IGF-1、HMGB-1、GSN和MIF水平在高血压脑出血中的意义
王京娥 陈燕 高山 周兴盛 乔叶红
·论著·
IGF-1、HMGB-1、GSN和MIF水平在高血压脑出血中的意义
王京娥陈燕高山周兴盛乔叶红
目的观察血清胰岛素样生长因子(IGF)-1、高迁移率族蛋白(HMGB)-1、凝溶胶蛋白(GSN)和巨噬细胞移动抑制因子(MIF)检测在高血压性脑出血患者中意义。方法选择2013年1月至2015年6月诊治的高血压性脑出血患者78例,为高血压性脑出血组。根据神经功能损伤程度分为轻度17例,中度36例和重度25例。根据脑出血量分为:小量出血组36例,中量出血组27例和大量出血组15例。根据格拉斯哥预后评分将出院患者分为:预后良好组43例和预后不良组35例。选择同期就诊单纯脑出血患者和单纯高血压患者分别为脑出血组(45例)和高血压组(35例)。选择同期在我院健康体检者30例为健康对照组。观察高血压性脑出血组,脑出血组,高血压组和健康对照组的血清IGF-1、HMGB-1、GSN和MIF水平,高血压性脑出血患者血清IGF-1、HMGB-1、GSN和MIF水平与神经功能缺损评分和脑出血面积的关系,各指标与预后和各指标之间的相关性分析。结果高血压脑出血组的IGF-1和GSN水平明显低于脑出血组,高血压组和健康对照组(P<0.01),高血压组和脑出血组的水平明显低于健康对照组(P<0.01);高血压脑出血组的HMGB-1和MIF水平明显高于脑出血组,高血压组和健康对照组(P<0.01),高血压组和脑出血组的水平明显高于健康对照组(P<0.01)。高血压脑出血患者的IGF-1和GSN水平随着神经损害程度和脑出血面积的增加而降低(P<0.01),预后良好组的IGF-1和GSN水平明显高于预后不良组(P<0.01),而HMGB-1和MIF水平神经损害程度和脑出血面积增加而升高(P<0.01),预后良好组的HMGB-1和MIF水平明显低于预后不良组(P<0.01)。并发现IGF-1水平与HMGB-1(r=-0.457,P<0.05)和MIF(r=-0.536,P<0.05)呈负相关,与GSN呈正相关(r=0.754,P<0.05);HMGB-1水平与GSN呈负相关(r=-0.486,P<0.05),与MIF呈正相关(r=0.864,P<0.05),GSN与MIF呈负相关(r=-0.758,P<0.05)。结论IGF-1、HMGB-1、GSN和MIF参与了高血压性脑出血疾病的发生发展,对于判断高血压脑出血的病情和预后具有重要意义。
脑出血;高血压;胰岛素样生长因子-1;高迁移率族蛋白-1;凝溶胶蛋白;巨噬细胞移动抑制因子
levels in hypertensive intracerebral hemorrhage group were decreased with the increase of the severity of nervous lesion and cerebral hemorrhage area (P<0.01).The levels of IGF-1 and GSN in good prognosis group were significantly higher than those in poor prognosis group (P<0.01),but the levels of HMGB-1 and MIF were increased with the increase of the severity of nervous lesion and cerebral hemorrhage area (P<0.01).The levels of HMGB-1 and MIF in good prognosis group were significantly lower than those in poor prognosis group (P<0.01).Besides the levels of IGF-1 were negatively correlated to those of HMGB-1 (r=0.457,P<0.05) and to MIF (r=0.536,P<0.05), however,which were positively correlated to those of GSN (r=0.754,P<0.05).The levels of HMGB-1 were negatively correlated to those of GSN (r=0.486,P<0.05),however,which were positively correlated to those of MIF (r=0.864,P<0.05), moreover, the GSN levels were negatively correlated to those of MIF (r=0.758,P<0.05).ConclusionThe IGF-1, HMGB-1, GSN and MIF are involved in the pathogenesis and development of hypertensive cerebral hemorrhage diseases, which play an important role in evaluating the severity and prognosis of hypertensive intracerebral hemorrhage.
