672-5123.2016.3.02
Zhang Y,Bi HS,Pan HW,Pan XM,Feng YQ,Liu L,Wang SM.Research of serum total and high-molecular-weight adiponectin levels in patients with type 2 diabetic retinopathy.Guoji Yanke Zazhi(Int Eye Sci)2016;16(3):403-408
Supported by the Ji'nan Youth Star Project of Science and Technology(201406014)
2015-04-06 Accepted:2015-08-20