脑出血患者由于血肿引起的占位性效应,同时伴有一系列的神经,血液循环和代谢的紊乱,引起脑组织的缺血缺氧,引起全身的炎性反应,继而引起继发性脑损伤,具有较高致残率和致死率。高迁移率族蛋白(HMGB)-1在脑出血后疾病的发生发展过程中具有重要作用,参与机体的炎症发生发展过程[1]。胰岛素样生长因子(IGF)-1 和巨噬细胞移动抑制因子(MIF)在神经细胞,血清和脑脊液中具有稳定的浓度,在急性脑损伤时出现明显的浓度变化,说明IGF-1和MIF可能是神经损伤的重要标志[2,3]。凝溶胶蛋白(GSN)可以清除机体机体损伤后释放的肌动蛋白,对组织损伤具有保护作用,并对脑出血的患者研究发现对疾病严重程度的评估和预后具有重要意义[4]。本组通过观察高血压脑出血患者血清中IGF-1、HMGB-1、GSN和MIF水平的变化,并观察各指标之间的相互联系。
1 资料与方法
1.1一般资料选择2013年1月至2015年6月在我院诊治的高血压性脑出血患者78例,为高血压性脑出血组。均能符合高血压性脑出血的诊断,均在6 h内入院;无心肝肾等重要脏器功能损害;无肝炎,结核和肺炎等急慢性感染疾病;生存期均超过7 d;无合并脑梗死和脑疝;均知情同意;排除有继发性高血压;排除有血液系统和肿瘤等疾病。其中,男42例,女36例;年龄45~80岁,平均年龄(64.83±7.39)岁;平均出血出血量(39.76±6.88)ml;出血部位:基底节35例,枕叶21例,颞叶13例和额叶9例。根据神经功能损伤程度分为轻度17例,中度36例和重度25例。根据脑出血量分为:小量出血组(30~45 ml)36例,中量出血组(46~60 ml)27例和大量出血组(超过60 ml)15例。根据格拉斯哥预后评分(GOS)将出院患者分为:预后良好组(GOS 4~5分)43例和预后不良组(GOS 1~3分)35例。选择同期在我院就诊单纯脑出血患者45例,为脑出血组,其中男25例,女20例;年龄45~80岁,平均年龄(65.16±8.73)岁;平均出血量(39.97±7.72)ml;出血部位:基底节20例,枕叶12例,颞叶7例和额叶6例。选择同期在我院就诊单纯高血压患者35例,为高血压组,男19例,女16例;平均年龄(66.16±7.87)岁。选择同期在我院健康体检者30例,为健康对照组,男16例,女14例;年龄45~80岁,平均年龄(65.55±6.87)岁。4组在年龄、性别比等一般资料差异无统计学意义(P>0.05),具有可比性。
1.2方法
1.2.1神经功能缺损评分:入院后采用美国国立健康研究所制定的急性脑卒中评定表(NIHSS):评分1~4分为轻型组,5~20分为中度组,大于20分为重度组。
1.2.2血液标本的保存和检测:78例均入院时采集外周静脉血约3 ml,注入不含抗凝剂的真空采血管,放置在室温30 min后,采用离心机以3 500 r/min的速度离心,收集血清放置在-80℃的冰箱中待测。采用免疫放射分析法测定IGF-1、HMGB-1、GSN和MIF,试剂盒购自美国BioSource公司,操作步骤严格按照试剂盒操作。
1.2.3观察指标:观察高血压性脑出血组,脑出血组,高血压组和健康对照组的血清IGF-1、HMGB-1、GSN和MIF水平,高血压性脑出血患者血清IGF-1、HMGB-1、GSN和MIF水平与神经功能缺损评分和脑出血面积的关系,各指标与预后和各指标之间的相关性分析。

2 结果
2.14组IGF-1、HMGB-1、GSN和MIF水平的变化高血压脑出血组的IGF-1和GSN水平明显低于脑出血组,高血压组和健康对照组(P<0.01),高血压组和脑出血组的水平明显低于健康对照组(P<0.01);高血压脑出血组的HMGB-1和MIF水平明显高于脑出血组,高血压组和健康对照组(P<0.01),高血压组和脑出血组的水平明显高于健康对照组(P<0.01)。见表1。

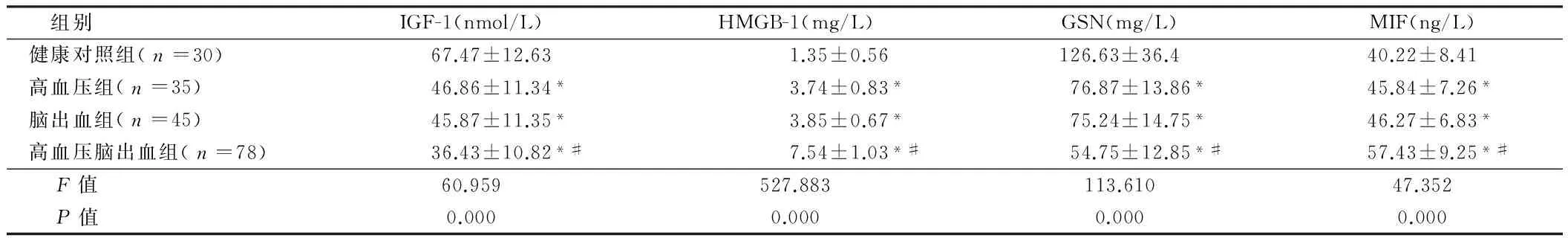
组别IGF-1(nmol/L)HMGB-1(mg/L)GSN(mg/L)MIF(ng/L)健康对照组(n=30)67.47±12.631.35±0.56126.63±36.440.22±8.41高血压组(n=35)46.86±11.34*3.74±0.83*76.87±13.86*45.84±7.26*脑出血组(n=45)45.87±11.35*3.85±0.67*75.24±14.75*46.27±6.83*高血压脑出血组(n=78)36.43±10.82*#7.54±1.03*#54.75±12.85*#57.43±9.25*# F值60.959527.883113.61047.352 P值0.0000.0000.0000.000
注:与健康对照组比较,*P<0.01;与高血压组和脑出血组比较,#P<0.01
2.2高血压脑出血患者血清IGF-1、HMGB-1、GSN和MIF水平的与神经损伤程度的关系高血压脑出血患者的IGF-1和GSN水平随着神经损害程度的升高而降低(P<0.01),而HMGB-1和MIF水平神经损害程度升高而升高(P<0.01)。见表2。

表2 高血压脑出血患者血清IGF-1、HMGB-1、GSN和MIF水平的与神经损伤程度的关系 ±s
注:与健康对照组比较,*P<0.01;与高血压组和脑出血组比较,#P<0.01
2.3高血压脑出血患者血清IGF-1,HMGB-1,GSN和MIF水平的与脑出血量的关系高血压脑出血患者的IGF-1和GSN水平随着脑出血量增加而降低(P<0.01),而HMGB-1和MIF水平随着出血量增加而增加(P<0.01)。见表3。
表3高血压脑出血患者血清IGF-1、HMGB-1、GSN和MIF水平的与脑出血量的关系


组别IGF-1(nmol/L)HMGB-1(mg/L)GSN(mg/L)MIF(ng/L)小量出血组(n=36)42.75±12.175.54±0.3765.35±15.8366.46±9.43中量出血组(n=27)36.86±10.73*7.49±0.89*53.17±13.37*52.53±8.88*大量出血组(n=15)20.49±8.31*#12.43±1.65*#32.15±10.18*#44.58±7.06*# F值24.208330.84133.82342.452 P值0.0000.0000.0000.000
注:与小量出血组比较,*P<0.01;与中量出血组比较,#P<0.01
2.4血清IGF-1,HMGB-1,GSN和MIF水平与高血压脑出血预后的关系高血压脑出血患者预后良好组的IGF-1和GSN水平明显高于预后不良组(P<0.01),而HMGB-1和MIF水平明显低于预后不良组(P<0.01)。见表4。
表4血清IGF-1、HMGB-1、GSN和MIF水平与高血压脑出血预后的关系


组别IGF-1(nmol/L)HMGB-1(mg/L)GSN(mg/L)MIF(ng/L)预后良好组(n=43)41.75±11.726.74±0.7661.86±12.8351.75±8.34预后不良组(n=35)29.89±9.738.52±1.6346.01±14.6764.41±9.17 t值4.7916.3685.0886.377 P值0.0000.0000.0000.000
2.5高血压脑出血患者的IGF-1,HMGB-1,GSN和MIF水平关系高血压脑出血患者的IGF-1,HMGB-1,GSN和MIF指标之间相关性分析,发现IGF-1与HMGB-1(r=-0.457,P<0.05)和MIF(r=-0.536,P<0.05)呈负相关,与GSN(r=0.754,P<0.05)呈正相关;HMGB-1与GSN(r=-0.486,P<0.05)呈负相关,与MIF(r=0.864,P<0.05)呈正相关,GSN与MIF(r=-0.758,P<0.05)呈负相关。
3 讨论
本组研究表明高血压脑出血组的IGF-1水平明显高于脑出血组和高血压组,并且随着脑出血面积和脑组织损伤程度的增加而降低,说明IGF-1的表达参与了脑出血的病理生理过程,与文献报道高血压脑出血患者血清的IGF-1的水平明显低于对照组[5]一致。IGF-1是调节神经生长的生物活性物质,不仅为大脑发育所必需,而且在脑缺血的状态下减轻对中枢神经系统的损伤,对神经系统的生长发育具有重要的作用。现有研究表明脑出血患者在在2 h机体出现IGF-1表达的增加,24 h达到高峰,7 d基本恢复正常[6]。现有的研究表明IGF-1不仅在保护和减少继发性神经元的丧失,而且在保护胶质细胞的增殖方面具有重要的作用,同时增殖的胶质细胞具有对神经元细胞进行营养和保护的作用[7]。急性高血压性脑出血时机体的IGF-1的水平明显降低,可能与脑出血后脑组织对IGF-1的需求水平进一步增加,通过将外周的IGF-1运输到脑组织中,使脑组织中的IGF-1的水平明显增加,从而更有效的保护好神经的作用。本组研究还发现预后良好的高血压脑出血的患者IGF-1的水平明显高于预后不良的患者,说明IGF-1对脑出血的患者是一个重要的保护因素,也是预后的重要指标。
本组研究表明高血压性脑出血患者的HMGB-1和MIF水平明显高于脑出血组和高血压组,并且随着脑出血面积和神经损伤程度的增加而增加,说明HMGB-1和MIF水平参与了高血压脑出血的病理发生发展过程。HMGB-1是一种典型的非组蛋白,当脑出血时,HMGB-1释放到细胞外并介导炎性反应,参与多种炎性反应的过程[8]。在脑损伤的早期,HMGB-1能够引起小胶质细胞被激活,引起炎性反应和凋亡,而给HMGB-1抗体后可以一直小胶质细胞的激活,减少神经元的凋亡[9]。MIF可以活化机体中的多种细胞因子,加速斑块形成和脂质的堆积过程,促进脑血管病变的发生发展,使用MIF抗体可以降低机体的炎症。本组研究MIF水平与脑出血面积和神经损伤程度增加而增加,与文献报道[10]一致。本组研究还表明MIF和HMGB-1水平预后良好组明显低于预后不良组,说明MIF和HMGB-1是脑出血重要的预后因子,与文献报道MIF和HMGB-1是脑出血预后指标[11]相一致。故MIF和HMGB-1参与了脑出血疾病发生发展的过程,是脑出血预后的重要指标。
本组研究表明高血压性脑出血患者的GSN水平明显低于脑出血组和高血压组,并且随着脑出血面积和神经损伤程度的增加而降低,说明GNS是脑出血的保护指标。GNS主要功能是清除体内的激动蛋白,当组织损伤后,大量的肌动蛋白释放到血浆中,而迅速被GNS清除,从而降低肌动蛋白对机体的毒性反应,并且GNS能够与促炎因子和大量的生物活性结合,消除这些活性因子对机体的毒性反应,从而达到减少对机体的伤害[12]。在急性脑梗死、脑外伤和脑出血等急性脑损伤疾病中,GNS水平的浓度也显著下降,其下降程度与神经损伤程度和出血量呈负相关,并且与病情的预后具有明显的相关性[13]。本组研究表明GNS水平预后良好的脑出血患者明显高于预后不良的患者,说明GNS对高血压脑出血患者病情预测具有重要意义。在IGF-1、HMGB-1、GSN和MIF指标之间相关性分析,发现IGF-1与HMGB-1和MIF呈负相关,与GSN呈正相关;HMGB-1与GSN呈负相关,与MIF呈正相关,GSN与MIF呈负相关。说明IGF-1、HMGB-1、GSN和MIF指标参与了高血压性脑出血的发生发展过程,与患者的预后具有明显的相关性,故联合检测对于高血压脑出血的早期诊断和预后具有重要意义。
总之,IGF-1、HMGB-1、GSN和MIF参与了高血压性脑出血疾病的发生发展,对于判断高血压脑出血的病情和预后具有重要意义。
1钱松泉,南勇,李蓓蓓,等. 脑出血患者血浆高迁移率族蛋白B1浓度的检测及临床意义.放射免疫学杂志,2012,25:77-79.
2严永兴,梁丽贞,袁艳蓉,等. 脑出血模型大鼠脑组织胰岛素样生长因子-1表达的实验研究.浙江中西医结合杂志,2014:773-776.
3袁宁,许宏伟,刘学军. 湖南汉族人群巨噬细胞移动抑制因子-173G/C基因多态性及其与脑出血关系的研究.国际神经病学神经外科学杂志,2011,38:413-416.
4张俊,王雪芳,梅光伟,等. 脑出血患者血浆凝溶胶蛋白早期检测的临床价值.浙江医学,2014:775-777,812.
5陈宝友,李强,刘爱,等. 脑出血患者血清中一氧化氮、胰岛素样生长因子-1和巨噬细胞转移抑制因子的表达水平及意义.中国老年学杂志,2015:1750-1751.
6Wadowska M, Woods J, Rogozinska M, et al. Neuroprotective effects of enriched environment housing after transient global cerebral ischaemia are associated with the upregulation of insulin-like growth factor-1 signalling.Neuropathol Appl Neurobiol,2015,41:544-556.
7Aoi N, Nakayama T, Soma M, et al. The insulin-like growth factor-1 gene is associated with cerebral infarction in Japanese subjects.Hereditas,2012,149:153-162.
8Laird MD,Shields JS,Sukumari-Ramesh S,et al.High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4.Glia,2014,62:26-38.
9Watanabe M, Miyajima M, Nakajima M, et al. Expression analysis of high mobility group box-1 protein (HMGB-1) in the cerebral cortex, hippocampus, and cerebellum of the congenital hydrocephalus (H-Tx) rat.Acta Neurochir Suppl,2012,113:91-96.
10Chen G, Zheng M, Shu H, et al. Macrophage migration inhibitory factor reduces apoptosis in cerebral arteriovenous malformations.Neurosci Lett,2012,508:84-88.
11金涛,权天龙,李东波,等. 高迁移率族蛋白B1对急性自发性脑出血患者预后的影响.中国医药导报,2014,11:17-19.
12郭智东,王弋,张祖勇,等. 血浆凝溶胶蛋白浓度对重型颅脑损伤长期预后的预测价值.浙江中西医结合杂志,2014,24:100-103.
13朱慧艳,赵智晗,王宏. 急性脑梗死患者血浆凝溶胶蛋白水平的变化及其临床意义.实用临床医学,2015:8-11.
Significance of IGF-1, HMGB-1, GSN and MIF in patients with hypertensive intracerebral hemorrhage
WANGJing’e,CHENYan,GAOShan,etal.
DepartmentofNeurology,SouthCampusofTheSixthPeople’sHospitalAffiliatedtoShanghaiTrafficUniversity,CentralHospitalofFengxianDistrict,Shanghai201499,China
ObjectiveTo investigate the significance of serum levels of insulin-like growth factor (IGF)-1, high mobility group box-1 protein (HMGB-1), gelsolin (GSN) and macrophage migration inhibitory factor (MIF) in patients with hypertensive intracerebral hemorrhage.MethodsSeventy-eight patients with hypertensive intracerebral hemorrhage who were admitted and treated in our hospital from January 2013 to June 2015 were enrolled as hypertensive intracerebral hemorrhage group.These patients were divided into mild injury group (n=17), moderate injury group (n=36) and severe injury group (n=25) according to the severity of nerve function injury,moreover, according to cerebral hemorrhage volume,the patients were divided into three groups: small hemorrhage group (n=36),middle hemorrhage group (n=27) and massive hemorrhage group (n=15).In addition, according to Glasgow Outcome Scale these patients were divided into good prognosis group (n=43) and poor prognosis group (n=35).Besides the patients with simple intracerebral hemorrhage or simple hypertension who were treated in our hospital at the same period were divided into cerebral hemorrhage group (n=45) and hypertension group (n=35).The other 30 healthy subjects were served as control group. The serum levels of IGF-1,HMGB-1,GSN and MIF were detected in hypertensive intracerebral hemorrhage group,cerebral hemorrhage group,hypertension group and control group,and the correlation between the levels of IGF-1, HMGB-1, GSN MIF and neurologic impairment scores as well as cerebral hemorrhage area was analyzed, moreover the correlation between these indexes and patient’s prognosis and the correlation among the indexes were also analyzed.ResultsThe levels of IGF-1 and GSN in hypertensive intracerebral hemorrhage group were significantly lower than those in cerebral hemorrhage, hypertension group and control group (P<0.01), which in hypertension group or cerebral hemorrhage group were significantly lower than those in control group (P<0.01). However the levels of HMGB-1 and MIF in hypertensive intracerebral hemorrhage group were significantly higher than those in cerebral hemorrhage group, hypertension group and control group (P<0.01),which in hypertension group or cerebral hemorrhage group were significantly higher than those in control group (P<0.01).The levels of GSN and IGF-1
cerebral hemorrhage; hypertension; insulin-like growth factor-1; high mobility group box-1 protein; gelsolin; macrophage migration inhibitory factor
10.3969/j.issn.1002-7386.2016.18.003
201499上海交通大学附属第六人民医院南院
R 743.34
A
1002-7386(2016)18-2733-04
2016-04-06)

